Chapter 10 Bacterial Overgrowth of the Small Intestine Breath Test
 Introduction
Introduction
Small intestinal bacterial overgrowth (SIBO) is an abnormal colonization within the small bowel by bacteria normally found in the colon, mouth, or pharynx.1 Also called bacterial overgrowth of the small intestine (BOSI), “blind-loop,” or “stagnant loop,”2 SIBO is a potentially serious disorder that leads to problems such as malabsorption, anemia and weight loss, malnutrition,3 increased intestinal permeability, and bone loss.4 Breath testing for hydrogen (H2) and methane (CH4) provides a simple noninvasive means of detecting SIBO. Once SIBO has been identified, antimicrobials are typically administered to eradicate the bacteria. Subsequent attention to underlying causes is also essential in preventing recurrence.
Frequency of Small Intestinal Bacterial Overgrowth
Bacterial overgrowth of the small intestine is an overlooked contributing factor in several common disorders.5 Several studies, for example, demonstrated the presence of SIBO in patients with irritable bowel syndrome (IBS).6 In one such study, in which 84% of IBS patients tested positive for SIBO (vs 20% of healthy controls), successful eradication of SIBO led to a 75% improvement (compared with a 36.7% improvement in those with incomplete eradication, and an 11% improvement in participants receiving placebo).7 SIBO has also been observed in patients with chronic fatigue syndrome8 and/or fibromyalgia.9 SIBO tends to increase intestinal permeability (aka “leaky gut”).10 Investigators who found leaky gut in 37.5% of patients with fibromyalgia suggested exposure of immune cells to luminal antigens and consequent immune modulation as a likely mechanism for the pain syndrome.11 A variety of anatomic and motor disorders of the small bowel can lead to SIBO, including surgical loops, diverticula, strictures, adhesions, tumors, fistulas,2 scleroderma,12 intestinal pseudoobstruction,13 and diabetic enteropathy.14 Jejunal diverticulosis5 and Crohn’s disease15 have both been associated with SIBO, particularly in patients with previous intestinal surgery. Although the concentration of bacteria normally increases exponentially toward the distal end of the small intestine,2 far fewer bacteria inhabit the small intestine than the colon.16 A common feature of most of these disorders is stasis of small bowel contents, which allows bacterial concentrations to increasingly resemble those of the large intestine (Box 10-1).16,17 Although many of the bacteria found in SIBO are beneficial within the colon, these same microorganisms can have deleterious effects within the delicate environment of the small intestine.
BOX 10-1 Causes of Small Intestinal Bacterial Overgrowth
• Achlorhydria, hypochlorhydria, drug-induced hypoacidity
• Stasis resulting from structural changes (e.g., diverticulosis, blind loops, radiation damage, stricture, fistulas, intestinal pseudoobstruction, adhesions resulting from prior surgery)
• Chronic pancreatic insufficiency
• Disaccharidase deficiencies (lactase)
• Immunodeficiency (especially of secretory immunoglobulin A)
Interestingly, many patients with celiac disease whose symptoms persist despite a gluten-free diet have been shown to have SIBO, with improvement only after bacterial eradication.18 The incidence of SIBO also increases with age.19 It has been found that 64% of individuals more than 75 years of age with chronic diarrhea have colonic-type flora in their small bowels5 and that SIBO is the most common cause of clinically significant malabsorption in elderly persons.2
Pathophysiology
Two major factors control the numbers and types of bacteria within the small bowel: intestinal peristalsis and gastric acid secretion.2,16 Accordingly, SIBO has been associated with both intestinal stasis and hypochlorhydria.17 Other factors that influence SIBO include pancreatic enzyme secretion,20 disaccharidase production by microvilli,21 ileocecal valve function,22 bile salts, luminal pH, and oxidation-reduction potential.16
For SIBO to produce clinical consequences, an adequate concentration of organisms with particular metabolic properties within specific locations of the small intestine is required. For example, a heavy concentration of strict anaerobes and coliforms in the proximal small intestine is more likely to be associated with malabsorption than a flora consisting of fewer strict anaerobes or coliforms or when strict anaerobes or coliforms are located in the distal small intestine.16 For this reason, SIBO may be asymptomatic in some individuals yet produce signs and symptoms in others. Box 10-2 outlines clinical signs and symptoms that alert the practitioner to consider testing for SIBO.
BOX 10-2 When to Consider Breath Testing for Small Intestinal Bacterial Overgrowth
• Gas, bloating, or diarrhea, usually after eating
• Chronic hypochlorhydria or achlorhydria
• Use of acid-blocking medications
• Prior intestinal surgery, chronic constipation, or other causes of intestinal stasis
• Intolerance of disaccharides (lactose)
• Unexplained vitamin B12 deficiency, weight loss, or bone loss
• Unexplained nutrient insufficiencies (e.g., calcium, magnesium, fat-soluble vitamins)
Diagnosis
Signs and Symptoms
The classic SIBO syndrome is characterized by megaloblastic anemia resulting from vitamin B12 deficiency and weight loss and diarrhea secondary to fat malabsorption.16 However, many patients present with nonspecific symptoms 1 to 2 hours after a meal, including bloating, flatulence, and abdominal pain resulting from bacterial fermentation of intraluminal sugars and associated gas production (Box 10-3).8,18
Via secretory and osmotic processes, diarrhea may occur even in the absence of significant steatorrhea. Unabsorbed fats and bile salts are modified by bacteria in the colon to hydroxylated fats and free bile acids, respectively, which stimulate colonic secretion of water and electrolytes.16
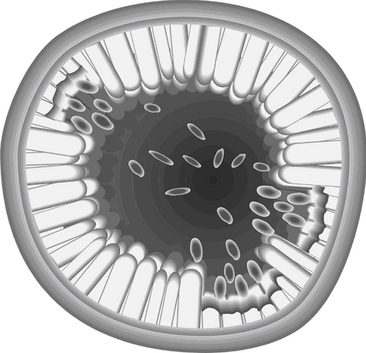
Bile salts, essential to fat emulsification and assimilation, must be conjugated with taurine or glycine to function properly. In SIBO, bacteria in the proximal small intestine deconjugate bile salts to form free bile acids.16 This can have two major clinical repercussions: (1) free bile acids can promote mucosal damage (Figure 10-1), resulting in reduced brush-border enzyme activities (especially lactase),23 defects in mucosal uptake of sugars and amino acids, enteric blood loss, and protein-losing enteropathy; or (2) the conjugated bile salt concentration may fall below the concentration necessary for effective micelle formation, resulting in fat malabsorption, steatorrhea,16,17 and deficiencies of fat-soluble vitamins.3
Fat malabsorption in SIBO can also result from mechanical interference, specifically formation of a pseudomembrane, thought to represent a maladaptive defense mechanism against the bacterial overgrowth.24
Unabsorbed fatty acids can form insoluble soaps with calcium and magnesium, rendering them unavailable.3 Osteomalacia, night blindness, hypocalcemic tetany,2 or metabolic bone disease4 may develop as a consequence of lipid malabsorption in patients with SIBO. Although rare, iron deficiency anemia may result from blood loss.3
SIBO may also lead to vitamin B12 deficiency, with megaloblastic anemia and low serum cobalamin levels.2,16 Although intrinsic factor is not altered by anaerobic bacteria, microbes are capable of detaching vitamin B12 from the intrinsic factor, as well as directly using B12.22 Either mechanism has the effect of making the vitamin unavailable. Paradoxically, serum folate values are usually normal or even elevated in SIBO, a result of bacterial synthesis of the vitamin.25
Hypoproteinemia may also occur in SIBO, secondary to protein-losing enteropathy and protein malabsorption.3,17 In addition, bacteria may metabolize proteins to ammonia and fatty acids, thereby rendering them unavailable to the host.23
 Laboratory Assessment
Laboratory Assessment
The composition of bacterial populations contaminating the small bowel is complex and variable.2 However, the diagnosis of SIBO tends to be oriented less to the identification of specific microorganisms and more to overall bacterial concentrations.2
Endoscopy
Culture of a small bowel aspirate via endoscopy is a direct method for diagnosing SIBO; abnormally high bacterial counts confirm the diagnosis.17 This method offers good sensitivity but low specificity. Because the aspirate is typically taken from only one location, SIBO in the more distal end of the small bowel or concentrated in a large diverticulum or blind loop may be missed.26 Intubation methods are invasive, time consuming, uncomfortable, and expensive.
Breath Testing
Breath tests were devised as less invasive alternatives to intubation and culture, offering greater patient comfort and convenience. They also offer good sensitivity27; a meta-analysis suggested that lactulose breath testing identifies SIBO in approximately 54% of IBS patients compared with only 4% of patients via jejunal aspirate and culture.28
Breath tests are based on the ability of intestinal microbes to ferment carbohydrates, producing H2 or CH4 in the process. A fraction of these gases naturally diffuse from the bowel to the circulation and are excreted with expired air. Because there is no other metabolic source of H2 and CH4, pulmonary excretion of these gases is used as a measure of bacterial fermentation during the passage through the bowel.29
A lactulose breath test is commonly employed to diagnose SIBO. Typically, patients ingest a challenge dose of lactulose (a synthetic, nonabsorbed disaccharide) after two days of fiber restriction and a 12-hour fast.30 Glucose has also been used as a challenge agent, although its rapid absorption reduces the test’s sensitivity in the distal ileum27 and the agent is not suitable for patients with blood sugar disorders such as diabetes. In all cases, intestinal bacteria modify the challenge substance, producing an early peak in breath gas values in patients with SIBO. In the case of lactulose, which offers the advantage of traveling the full length of the small intestine, the early H2 and CH4 peak is typically followed by a prolonged peak representing colonic bacterial activity (approximately 90 minutes into the collection process).27,31
Hydrogen Versus Methane
Many studies using carbohydrate challenges have measured only breath H2. However, 30% to 50% of H2 producers also produce CH4,32 most likely a result of “methanogenic” bacteria, which consume H2, producing CH4 in the process.30 Individuals whose intestines harbor methanogenic bacteria typically produce greater amounts of breath CH4 during the test, thus being potentially missed on a test examining only H2.33
Clinical correlations have been noted between various disorders and the production of H2 versus CH4. In one study, individuals producing higher amounts of H2 relative to CH4 reported significantly increased bloating and cramping after carbohydrate ingestion, whereas individuals producing high CH4 reported no significant increase in these symptoms.34 Specific IBS symptoms also vary with breath gas values. For example, CH4 production has been associated with constipation-predominant IBS, whereas H2 production has been associated with diarrhea.35 SIBO, in general, appears to be more common in diarrhea-predominant IBS than in constipation-predominant IBS.28
Interpretation
Lactulose is normally not fermented until it reaches the colon. As a result, the typical fasting breath sample contains less than 20 ppm of H2 or CH4. An increase in breath gas levels in the later breath specimens (90 and 120 minutes) usually reflects colonic bacterial fermentation and is considered normal. Lack of the expected colonic peak can result from antibiotics or an acidic colonic pH.36,37 In patients with SIBO, the lactulose is fermented in the small intestine, resulting in an early peak in breath gas values.27
A positive test result (indicating SIBO) is defined by either (1) the presence of a total H2 and CH4 gas peak more than 15 ppm above baseline levels, occurring less than 90 minutes after lactulose ingestion, or (2) an elevated baseline (fasting) breath gas concentration, even if there is no large increase from baseline over the next few samples.38 Elevated baseline values occur in up to one-third of patients with SIBO36 and are thought to relate to the fermentation of endogenous brush-border glycoproteins.39
False-Positive and False-Negative Results
False-Positive Results
The following factors may account for a false-positive result on a breath test:
• Failure to fast for at least 12 hours before the test or to avoid dietary fiber the day before collection can result in excessive “background noise” that contributes to the overall concentration of breath gases.29
• Sleeping, smoking, or eating shortly before or during sample collection can increase concentrations of breath gases.40
• Fermentation by oropharyngeal flora can lead to early, transient elevations in breath gases after carbohydrate ingestion.41 As a result, teeth and tongue brushing before specimen collection is recommended.
False-Negative Results
False-positive results on a breath test can be caused by the following factors:
• Diarrhea or the recent administration of antimicrobials can temporarily reduce the concentration of gut bacteria,42 thus obscuring SIBO. Laxatives and enemas pose a similar risk.43 Patients are advised to wait at least 1 week after antibiotic therapy before performing the test.
• SIBO confined to the distal ileum may go undetected if the breath gas peak produced in the ileum merges with the breath gases produced by the colonic flora.27
• Rapid intestinal transit may cause delayed increases in breath gases, leading to a rise only after the lactulose has already reached the cecum.44 This is particularly relevant for patients with SIBO who have undergone small bowel resection.
 Treatment of Bacterial Overgrowth
Treatment of Bacterial Overgrowth
Bacterial Eradication
Unfortunately, addressing only the contributing factors to SIBO usually fails to reverse it; therefore, the primary treatment of SIBO is directed at altering the intestinal flora with antimicrobials.17 Conversely, investigation and treatment of the root cause is necessary to prevent chronic recurrence of SIBO.
Most patients with clinically significant SIBO host an intestinal flora consisting largely of anaerobes; however, some patients harbor a predominance of gram-negative aerobes, such as Escherichia coli, Klebsiella, and Pseudomonas.45 As a result, the most effective antimicrobial agent is one targeting both aerobic and anaerobic microorganisms.2
Antibiotics
The first-line antibiotic for SIBO has been tetracycline (250 mg four times daily for 7 days).2 However, the high prevalence of bacterial resistance to this drug (up to 60% of patients with SIBO)2 has led to the use of alternative antibiotics. Common alternatives include the quinolones, amoxicillin with clavulanic acid (Augmentin), clindamycin, and metronidazole.46,47 Although included in some of these lists, antibiotics with poor activity against anaerobes might best be avoided in the treatment of SIBO (e.g., penicillin, ampicillin, and the oral aminoglycosides kanamycin and neomycin).2
The minimally absorbed antibiotic, rifaximin, is particularly effective while also minimizing the risk of side effects. In one study, a 7-day course of rifaximin (Xifarxan) at 400 mg three times daily normalized breath hydrogen excretion in 70% of patients with SIBO, whereas tetracycline normalized H2 excretion in only 27% of patients.48 More recent studies of rifaximin utilized 550 mg twice daily for 14 days and demonstrated equivalent resolution of SIBO, as well as elimination of IBS symptoms.49
A poor response to antibiotics may indicate mucosal disease, antibiotic resistance, antibiotic-associated diarrhea, or an incorrect diagnosis.22,50 Recurrence of symptoms after treatment suggests the need for follow-up testing and possible re-treatment. Older age, history of appendectomy, and chronic use of proton pump inhibitors increase the likelihood of recurrence.51 Because prolonged antibiotic therapy significantly raises the risk of diarrhea, Clostridium difficile infection, and bacterial resistance,2 the administration of probiotics is advised to minimize such side effects.21
Antibiotic Alternatives
Peppermint oil, which has been used successfully in patients with IBS, is a volatile oil with antimicrobial properties.52 Enteric-coated peppermint oil (dose of 0.2 mL three times a day) dramatically reduced gastrointestinal symptoms in a patient with SIBO.53 Follow-up breath testing suggested some persistent bacterial overgrowth; the addition of an established antimicrobial agent such as berberine might help improve the results.54 Further research on the use of botanical agents in SIBO is clearly needed.
A small double-blind study examined the effect of oral probiotics (combined Lactobacillus acidophilus and L. casei strains) on SIBO. A significant decrease in breath H2 concentration was noted as early as 1 week into treatment, providing evidence that Lactobacillus strains might be useful in SIBO.55
Addressing the Underlying Cause
Bacterial overgrowth of the small intestine may easily recur if root causes are not addressed.
Restoration of Gastric Acidity
Because gastric acidity is a critical deterrent to SIBO, restoration of normal stomach pH in patients with hypochlorhydria or achlorhydria is essential. This may include the use of betaine hydrochloride with meals or the discontinuation of antacid medications. SIBO has been found in both healthy subjects and patients with an ulcer after even short-term (5-week) administration of omeprazole.56 Alterations in gastric pH affect digestive capacity, leading to incompletely digested proteins providing substrate for bacteria in the terminal ileum.
Normalization of Intestinal Motility
As mentioned, intestinal stasis is another major contributing factor to SIBO. When not resulting from anatomic or organic causes, reduced motility may be improved with measures such as increased dietary fiber, water, probiotics, stress management, and exercise. Surgical correction of anatomic causes of intestinal stasis, such as small bowel diverticula, may be warranted.57
Supportive Measures
SIBO patients may become lactose intolerant as a result of disaccharidase deficiency. This is often ameliorated with bacterial eradication58; however, temporary avoidance of all disaccharides can also help to “starve” the excess bacteria and allow healing of the intestinal lining.59
Substituting more easily absorbed medium-chain triglycerides for most dietary fat may be helpful in patients with diarrhea and steatorrhea.2
Probiotics and prebiotics are recommended to help restore normal balance of intestinal flora, especially in patients with a history of antibiotic use.21,55
1. Bouhnik Y., Alain S., Attar A., et al. Bacterial populations contaminating the upper gut in patients with small intestinal bacterial overgrowth syndrome. Am J Gastroenterol. 1997;94:1327–1331.
2. Toskes P.P. Bacterial overgrowth of the gastrointestinal tract. Adv Intern Med. 1993;38:387–407.
3. Keusch G.T., Solomons N.W. Microorganisms, malabsorption, diarrhea and dysnutrition. J Environ Pathol Toxicol Oncol. 1985;5:165–209.
4. Di Stefano M., Veneto G., Malservisi S., et al. Small intestine bacterial overgrowth and metabolic bone disease. Dig Dis Sci. 2001;46:1077–1082.
5. Thomas P.D., Forbes A., Green J., et al. Guidelines for the investigation of chronic diarrhoea. Gut. 2003;52(Suppl 5):v1–v15.
6. Reddymasu S.C., Sostarich S., McCallum R.W. Small intestinal bacterial overgrowth in irritable bowel syndrome: are there any predictors? BMC Gastroenterol. 2010;10:23.
7. Pimentel M., Chow E.J., Lin H.C. Normalization of lactulose breath testing correlates with symptom improvement in irritable bowel syndrome. A double-blind, randomized, placebo-controlled study. Am J Gastroenterol. 2003;98(2):412–419.
8. Logan A.C., Venket Rao A., Irani D. Chronic fatigue syndrome: lactic acid bacteria may be of therapeutic value. Med Hypotheses. 2003;60(6):915–923.
9. Pimentel M., Wallace D., Hallegua D., et al. A link between irritable bowel syndrome and fibromyalgia may be related to findings on lactulose breath testing. Ann Rheum Dis. 2004;63(4):450–452.
10. Riordan S.M., McIver C.J., Thomas D.H., et al. Luminal bacteria and small-intestinal permeability. Scand J Gastroenterol. 1997;32:556–563.
11. Goebel A., Buhner S., Schedel R., et al. Altered intestinal permeability in patients with primary fibromyalgia and in patients with complex regional pain syndrome. Rheumatology (Oxford). 2008;47(8):1223–1237.
12. Rose S., Young M.A., Reynolds J.C. Gastrointestinal manifestations of scleroderma. Gastroenterol Clin North Am. 1998;27:563–594.
13. Camilleri M. Small bowel motility disorders. Rev Gastroenterol Mex. 1994;59:120–126.
14. Virally-Monod M., Tielmans D., Kevorkian J.P., et al. Chronic diarrhoea and diabetes mellitus: prevalence of small intestinal bacterial overgrowth. Diabetes Metab. 1998;24:530–536.
15. Castiglione F., Del Vecchio Blanco G., Rispo A., et al. Orocecal transit time and bacterial overgrowth in patients with Crohn’s disease. J Clin Gastroenterol. 2000;31:63–66.
16. Anonymous. Small intestinal bacterial overgrowth syndrome. Gastroenterol. 1981;80:834–845.
17. Kirsch M. Bacterial overgrowth. Am J Gastroenterol. 1990;85:231–237.
18. Tursi A., Brandimarte G., Giorgetti G. High prevalence of small intestinal bacterial overgrowth in celiac patients with persistence of gastrointestinal symptoms after gluten withdrawal. Am J Gastroenterol. 2003;98:839–843.
19. Riordan S.M., McIver C.J., Wakefield D., et al. Small intestinal bacterial overgrowth in the symptomatic elderly. Am J Gastroenterol. 1997;92:47–51.
20. Hill M. Normal and pathological microbial flora of the upper gastrointestinal tract. Scand J Gastroenterol. 1985;111(Suppl):1–6.
21. Rolfe R.D. The role of probiotic cultures in the control of gastrointestinal health. J Nutr. 2000;130(Suppl):396S–402S.
22. King C.E., Toskes P.P. Small intestine bacterial overgrowth. Gastroenterol. 1979;76:1035–1055.
23. Sherman P., Lichtman S. Small bowel bacterial overgrowth syndrome. Dig Dis Sci. 1987;5:157–171.
24. Fagundes-Neto U., De Martini-Costa S., Pedroso M.Z., Scaletsky I.C. Studies of the small bowel surface by scanning electron microscopy in infants with persistent diarrhea. Braz J Med Biol Res. 2000;33:1437–1442.
25. Camilo E., Zimmerman J., Mason J.B., et al. Folate synthesized by bacteria in the human upper small intestine is assimilated by the host. Gastroenterol. 1996;110:991–998.
26. O’Leary C., Quigley E.M. Small bowel bacterial overgrowth, celiac disease, and IBS: what are the real associations? Am J Gastroenterol. 2003;98:720–722.
27. Rhodes J.M., Middleton P., Jewell D.P. The lactulose hydrogen breath test as a diagnostic test for small-bowel bacterial overgrowth. Scand J Gastroenterol. 1979;14:333–336.
28. Ford A.C., Spiegel B.M., Talley N.J., Moayyedi P. Small intestinal bacterial overgrowth in irritable bowel syndrome: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2009;7(12):1279–1286.
29. Brummer R.J., Armbrecht U., Bosaeus I., et al. The hydrogen (H2) breath test: sampling methods and the influence of dietary fibre on fasting level. Scand J Gastroenterol. 1985;20:1007–1013.
30. Hamilton L.H. Breath tests and gastroenterology, 2nd ed., Milwaukee: QuinTron Instrument Company, 1998.
31. Cloarec D., Bornet F., Gouilloud S., et al. Breath hydrogen response to lactulose in healthy subjects: relationship to methane producing status. Gut. 1990;31:300–304.
32. Rumessen J.J., Nordgaard-Andersen I., Gudmand-Hoyer E. Carbohydrate malabsorption: quantification by methane and hydrogen breath tests. Scand J Gastroenterol. 1994;29:826–832.
33. Corazza G., Strocchi A., Sorge M., et al. Prevalence and consistency of low breath H2 excretion following lactulose ingestion: possible implications for the clinical use of the H2 breath test. Dig Dis Sci. 1993;38:2010–2016.
34. Kajs T.M., Fitzgerald J.A., Buckner R.Y., et al. Influence of a methanogenic flora on the breath H2 and symptom response to ingestion of sorbitol or oat fiber. Am J Gastroenterol. 1997;92:89–94.
35. Pimentel M., Mayer A.G., Park S., et al. Methane production during lactulose breath test is associated with gastrointestinal disease presentation. Dig Dis Sci. 2003;48:86–92.
36. Romagnuolo J., Schiller D., Bailey R.J. Using breath tests wisely in a gastroenterology practice: an evidence-based review of indications and pitfalls in interpretation. Am J Gastroenterol. 2002;97:1113–1126.
37. Vogelsang H., Ferenci P., Frotz S., et al. Acidic colonic microclimate—possible reason for false negative hydrogen breath tests. Gut. 1988;29:21–26.
38. Kerlin P., Wong L. Breath hydrogen testing in bacterial overgrowth of the small intestine. Gastroenterol. 1988;95:982–988.
39. Perman J.A., Modler S. Glycoproteins as substrates for production of hydrogen and methane by colonic bacterial flora. Gastroenterol. 1982;83:388–393.
40. Solomons N. Evaluation of carbohydrate absorption: the hydrogen breath test in clinical practice. Clin Nutr J. 1984;3:71–78.
41. Thompson D.G., O’Brien J.D., Hardie J.M. Influence of the oropharyngeal microflora on the measurement of exhaled breath hydrogen. Gastroenterol. 1986;91:853–860.
42. Gilat T., Ben Hur H., Gelman-Malachi E., et al. Alterations of the colonic flora and their effect on the hydrogen breath test. Gut. 1978;19:602–605.
43. Solomons N.W., Garcia R., Schneider R., et al. H2 breath tests during diarrhea. Acta Paediatr Scand. 1979;68:171–172.
44. Caride V.J., Prokop E.K., Troncale F.J., et al. Scintigraphic determination of small intestinal transit time: comparison with the hydrogen breath technique. Gastroenterol. 1984;86:714–720.
45. Kocoshis S.A., Schletewitz K., Lovelace G., Laine R.A. Duodenal bile acids among children: keto derivatives and aerobic small bowel bacterial overgrowth. J Pediatr Gastroenterol Nutr. 1987;6:686–696.
46. Meyers J.S., Ehrenpreis E.D., Craig R.M. Small intestinal bacterial overgrowth syndrome. Curr Treat Options Gastroenterol. 2001;4:7–14.
47. Attar A., Flourie B., Rambaud J.C., et al. Antibiotic efficacy in small intestinal bacterial overgrowth-related chronic diarrhea: a crossover, randomized trial. Gastroenterol. 1999;117:794–797.
48. Di Stefano M., Malservisi S., Veneto G., et al. Rifaximin versus chlortetracycline in the short-term treatment of small intestinal bacterial overgrowth. Aliment Pharmacol Ther. 2000;14:551–556.
49. Pimentel M., Lembo A., Chey W.D., et al. Rifaximin therapy for patients with irritable bowel syndrome without constipation. N Engl J Med. 2011;364:22–32.
50. Bjorneklett A., Hoverstad T., Hovig T. Bacterial overgrowth. Scand J Gastroenterol. 1985;109(Suppl):123–132.
51. Lauritano E.C., Gabrielli M., Scarpellini E., et al. Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol. 2008;103(8):2031–2035.
52. Shapiro S., Meier A., Guggenheim B. The antimicrobial activity of essential oils and essential oil components towards oral bacteria. Oral Microbiol Immunol. 1994;9:202–208.
53. Logan A.C., Beaulne T.M. The treatment of small intestinal bacterial overgrowth with enteric-coated peppermint oil: a case report. Alt Med Rev. 2002;7:410–417.
54. Birdsall T., Kelly G. Berberine: therapeutic potential of an alkaloid found in several medicinal plants. Alt Med Rev. 1997;2:94–103.
55. Gaon D., Garmendia C., Murrielo N.O., et al. Effect of Lactobacillus strains (L. casei and L. acidophilus strains cereal) on bacterial overgrowth-related chronic diarrhea. Medicina (Brazil). 2002;62:159–163.
56. Shindo K., Machida M., Fukumura M., et al. Omeprazole induces altered bile acid metabolism. Gut. 1998;42:266–271.
57. Drude R.B., Jr., Finkelman D., Davis W.D., Ferrante W.A. Malabsorption in jejunal diverticulosis treated with resection of the diverticula. Dig Dis Sci. 1980;25:802–806.
58. Nucera C., Lupascu A., Gabrielli M., et al. Sugar intolerance in irritable bowel syndrome: the role of small bowel bacterial overgrowth. Gastroenterol. 2004;126(4 Suppl 2):A511.
59. Gottschall E. Breaking the vicious cycle. Baltimore: Kirkton Press; 1994.