Chapter 12 Balance and Coordination
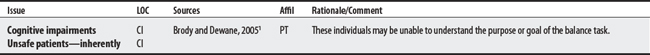
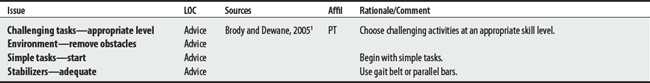
Balance exercises or training involves activities aimed at reducing instability/falls by improving patients’ ability to maintain their center of gravity within their support base. Because balance training aims to challenge stability, it is important to structure patient activities at the appropriate level and to screen patients who may be exceedingly unsafe for these activities1 (also see Screening for Falls, Chapter 4; Gait and Locomotion Training, Chapter 14).
12.2 Vestibular Exercises
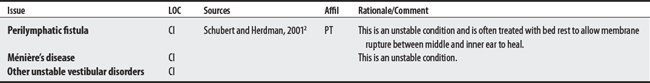
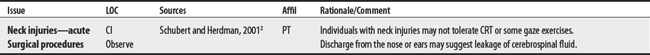
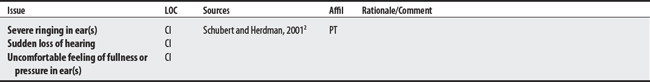
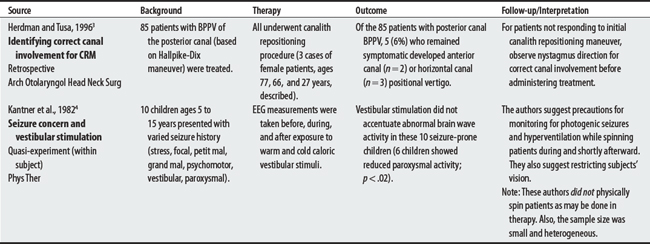
Vestibular rehabilitation aims at addressing disequilibrium and dizziness symptoms related to peripheral vestibular pathology by using specific exercises to improve balance and reduce dizziness.1 Unstable conditions listed below are CIs. For CRM, correct identification of semicircular canal involvement is necessary before treatment can be appropriately administered.
CONTRAINDICATIONS AND PRECAUTIONS
H60-H95 DISEASES OF THE EAR AND MASTOID PROCESS
S00-T98 INJURY, POISONING, AND CERTAIN OTHER CONSEQUENCES OF EXTERNAL CAUSES
1 Shumway-Cook A. Vestibular rehabilitation: What is vestibular rehabilitation? Available at: http://www.vestibular.org/rehab.html#rehabilitation. Accessed May 16, 2005
2 Schubert MC, Herdman SJ. Vestibular rehabilitation. In O’Sullivan SB, Schmitz TJ, editors: Physical rehabilitation: assessment and treatment, ed 4, Philadelphia: FA Davis, 2001.
3 Herdman SJ, Tusa RJ. Complications of the canalith repositioning procedure. Arch Otolaryngol Head Neck Surg. 1996;122(3):281-286.
4 Kantner RM, Clark DL, Atkinson J, Paulson G. Effects of vestibular stimulation in seizure-prone children. An EEG study. Phys Ther. 1982;62(1):16-21.
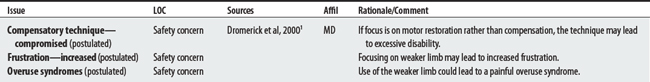
12.3 Constraint-Induced Movement Therapy (Acute Rehabilitation Setting)
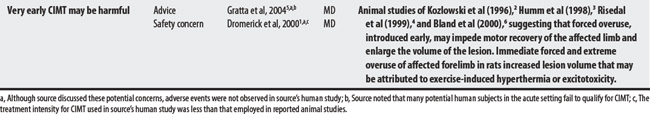
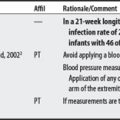
Constraint-induced movement therapy (CIMT, also called forced use) involves discouraging the use of the intact limb and encouraging active use of the hemiplegic one in order to maximize or restore function of the paralyzed upper limb.1 Some animal studies suggest that introducing CIMT too early (during acute rehabilitation) may be harmful (see Kozlowski,2 Humm,3 and Risedal’s4 animal studies.)
1 Dromerick AW, Edwards DF, Hahn M. Does the application of constraint-induced movement therapy during acute rehabilitation reduce arm impairment after ischemic stroke? Stroke. 2000;31:2984-2988.
2 Kozlowski DA, James DC, Schallert T. Use-dependent exaggeration of neuronal injury following unilateral sensorimotor cortex lesions. J Neurosci. 1996;16:4776-4786.
3 Humm JL, Kozlowski DA, James DC, et al. Use-dependent exacerbation of brain damage occurs during an early post-lesion vulnerable period. Brain Res. 1998;783:286-292.
4 Risedal A, Zeng J, Johansson BB. Early training may exacerbate brain damage after focal brain ischemia in the rat. J Cereb Blood Flow Metab. 1999;16:4776-4786.
5 Gratta JC, Noser EA, Ro T, et al. Constraint-induced movement therapy. Stroke. 2004;35(Suppl I):2699-2701.
6 Bland ST, Schallert T, Strong R, et al. Early exclusive use of the affected forelimb after moderate transient focal ischemia in rats: functional and anatomic outcome. Stroke. 2000;31:1144-1152.
12.4 Neurodevelopmental Treatment
OVERVIEW.
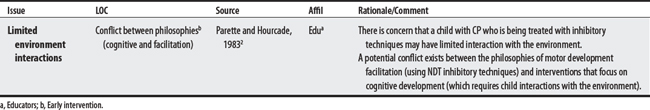
Neurodevelopmental treatment (NDT) is a neurological treatment approach that progresses individuals developmentally from a horizontal to a standing position. NDT has its roots in the reflex-based therapies of the 1950s, which relied heavily on the facilitation and inhibition of reflexes during treatment. The treatment is commonly administered to children with cerebral palsy.1 Parette and Hourcade2 raise a concern that this approach may limit a child’s interactions or experiences with the environment that are needed for cognitive development.
12.5 Proprioceptive Neuromuscular Facilitation
OVERVIEW.
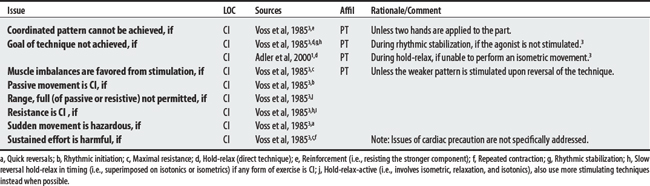
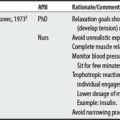
Proprioceptive neuromuscular facilitation (PNF) is a hands-on therapeutic exercise technique used to improve mobility, stability, stamina, coordination, and range of motion. The clinician typically facilitates a contraction with the muscles initially placed on maximal stretch (to provide afferent input) and then offers maximal graded resistance to recruit additional muscle activity while having the patient move through diagonal and spiral patterns of the body part. During a session, patients may be subjected to various forces including manual resistance, repeated stretches, joint compressions, and distractions.1
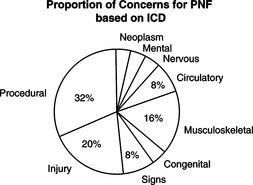
CONTRAINDICATIONS AND PRECAUTIONS
F00-F99 MENTAL AND BEHAVIORAL DISORDERS
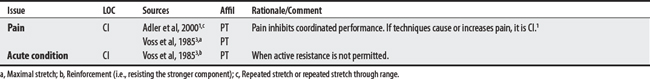
G00-G99 DISEASES OF THE NERVOUS SYSTEM
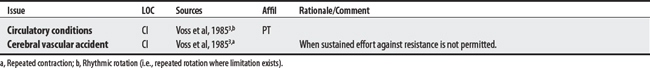
I00-I99 DISEASES OF THE CIRCULATORY SYSTEM
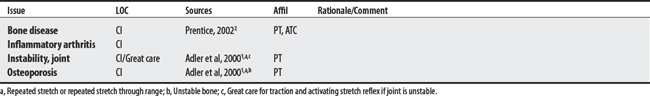
M00-M99 DISEASES OF THE MUSCULOSKELETAL SYSTEM AND CONNECTIVE TISSUE
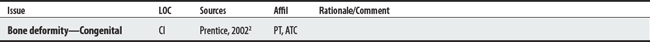
Q00-Q99 CONGENITAL MALFORMATIONS, DEFORMITIES, AND CHROMOSOMAL ABNORMALITIES
R00-R99 SYMPTOMS, SIGNS, AND ABNORMAL CLINICAL & LABORATORY FINDINGS (NOT ELSEWHERE CLASSIFIED)
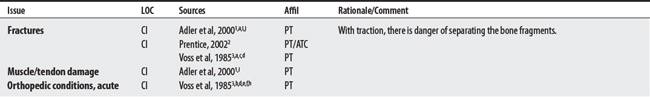
S00-T98 INJURY, POISONING, AND CERTAIN OTHER CONSEQUENCES OF EXTERNAL CAUSES
1 Adler SS, Beckers D, Buck M, et al. PNF in practice: An illustrated guide, ed 2. Berlin: Springer, 2000.
2 Prentice WE. Proprioceptive neuromuscular facilitation techniques. In: Prentice WE, editor. Therapeutic modalities for physical therapists. New York: McGraw-Hill, 2002.
3 Voss DE, Ionta MK, Myers BJ. Proprioceptive neuromuscular facilitation: patterns and techniques, ed 3. Philadelphia: Harper & Row, 1985.