Balance
What is balance?
• Postural equilibrium/stability involving the coordination of movement strategies to:
• Maintain an upright posture against gravity and any other external forces
• Maintain the COM within the stability limits of the BOS during internally and externally initiated movement (planned/intentional and unpredictable).
• Postural orientation involving the control of body segment alignment with respect to:
Sensory input and balance
The state of balance is maintained through complex postural control mechanisms which are reliant on adequate sensory input. The principal input systems to balance are the vestibular system (S2.10), the visual system (S2.10) and the somatosensory systems (S3.23) (Massion et al. 2004). Visual input provides a reference for upright vertical but is also essential in predicting forthcoming threats to balance from the environment. The somatosensory system, primarily proprioception, provides a reference for the body’s position in relation to the supporting surface and to other body parts and finally the vestibular system provides a reference for head position and movement of the head in relation to gravity.
In general this sensory input has two main functions:
Sensory feed forward which allows a preparation for movement. These anticipatory adjustments require input from both the internal and external environment and are an integral part of every movement. They are strongly linked to previous experiences.
Sensory feedback which allows ongoing regulation and appropriate muscle adjustments to be made in response to planned and unplanned displacement of the COM during movement.
Integration
Integration of this sensory information for an appropriate motor response is facilitated by various higher centres, including: the brain stem and cranial nerves (S2.10); the cerebellum (S2.12); reticular formation (S2.10) and the cerebral cortex (S2.7). The amount of cognitive processing by the cortex for postural control is usually minimal, with its contribution depending on the complexity of the task and the capability of the individual’s postural control system. For example, postural control relies on accurate sensory input, but also on the ability of the central nervous system (CNS) to attend to the relevant sensory cues and to prioritize or weight the input according to its relevance to the context and task (Horak 2006). The CNS also intervenes if a sensory conflict exists when it must weight the sources and reject the potential source of error (Karnath et al. 2000b).
Motor output and balance
During movement there is inevitably a displacement of the COM in relation to the BOS. This occurs whether the movement involves the trunk, the upper limb, the lower limb, turning the head or simply breathing. What determines whether the displacement leads to a fall is the motor response by which balance is recovered. These motor adjustments are flexible and varied and dependent on the task, the environmental context and the individual. An appropriate motor response requires a certain level of muscle strength, endurance and an available range of movement (Cholewicki et al. 1997; Ebenbichler and Oddsson 2001; Hodges and Richardson 1997) but also fine grading of agonists, antagonists and synergistic muscles, appropriate co-contraction and a high level of reciprocal innervation.
Movement strategies
An individual can slow down the displacement of the COM by rapidly generating muscle torque at the ankles, hips or other joints around a fixed BOS. For anteroposterior displacements of the COM the predominant torque is generated via an ankle strategy (Fig. 32.1) although a hip strategy (Fig. 32.2) may also be present. For a mediolateral displacement, the hip strategy is dominant (Maki and McIlroy 2006). These strategies occur in a feed forward manner to maintain balance and are continuously interchangeable during movement. However, if the perturbation is large and these strategies are unsuccessful, the individual may actually change the BOS by stepping (Fig. 32.3) or using an outstretched arm. Although the latter response is often referred to as protective it can also occur during small perturbations as a normal strategy for balance.
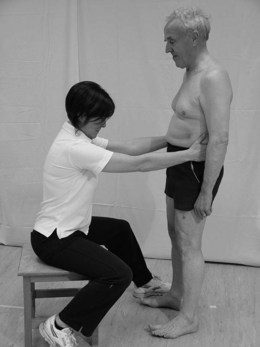
Figure 32.1 Movement strategy: Ankle.

Figure 32.2 Movement strategy: Hip.

Figure 32.3 Movement strategy: Step backwards.
Balance reactions
Equilibrium reactions
These are subtle changes in muscle tone required to maintain equilibrium and are analogous with postural sway (Fig. 32.4). When people stand with their eyes closed, postural sway may increase by 20–70% (Lord and Menz 2000).
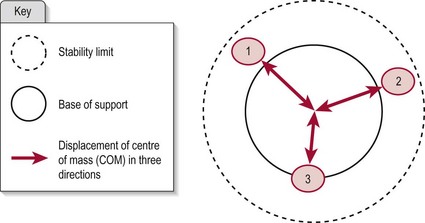
Figure 32.4 Equilibrium reactions.
Righting reactions
Righting reactions occur in response to displacement of the COM beyond the stability limits in an attempt to regain equilibrium. They are a basic component in maintaining equilibrium while changing between positions and hence during movement. Righting reactions may involve the head (moving on the trunk to maintain the head in vertical), the trunk (in response to weight transfer or head/limb movement) or limb movement (acting as a counter balance to offset the displacement of COM) (Fig. 32.5).
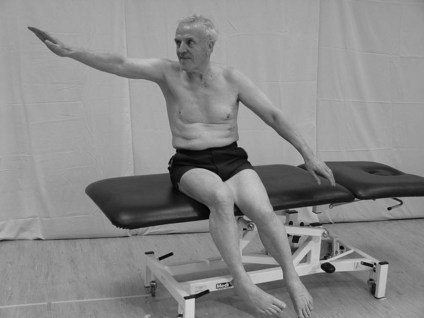
Figure 32.5 Righting reactions in sitting.
Why do we need to assess balance?
Balance impairments have been shown to increase the risk of falls (S3.34) resulting in high economic costs and social problems (Lamb et al. 2003; Harris et al. 2005; Belgen et al. 2006). Balance problems in neurologically impaired patients are common, being associated with the following impairments:
Motor dysfunction
Biomechanics
• Reduced stability limits: In CVA (De Haart et al. 2004) and in Parkinson’s disease (PD) (Mancini et al. 2008)
• Reduced balance response (magnitude and velocity): In PD (Mancini et al. 2008)
• Altered movement strategies: In CVA there is a reliance on hip and stepping strategies which are less efficient in terms of stability (Maki and McIlroy 1997; Chen et al. 2000).
Sensory dysfunction
Altered sensory integration
• Difficulty dividing attention between two tasks (Stapleton et al. 2001)
• Impaired ability to use sensory weighting: Reduced speed of integration in PD (Brown et al. 2006; De Nunzio et al. 2007). In CVA there is often excessive reliance on visual input which may lead to inappropriate postural adjustments (Bonan et al. 2004)
• Delayed or inadequate anticipatory response: In CVA and PD (Horak et al. 1997)
• Altered perceived stability limits: In CVA (De Haart et al. 2004) linked to anxiety and lack of confidence
• Abnormal perception of vertical via the somatosensory systems in CVA, particularly in association with visuospatial neglect (Yelnik et al. 2002; Bonan et al. 2006).
How do I assess balance?
Functional observation
Therapist
1. The therapist should set an appropriate balance task. When setting a task the therapist should consider the following:
a. Create a safe situation (environment, assistance as required).
b. Incorporate various environmental contexts and various tasks as our postural control is highly specific to both.
c. Challenge their balance: This means making them unstable and could be achieved by:
2. Observe the patient performing the balance task.
Can they balance (maintain the COM within the BOS) in a specific posture? Instability during a stable posture may indicate a severe balance deficit. If there is inappropriate excessive sway in all postures with eyes open, then sufficient assistance is recommended before challenging the patient any further.
Can they balance during movement? If not, do they fall?
If they can balance, what strategies do they use to achieve balance? Are their responses appropriate for the amount of COM displacement?
Does the patient use compensatory strategies to maintain balance? Using trunk or limb muscles to fix is inefficient and may indicate underlying instability. Visual fixation is also common.
Are these compensations effective?
Is the goal completed successfully? Without a stable/balanced base the execution may be unsuccessful.
Is the task performance effortful? This may indicate extra muscle work to hide poor balance.
Do they interact with their BOS during the movement? The BOS should act as a point of reference for movement. The base providing a stable point that the patient can move around confidently.
What happens to the balance if sensory input is reduced (e.g. eyes closed)?
Analysis
Postural control is hugely complex and therefore simple balance measures are unlikely to identify the specific deficits of the sensorimotor processes. Comprehensive assessment is required to evaluate the potential impairments implicated in a deficit of balance. Therefore the findings from your balance assessment must be considered in conjunction with the findings from other assessment tools (S3.19–34). Particular attention should be paid to vision (S3.27) and sensory testing (S3.23) and if a lesion of the vestibular system is suspected, referral to a specialist unit is advised. However, trunk stability, muscle tone, alignment, pain, strength, range of movement and cognition/perception may also be linked to reduced balance.
Outcome measures
Research
Posturography refers to any technique used to quantify postural control in standing. These objective quantitative measures of balance can assess with greater sensitivity than observation by the therapist (De Oliveira 2008). Postural reactions can be quantified on force platforms with the sensory environment being manipulated to challenge different systems of balance. However, the output from a force platform does not tell the therapist about the quality of the postural control mechanisms.
Clinical
• Functional activities: validated in stroke (Tyson and DeSouza 2004)
• Sitting: supported sitting balance, sitting arm raise, sitting forward reach
• Standing: supported standing balance, standing arm raise, standing forward reach, static tandem standing, weight shift
• Walking: timed 5-m walk with and without an aid, tap and step.
References and Further Reading
Au-Yeung, SS, Ng, JT, Lo, SK. Does balance or motor impairment of limbs discriminate the ambulatory status of stroke survivors? American Journal of Physical Medicine and Rehabilitation. 2003; 824:279–283.
Belgen, B, Beninato, M, Sullivan, PE, et al. The association of balance capacity and falls self-efficacy with history of falling in community-dwelling people with chronic stroke. Archives of Physical Medicine and Rehabilitation. 2006; 874:554–561.
Bonan, IV, Colle, FM, Guichard, JP, et al. Reliance on visual information after stroke, Part I: Balance on dynamic posturography. Archives of Physical Medicine Rehabilitation. 2004; 852:268–273.
Bonan, IV, Guettard, E, Leman, MC. Subjective visual vertical perception relates to balance in acute stroke. Archives of Physical Medicine Rehabilitation. 2006; 875:642–646.
Brown, LA, Sleik, RJ, Winder, TR. Attentional demands for static postural control after stroke. Archives of Physical Medicine Rehabilitation. 2002; 8312:1732–1735.
Brown, LA, Cooper, SA, Doan, JB, et al. Parkinsonian deficits in sensory integration for postural control: temporal response to changes in visual input. Parkinsonism Related Disorders. 2006; 12:376–381.
Chen, IC, Cheng, PT, Hu, AL, et al. Balance evaluation in hemiplegic stroke patients. Chan Gung Medical. 2000; J236:339–347.
Cholewicki, J, Panjabi, M, Khachatryan, A. Stabilizing function of trunk flexor and extensor muscles around a neutral spine posture. Spine. 1997; 22:2207–2212.
Danells, CJ, Black, SE, Gladstone, DJ, et al. Poststroke ‘pushing’: Natural history and relationship to motor and functional recovery. Stroke. 2004; 3512:2873–2878.
De Haart, M, Geurts, AC, Huidekoper, SC, et al. Recovery of standing balance in postacute stroke patients: a rehabilitation cohort study. Archives of Physical Medicine Rehabilitation. 2004; 856:886–895.
De Nunzio, AM, Nardone, A, Schieppati, M. The control of equilibrium in Parkinson’s disease patients: delayed adaptation of balancing strategy to shifts in sensory set during a dynamic task. Brain Research Bulletin. 2007; 74:258–270.
De Oliveira, CB, de Medeiros, IR, Frota, NA, et al. Balance control in hemiparetic stroke patients: main tools for evaluation. Journal of Rehabilitation Research and Development. 2008; 468:1216–1228.
Ebenbichler, G, Oddsson, L. Sensory-motor control of the lower back: implications for rehabilitation. Medicine and Science in Sports and Exercise. 2001; 33:1889–1898.
Garland, SJ, Ivanova, TD, Mochizuki, G. Recovery of standing balance and health-related quality of life after mild or moderately severe stroke. Archives of Physical Medicine Rehabilitation. 2007; 882:218–227.
Gustafson, Y. Falls and injuries after stroke: time for action!. Stroke. 2003; 342:494–501.
Harris, JE, Eng, JJ, Marigold, DS, et al. Relationship of balance and mobility to fall incidence in people with chronic stroke. Physical Therapy. 2005; 852:150–158.
Hodges, P, Richardson, C. Relationship between limb movement speed and associated contraction of the trunk muscles. Ergonomics. 1997; 40:1220–1230.
Horak, FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing. 2006; 35(Suppl 2):7–11.
Horak, FB, Henry, SM, Shumway-Cook, A. Postural perturbations: new insights for treatment of balance disorders. Physical Therapy. 1997; 775:517–533.
Karnath, HO, Broetz, D. Understanding and treating ‘pusher syndrome’. Physical Therapy. 2003; 8312:1119–1125.
Karnath, HO, Ferber, S, Dichgans, J. The origin of contraversive pushing: evidence for a second graviceptive system in humans. Neurology. 2000; 559:1298–1304.
Karnath, HO, Ferber, S, Dichgans, J. The neural representation of postural control in humans. Proceedings of the National Academy of Science USA. 2000; 9725:13931–13936.
Karatas, M, Cetin, N, Bayramoglu, M, et al. Trunk muscle strength in relation to balance and functional disability in unihemispheric stroke patients. American Journal of Physical Medicine and Rehabilitation. 2004; 832:81–87.
Lamb, SE, Ferrucci, L, Volapto, S, et al. Risk factors for falling in home-dwelling older women with stroke: the Women’s Health and Aging Study. Stroke. 2003; 342:494–501.
Lord, SR, Menz, HB. Visual contributions to postural stability in older adults. Gerontology. 2000; 46:306–310.
Maki, BE, McIlroy, WE. The role of limb movements in maintaining upright stance: the ‘change-in-support’ strategy. Physical Therapy. 1997; 775:488–507.
Maki, BE, McIlroy, WE. Control of rapid limb movements for balance recovery: age-related changes and implications for fall prevention. Age and Ageing. 2006; 35-S2:12–18.
Mancini, M, Rocchi, L, Horak, FB, et al. Effects of Parkinson’s disease and levodopa on functional limits of stability. Clinical Biomechanics. 2008; 23:450–458.
Massion, J, Alexandrov, A, Frolov, A. Why and how are posture and movement coordinated? Progress in Brain Research. 2004; 1432:13–27.
Niam, S, Cheung, W, Sullivan, PE, et al. Balance and physical impairments after stroke. Archives of Physical Medicine Rehabilitation. 1999; 80(10):1227–1233.
Oie, KS, Kiemel, T, Jeka, JJ. Multisensory fusion: simultaneous re-weighting of vision and touch for the control of human posture. Brain Research Cognitive Brain Research. 2002; 141:164–176.
Oxford Dictionary. Online www.askoxford.com/?view=uk.
Peterka, JR. Sensorimotor integration in human postural control. Journal of Neurophysiology. 2002; 883:1097–1118.
Peterka, RJ, Loughlin, PJ. Dynamic regulation of sensorimotor integration in human postural control. Journal of Neurophysiology. 2004; 911:410–423.
Stapleton, T, Ashburn, A, Stack, E. A pilot study of attention deficits balance control and falls in the acute stage following stroke. Clinical Rehabilitation. 2001; 15:437–444.
Stokes, M. Physical management in neurological rehabilitation, ed 2. Edinburgh: Elsevier/Mosby; 2004.
Tyson, SF, DeSouza, LH. Reliability and validity of functional balance tests post stroke. Clinical Rehabilitation. 2004; 188:916–923.
Tyson, SF, Hanley, M, Chillala, J, et al. Balance disability after stroke. Physical Therapy. 2006; 861:30–38.
Vaugoyeau, M, Viel, S, Assaiante, C, et al. Impaired vertical postural control and proprioceptive integration deficits in Parkinson’s disease. Neuroscience. 2007; 146:852–863.
Verheyden, G, Vereeck, L, Truijen, S, et al. Trunk performance after stroke and the relationship with balance gait and functional ability. Clinical Rehabilitation. 2006; 205:451–458.
Yelnik, AP, Lebreton, FO, Bonan, IV, et al. Perception of verticality after recent cerebral hemispheric stroke. Stroke. 2002; 339:2247–2253.





