6
Balance and Coordination
1. Define and contrast balance and coordination.
2. Discuss the mechanoreceptor system and define four mechanoreceptors.
3. List static and dynamic balance and coordination tests and activities.
4. Define proprioception and kinesthetic awareness.
5. Discuss several factors that contribute to balance dysfunction.
6. Identify functional closed kinetic chain proprioceptive exercises.
7. Discuss the rationale for proprioceptive training for the upper extremity.
DEFINITIONS OF BALANCE, PROPRIOCEPTION, NEUROMUSCULAR CONTROL, AND COORDINATION
Balance is often considered as the ability to maintain the center of mass (COM) over the base of support.12 This definition is only appropriate, however, when the base of support is fixed, such as standing in a constant location on two feet. The base of support is defined as the area contained within the parts of the body making physical contact with the external environment (Fig. 6-1).9 During dynamic situations, such as gait and functional activity, the base of support does not remain fixed to a constant location. Rather, as part of locomotion, the base of support moves, increasing the challenge to the elements responsible for maintaining balance. For this reason, the concept of balance also needs to include consideration to these circumstances. Postural equilibrium is a broader term that refers to balancing all forces acting on the body’s COM to maintain COM within the limits of stability with optimal joint segment alignment.1 Forces that challenge postural equilibrium arise from gravity, unexpected perturbations (i.e., stumbling over an unforeseen obstacle), or performance of voluntary motor activities (i.e., picking up a bag of groceries). Maintaining postural equilibrium is accomplished by the postural control system, the collection of sensory sources (somatosensory, vision, and vestibular), central nervous system, and the musculoskeletal system, all serving to maintain postural equilibrium. The somatosensory sources relevant to postural equilibrium are the mechanoreceptor populations residing in joint, muscle, connective, and ligamentous tissues. Because these tissues are often damaged during orthopedic injury, postural equilibrium may be disturbed following injury because of sensory disruptions, musculoskeletal disruptions, or both.9
Performing motor tasks effectively and efficiently requires not only postural equilibrium, but also effective coordination of the many muscles serving to move and stabilize the joints upon which they cross. Coordination has been defined as the ability to produce patterns of body and limb motions in the context of environmental objects and events.13 For example, picking up an object from a table requires coordinating the shoulder, elbow, and wrists joints to put the hand and fingers into position so the object can be grasped. Essential to coordinating joint positions is sufficient sensory (afferent) information regarding joint position, movement (kinesthesia), and movement resistance/tension. The afferent information contributing to these three elements, joint position, movement (kinesthesia), and movement resistance/tension, is referred to as proprioception.12 When the proprioception elements are consciously perceived, they are referred to as the conscious perceptions of proprioception.12 Proprioception is vital for neuromuscular control. From a joint stability perspective, neuromuscular control refers to the subconscious activation of muscles occurring in preparation for and in response to joint motion and loading.12
Mechanoreceptors
Mechanoreceptors are the sensory receptors that are responsible for converting mechanical events (e.g., movement, tension) into neural signals that can be conveyed to the central nervous system.7 As mentioned previously, mechanoreceptors are located in muscle, tendon, ligament, joint capsules, and in skin and connective (fascial) tissues. Each mechanoreceptor has specific stimuli (e.g., light touch versus tissue lengthening) and thresholds (e.g., magnitude of stimuli required) to which it will respond.6 Mechanoreceptors most susceptible to disruption during orthopedic injury include the receptors located in the musculotendinous, ligaments, and joint capsules. Mechanoreceptors located in the musculotendinous tissues include the muscle spindles and Golgi tendon organs. Muscle spindles are responsible for conveying information regarding muscle length and rate of length change. Unique to muscle spindles is their adjustable sensitivity via the gamma motor neurons. Golgi tendon organs, located across a musculotendinous junction are responsible for conveying information regarding muscle tension. Located in the ligaments and joint capsules are Ruffini receptors, Pacinian corpuscles, Golgi tendon-like endings and free nerve endings. Collectively, based on their threshold and adaptation characteristics, these four mechanoreceptors provide the central nervous system with information regarding speed of joint position and movement and host tissue load levels.
BALANCE AND COORDINATION TESTS
To prescribe appropriate balance and coordination exercises, it is essential to have data related to present balance and coordination status. Most often, coordination is evaluated by using the simple tests such as those outlined in Box 6-1. Although quantifying a patient’s coordination abilities can be easily accomplished by counting the number of repetitions completed in a given time frame or the number or percentage of successes per number of attempts, qualitatively examining and describing the patient’s abilities and difficulties (e.g., steadiness, control, speed) can also be useful.
Interestingly, balance tests and specific balance treatment activities are rarely separated, and the same movements are used for fundamental balance exercises and clinically relevant balance tests. Recall that three sensory sources, somatosensory, visual, and vestibular, contribute afferent information to the central nervous system so that appropriate muscle actions can be selected. By manipulating the conditions in which balance tasks are conducted, different aspects of the postural control system may be more selectively challenged.9 For example, having a patient stand with eyes closed heightens their reliance on somatosensory and vestibular information. In addition, manipulating the base of support and support surface characteristics can also change the challenge imposed upon the postural control system. For example, compared to double-leg stance, single-leg stance requires that the postural control system reorganize itself over a narrow and short base of support, with the additional advantage that bilateral comparisons can be made. Functionally, periods of single-leg stance are often interspersed in many activities of daily living, such as walking, turning, climbing stairs, and putting on a pair of pants. Further, during activities of daily living, one does not usually solely concentrate on maintaining balance, but rather on the details of the task (e.g., reaching up to remove the correct book from a shelf). Additionally, during activities of daily living, situations arise where unexpected challenges (perturbations) to postural equilibrium occur. Thus comprehensive balance assessment and training frequently call for a progressive battery of specific tasks of incremental difficulty and should include not only static stances with varying bases of support and support surface characteristics, but also tasks that involve voluntary movement and task completion and unexpected perturbations.9 Close observation of the patient’s protective reactions during loss of balance is a critical component of all balance tests and training activities. Immediate corrective action by the patient to maintain balance is necessary to move the patient from low-level balance activities to more challenging, complex maneuvers.
Box 6-2 summarizes common progressions used with respect to stances, support surfaces, and vision. For example, the static double-leg stance test with the eyes open is often the first test performed. This very simple test is made more challenging by having the patient maintain balance on both legs with his or her eyes closed. Next, the patient can then stand on a high-density foam surface with eyes open and closed, followed by standing on low-density foam with eyes open and closed. After that, the patient can stand on inclined or declined surfaces and unstable surfaces such as minitrampolines, rocker boards, and wobble boards, again using the eyes open to eyes closed progression. Similar eyes open to eyes closed and support surface progressions can be used with the patient using single-leg and tandem stances.
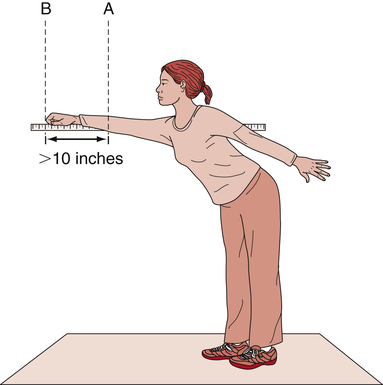
After a patient has mastered static stances under a variety of visual and support surface conditions, balance tasks can be progressed to include concurrent voluntary movements and tasks. Reaching tasks are very practical and functional test that determine a patient’s ability to perform simple daily tasks. Tests can be performed with the patient seated or standing using the upper or lower extremity (Fig. 6-2). Patients are offered a target that is slightly out of reach to test their ability to shift their center of mass to their limits of stability. Automatic activities, such as catching a ball, can also be performed in sequence from a seated to a standing position. The velocity, angle, and direction of throwing the ball to the patient challenges the patient’s ability to rapidly move arms and trunk out of static balance state, and back to equilibrium.
Quantifying performance during many of the previously mentioned tasks can be done using noninstrumented or instrumented measures. Noninstrumented measures include variables such as length of time in equilibrium,5,9 error scoring systems,10,11 and distances reached with arms or legs.1,8 During the dynamic tests, such as tandem walking (straight line, heel-to-toe sequencing), the distance traveled during a specified time period can be recorded. Instrumented measures often involve technology that record the forces exerted on a support surface (force platforms) or sensors that detect movement and position of the support surface. In addition to providing objective measures of balance performance, some also provide real time biofeedback to facilitate weight transfer within base of support boundaries.
As an additional objective measurement of static balancing abilities, Wolfson and associates14 designed the postural stress test (PST) to help quantify static balance. This test measures a patient’s ability to maintain balance during a series of progressive graded destabilizing forces. It is clinically cumbersome in that it involves applying a belt to the patient’s waist and attaching a weight-pulley system behind the patient. Without the patient’s knowledge, a weight is applied to the pulley system, which provides a sudden posterior force necessitating rapid correction of the postural interference. The test is graded on a scale from 0 to 9, with 0 representing a total inability to correct balance, and 9 representing no loss of balance. In addition to assessing a patient’s ability to withstand destabilizing perturbations, the PST may also serve as a training task.
BALANCE TRAINING IN ORTHOPEDICS
In concert with regaining strength and motion, specific functional tasks must be incorporated into the rehabilitation plan to accentuate muscular coordination, neuromuscular control, and postural equilibrium during dynamic activities. Duncan4 has identified several factors that may significantly contribute to balance dysfunction:
Specific Balance Tasks in Orthopedics
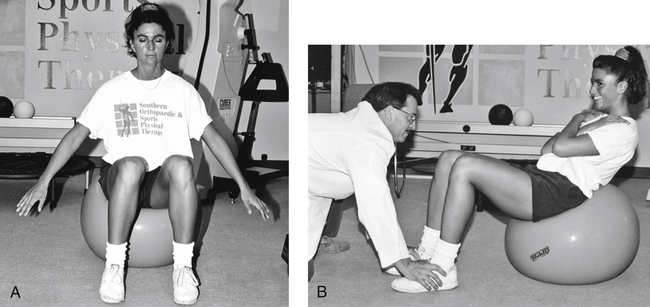
In cases of lower extremity injury with long-term, bedbound convalescence, manual resistive hip and knee extension with varying joint positions may be appropriate to initiate restoration of normal proprioceptive pathways. Once a patient may assume an upright position, progressive balance training may begin in a seated position. Similar progressive sequencing as with the standing tasks can be used, with the patient first attempting to maintain balance with the eyes open, then with the eyes closed. Progressions can include movements such as reaching tasks and the lifting of objects. Manually applied external forces (perturbations) can be applied while the patient’s eyes are closed to initiate reflexive balance training. Comparable to using foam and unstable surface for standing progressions, a large physioball or Swiss ball can be used as part of a seated static and dynamic balancing program to increase the challenge to the postural control system (Fig. 6-3, A). The physioball, which is a rather demanding exercise apparatus, has many applicable and creative uses in balancing and strengthening programs for various orthopedic patients. One very challenging exercise is the performance of support sit-ups on the physioball (Fig. 6-3, B). Obviously this particular exercise is for a rather active population, and not for all patients.
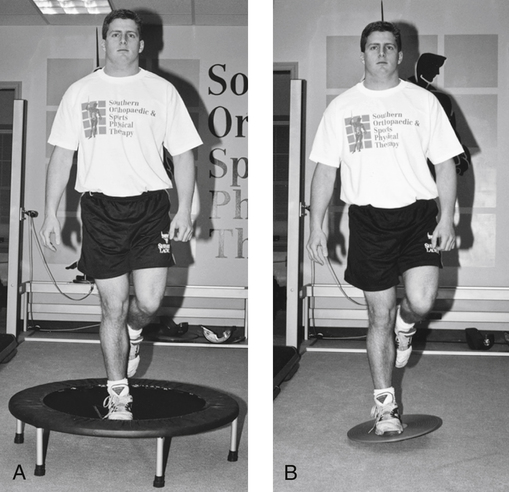
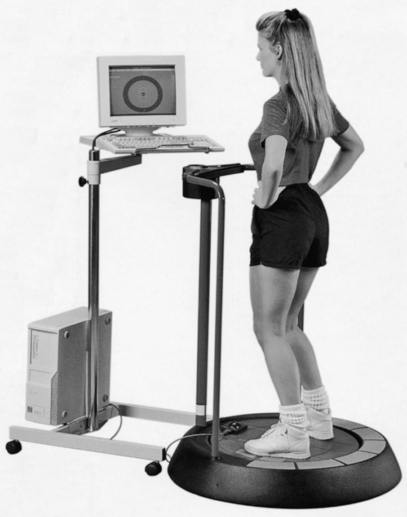
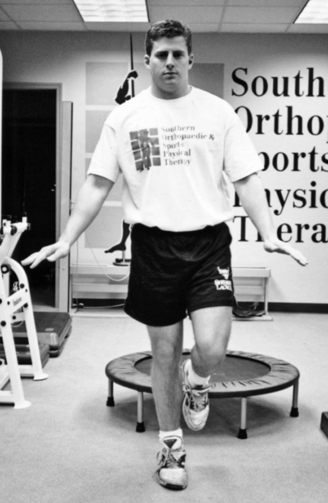
It is important that advanced functional balance drills, such as hopping, be included in the programs of patients returning to high levels of physical activity. Hopping drills can range from simple vertical leaps to quite challenging combinations of vertical and horizontal patterns. Hopping is useful with an athletic population and can be done on a flat, hard surface or on a minitrampoline (Fig. 6-4, A). The forgiving, uneven rebound surface of the minitrampoline adds an appropriate challenge for progressive balance training. Additionally, a wobble board (Fig. 6-4, B) or the kinesthetic ability trainer (Fig. 6-5) can be used to challenge single- or double-leg proprioception. Using the minitrampoline after hip, knee, or ankle injury for static standing balance and for single-leg or double-leg hopping is unique and challenging for many patients. As with other balance drills, single-leg or double-leg standing or hopping can progress from eyes open to eyes closed.
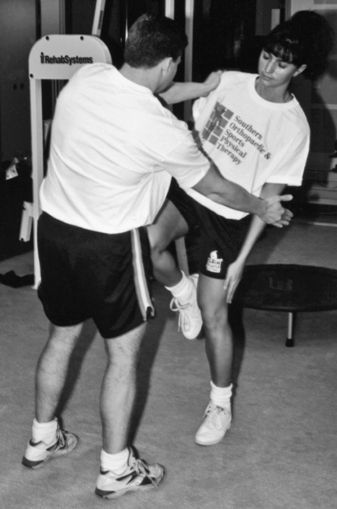
Inclusions of tasks in which sudden perturbations challenge balance are also important components of a balance training program. For example the clinician can apply sudden force to the patient while the patient is standing on one leg with the eyes closed (Fig. 6-6). Applying the manual postural stresses in different directions and with varying degrees of force can further challenge the ability to “right” or correct balance. Another method of perturbing balance is to use elastic tubing secured to a patient. The clinician begins the task by applying tension through the tubing. By suddenly releasing the tubing, the patient is suddenly presented with an immediate challenge to postural equilibrium.
Many commercial training devices have been developed to assist with balance training. Most commonly used is the biomechanical ankle platform system (BAPS). The name is misleading because this unit can be used for a wide variety of lower extremity conditions. The generic names for this tool are wobble board and balance board (Fig. 6-7). This device is very adaptable, portable, and affordable for many physical therapy environments. Initially, double-leg support progresses to single-leg standing. One of the most challenging balance drills is performing single-leg standing on a balance board with the eyes closed.
Balance and Proprioceptive Training for the Upper Extremity
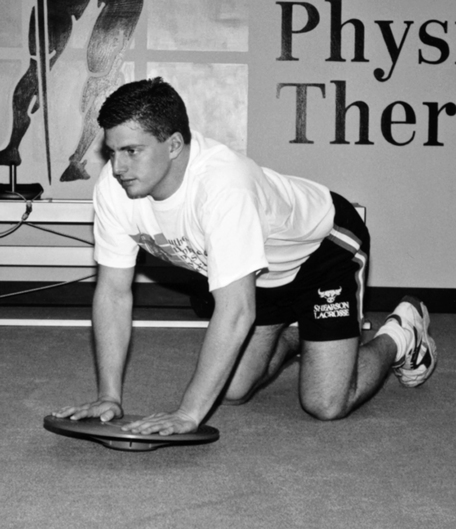
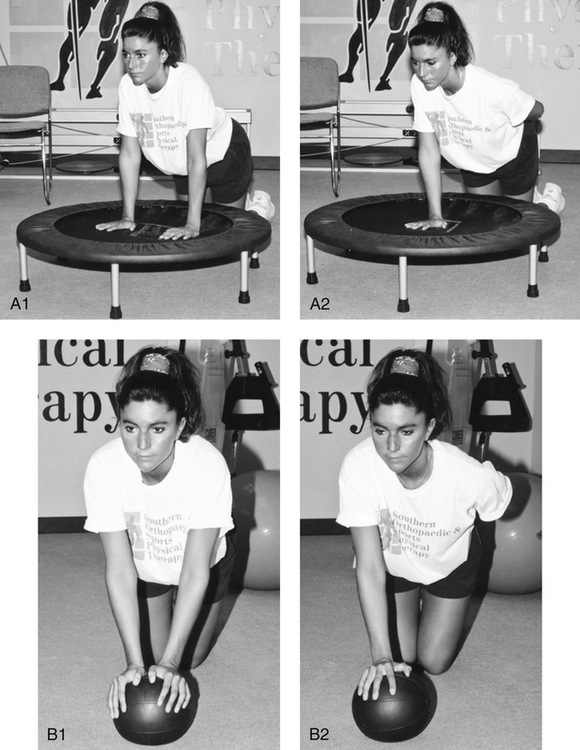
The upper extremities can be progressed in much the same way as the lower extremities. Although many of these exercises are often considered to be specific for an athletic population, they can be adapted to the general orthopedic population who must rely on dynamic vigorous weight-bearing shoulder and arm activities to accomplish tasks of daily living. With both arms in contact with the ground, weight shifting between the arms can be conducted on firm and unstable surfaces. In addition, while in a similar position, eyes open and eyes closed, balancing can be conducted on the same support surfaces used for standing balance (Figs. 6-7, 6-8, A1–A2). Beginning with two arms, this exercise can be intensified by having the patient use one arm with the eyes open and closed. Global stability of the glenohumeral joint can be enhanced effectively with the use of medicine balls and physioballs (Fig. 6-8, B1–B2). The patient begins the progression of this exercise by kneeling in front of the ball and placing both hands on the ball. As the exercise progresses, extraordinary joint stability, strength, and balance are required to maintain equilibrium.
Summary
GLOSSARY
Balance The ability to maintain the center of mass (COM) over the base of support.12
Base of support The area contained within the parts of the body making physical contact with the external environment.9
Coordination The ability to produce patterns of body and limb motions in the context of environmental objects and events.13
Golgi tendon organs Fibers responsible for conveying information regarding muscle tension.
Mechanoreceptors Sensory receptors responsible for converting mechanical events into neural signals that can be conveyed to the central nervous system.7
Neuromuscular control Subconscious activation of muscles occurring in preparation for and in response to joint motion and loading.12
Postural equilibrium The balance of all forces acting on the body’s COM to maintain it within the limits of stability with optimal joint segment alignment.1