Back
Conceptual overview
General description
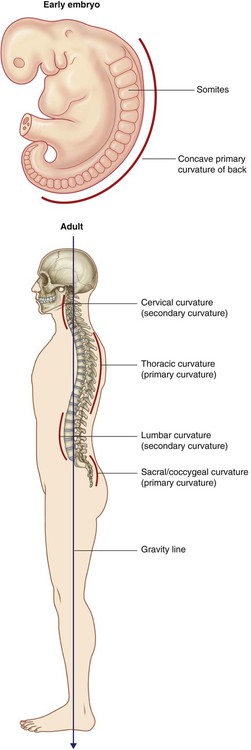
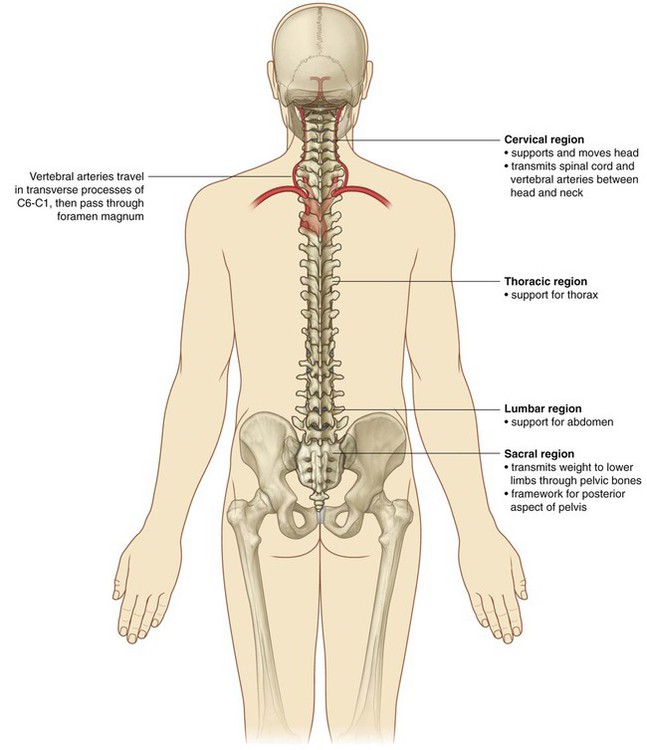
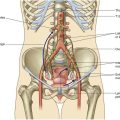
The back consists of the posterior aspect of the body and provides the musculoskeletal axis of support for the trunk. Bony elements consist mainly of the vertebrae, although proximal elements of the ribs, superior aspects of the pelvic bones, and posterior basal regions of the skull contribute to the back’s skeletal framework (Fig. 2.1).
Functions
Support
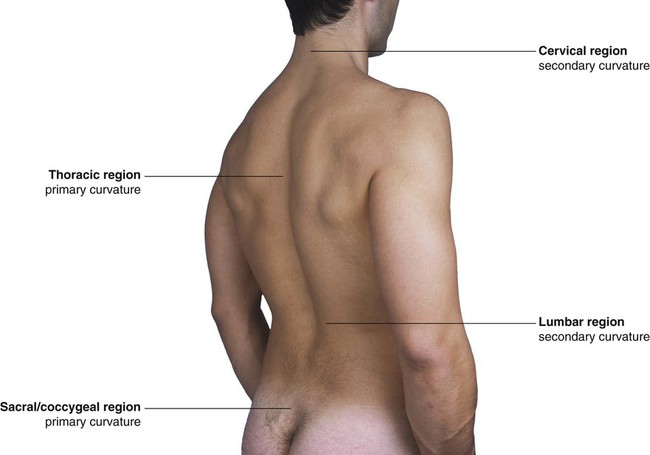
The skeletal and muscular elements of the back support the body’s weight, transmit forces through the pelvis to the lower limbs, carry and position the head, and brace and help maneuver the upper limbs. The vertebral column is positioned posteriorly in the body at the midline. When viewed laterally, it has a number of curvatures (Fig. 2.2):
 The primary curvature of the vertebral column is concave anteriorly, reflecting the original shape of the embryo, and is retained in the thoracic and sacral regions in adults.
The primary curvature of the vertebral column is concave anteriorly, reflecting the original shape of the embryo, and is retained in the thoracic and sacral regions in adults.
 Secondary curvatures, which are concave posteriorly, form in the cervical and lumbar regions and bring the center of gravity into a vertical line, which allows the body’s weight to be balanced on the vertebral column in a way that expends the least amount of muscular energy to maintain an upright bipedal stance.
Secondary curvatures, which are concave posteriorly, form in the cervical and lumbar regions and bring the center of gravity into a vertical line, which allows the body’s weight to be balanced on the vertebral column in a way that expends the least amount of muscular energy to maintain an upright bipedal stance.
Movement
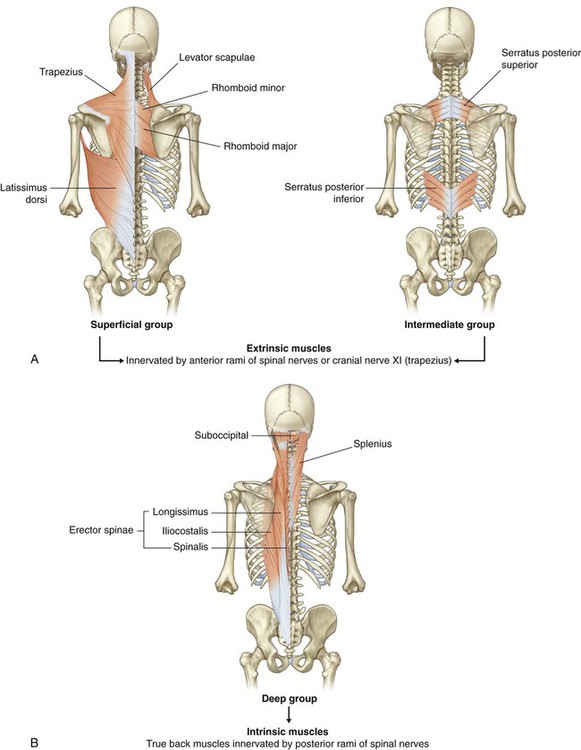
Muscles of the back consist of extrinsic and intrinsic groups:
 The extrinsic muscles of the back move the upper limbs and the ribs.
The extrinsic muscles of the back move the upper limbs and the ribs.
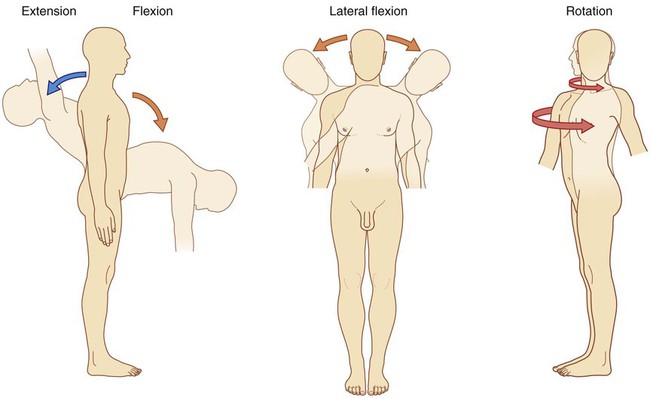
 The intrinsic muscles of the back maintain posture and move the vertebral column; these movements include flexion (anterior bending), extension, lateral flexion, and rotation (Fig. 2.3).
The intrinsic muscles of the back maintain posture and move the vertebral column; these movements include flexion (anterior bending), extension, lateral flexion, and rotation (Fig. 2.3).
In the cervical region, the first two vertebrae and associated muscles are specifically modified to support and position the head. The head flexes and extends, in the nodding motion, on vertebra CI, and rotation of the head occurs as vertebra CI moves on vertebra CII (Fig. 2.3).
Component parts
Bones
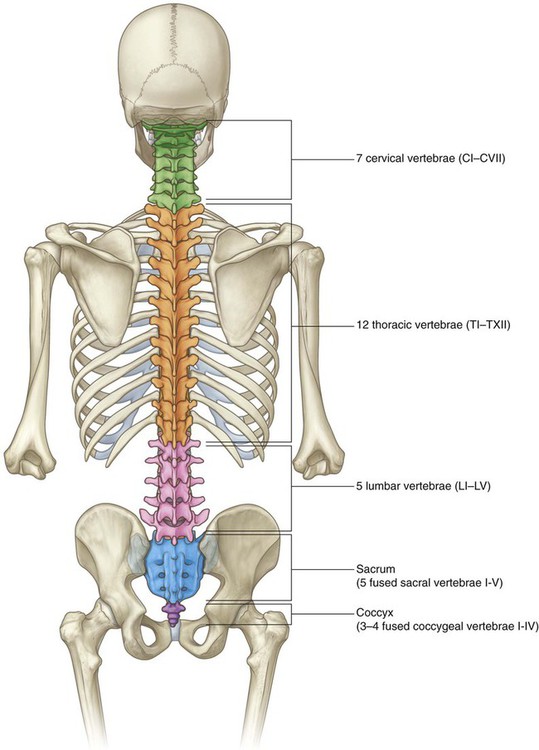
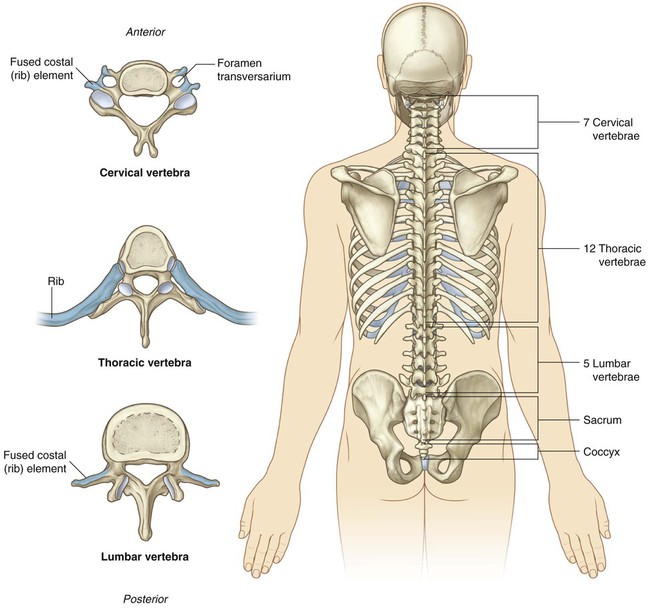
The major bones of the back are the 33 vertebrae (Fig. 2.5). The number and specific characteristics of the vertebrae vary depending on the body region with which they are associated. There are seven cervical, twelve thoracic, five lumbar, five sacral, and three to four coccygeal vertebrae. The sacral vertebrae fuse into a single bony element, the sacrum. The coccygeal vertebrae are rudimentary in structure, vary in number from three to four, and often fuse into a single coccyx.
Typical vertebra
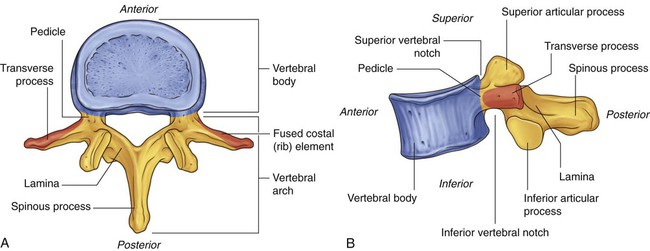
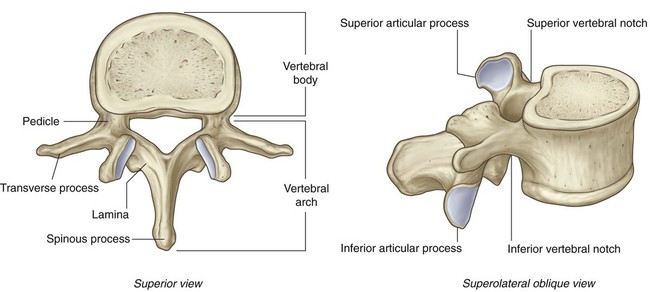
A typical vertebra consists of a vertebral body and a vertebral arch (Fig. 2.6).
The vertebral arch of a typical vertebra has a number of characteristic projections, which serve as:
A spinous process projects posteriorly and generally inferiorly from the roof of the vertebral arch.
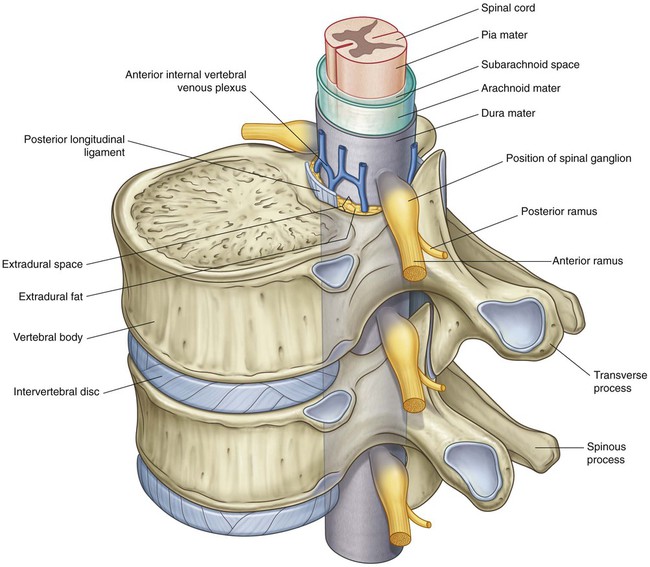
Vertebral canal
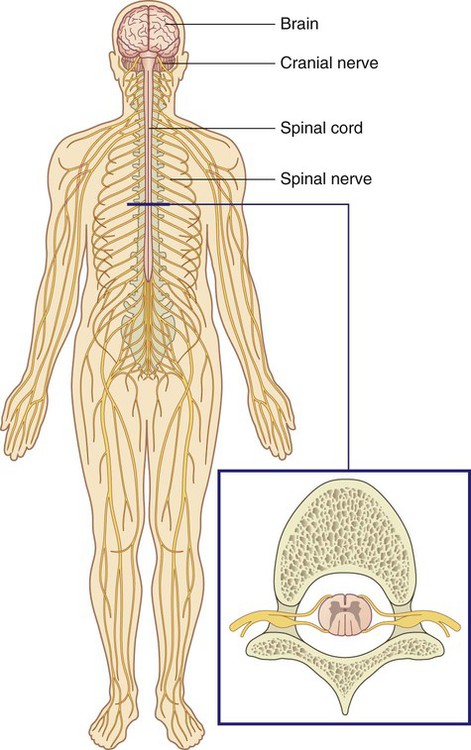
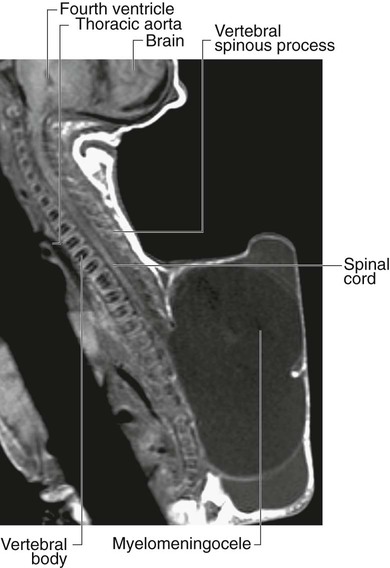
The spinal cord lies within a bony canal formed by adjacent vertebrae and soft tissue elements (the vertebral canal) (Fig. 2.8):
 The anterior wall is formed by the vertebral bodies of the vertebrae, intervertebral discs, and associated ligaments.
The anterior wall is formed by the vertebral bodies of the vertebrae, intervertebral discs, and associated ligaments.
 The lateral walls and roof are formed by the vertebral arches and ligaments.
The lateral walls and roof are formed by the vertebral arches and ligaments.
 The pia mater is the innermost membrane and is intimately associated with the surface of the spinal cord.
The pia mater is the innermost membrane and is intimately associated with the surface of the spinal cord.
 The second membrane, the arachnoid mater, is separated from the pia by the subarachnoid space, which contains cerebrospinal fluid.
The second membrane, the arachnoid mater, is separated from the pia by the subarachnoid space, which contains cerebrospinal fluid.
 The thickest and most external of the membranes, the dura mater, lies directly against, but is not attached to, the arachnoid mater.
The thickest and most external of the membranes, the dura mater, lies directly against, but is not attached to, the arachnoid mater.
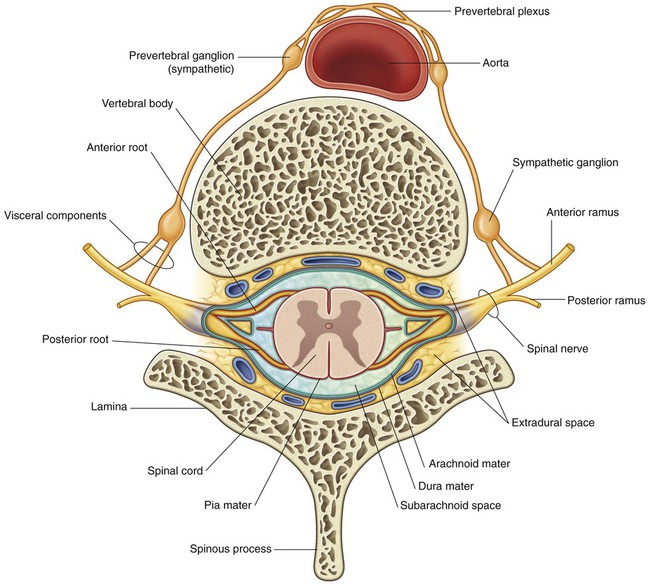
Spinal nerves
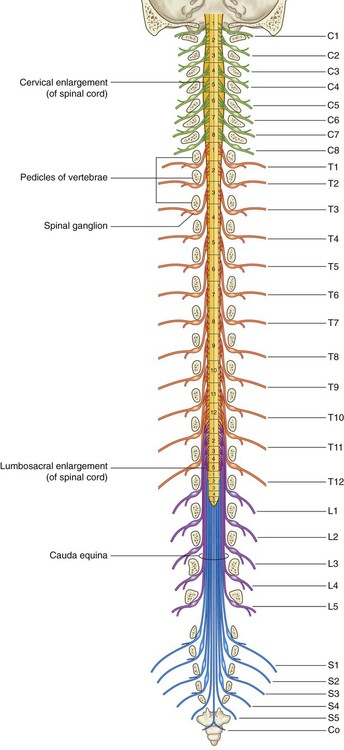
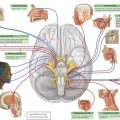
The 31 pairs of spinal nerves are segmental in distribution and emerge from the vertebral canal between the pedicles of adjacent vertebrae. There are eight pairs of cervical nerves (C1 to C8), twelve thoracic (T1 to T12), five lumbar (L1 to L5), five sacral (S1 to S5), and one coccygeal (Co). Each nerve is attached to the spinal cord by a posterior root and an anterior root (Fig. 2.9).
After exiting the vertebral canal, each spinal nerve branches into:
Relationship to other regions
Head
Cervical regions of the back constitute the skeletal and much of the muscular framework of the neck, which in turn supports and moves the head (Fig. 2.10).
Thorax, abdomen, and pelvis
The different regions of the vertebral column contribute to the skeletal framework of the thorax, abdomen, and pelvis (Fig. 2.10). In addition to providing support for each of these parts of the body, the vertebrae provide attachments for muscles and fascia, and articulation sites for other bones. The anterior rami of spinal nerves associated with the thorax, abdomen, and pelvis pass into these parts of the body from the back.
Key features
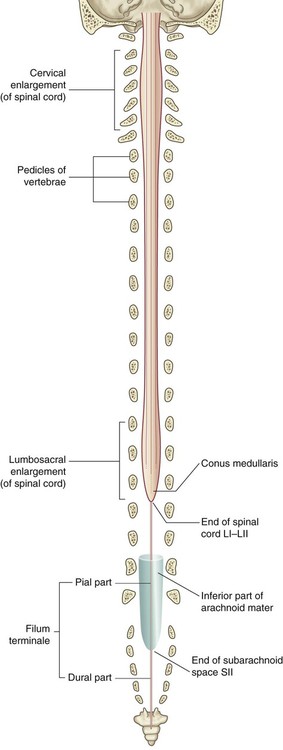
Long vertebral column and short spinal cord
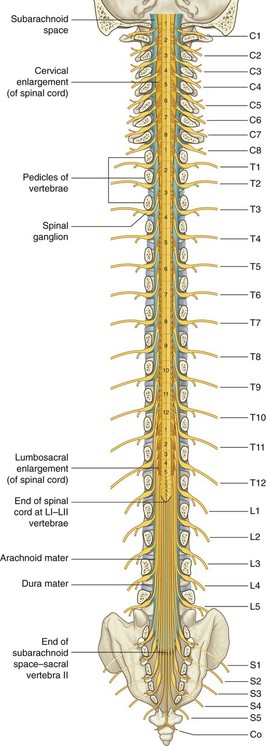
During development, the vertebral column grows much faster than the spinal cord. As a result, the spinal cord does not extend the entire length of the vertebral canal (Fig. 2.11).
Intervertebral foramina and spinal nerves
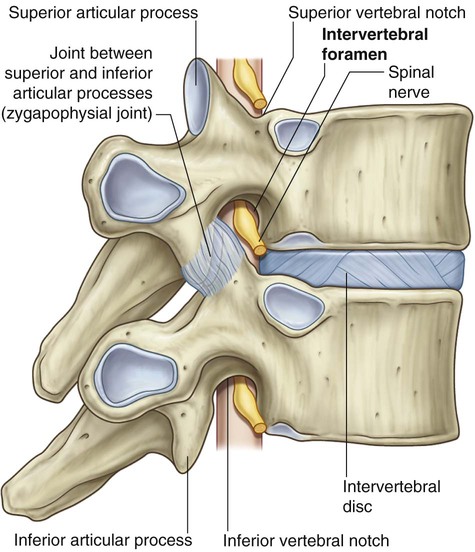
Each spinal nerve exits the vertebral canal laterally through an intervertebral foramen (Fig. 2.12). The foramen is formed between adjacent vertebral arches and is closely related to intervertebral joints:
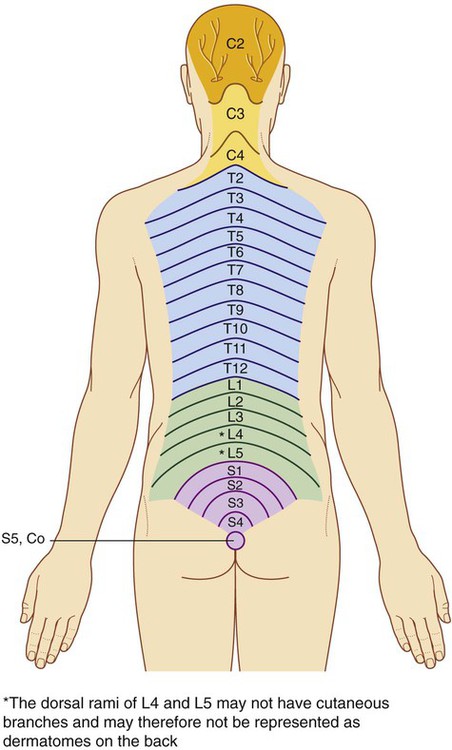
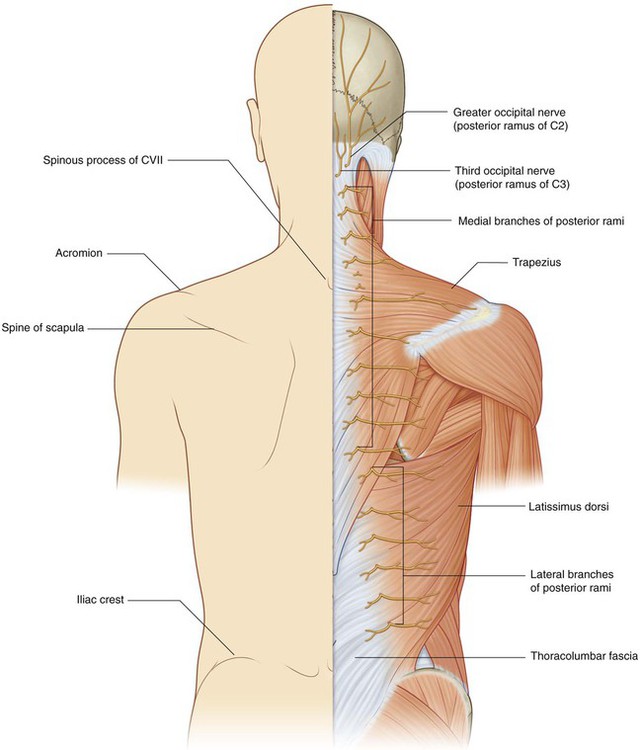
Innervation of the back
Posterior branches of spinal nerves innervate the intrinsic muscles of the back and adjacent skin. The cutaneous distribution of these posterior rami extends into the gluteal region of the lower limb and the posterior aspect of the head. Parts of dermatomes innervated by the posterior rami of spinal nerves are shown in Fig. 2.13.
Regional anatomy
Skeletal framework
Vertebrae
There are approximately 33 vertebrae, which are subdivided into five groups based on morphology and location (Fig. 2.14):
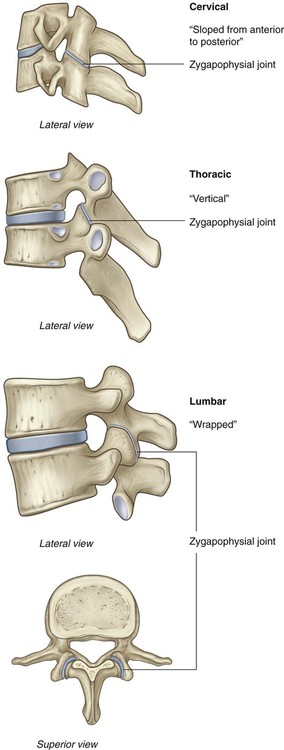
 The seven cervical vertebrae between the thorax and skull are characterized mainly by their small size and the presence of a foramen in each transverse process (Figs. 2.14 and 2.15).
The seven cervical vertebrae between the thorax and skull are characterized mainly by their small size and the presence of a foramen in each transverse process (Figs. 2.14 and 2.15).


 The 12 thoracic vertebrae are characterized by their articulated ribs (Figs. 2.14 and 2.16); although all vertebrae have rib elements, these elements are small and are incorporated into the transverse processes in regions other than the thorax; but in the thorax, the ribs are separate bones and articulate via synovial joints with the vertebral bodies and transverse processes of the associated vertebrae.
The 12 thoracic vertebrae are characterized by their articulated ribs (Figs. 2.14 and 2.16); although all vertebrae have rib elements, these elements are small and are incorporated into the transverse processes in regions other than the thorax; but in the thorax, the ribs are separate bones and articulate via synovial joints with the vertebral bodies and transverse processes of the associated vertebrae.
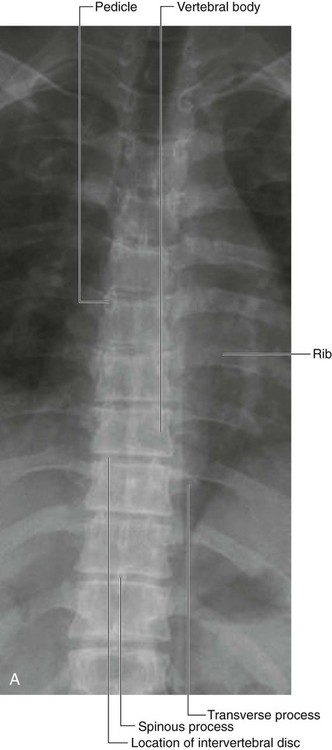

 Inferior to the thoracic vertebrae are five lumbar vertebrae, which form the skeletal support for the posterior abdominal wall and are characterized by their large size (Figs. 2.14 and 2.17).
Inferior to the thoracic vertebrae are five lumbar vertebrae, which form the skeletal support for the posterior abdominal wall and are characterized by their large size (Figs. 2.14 and 2.17).


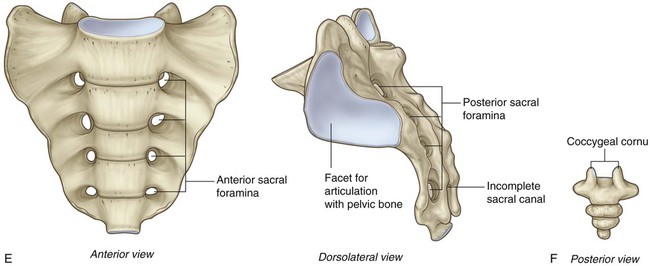
 Next are five sacral vertebrae fused into one single bone called the sacrum, which articulates on each side with a pelvic bone and is a component of the pelvic wall.
Next are five sacral vertebrae fused into one single bone called the sacrum, which articulates on each side with a pelvic bone and is a component of the pelvic wall.
 Inferior to the sacrum is a variable number, usually four, of coccygeal vertebrae, which fuse into a single small triangular bone called the coccyx.
Inferior to the sacrum is a variable number, usually four, of coccygeal vertebrae, which fuse into a single small triangular bone called the coccyx.
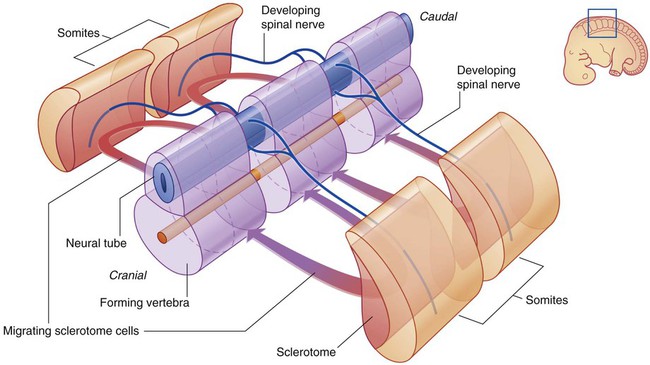
In the embryo, the vertebrae are formed intersegmentally from cells called sclerotomes, which originate from adjacent somites (Fig. 2.18). Each vertebra is derived from the cranial parts of the two somites below, one on each side, and the caudal parts of the two somites above. The spinal nerves develop segmentally and pass between the forming vertebrae.
Typical vertebra
A typical vertebra consists of a vertebral body and a posterior vertebral arch (Fig. 2.19). Extending from the vertebral arch are a number of processes for muscle attachment and articulation with adjacent bone.
The vertebral arch forms the lateral and posterior parts of the vertebral foramen.
The vertebral arch of each vertebra consists of pedicles and laminae (Fig. 2.19):
 The two pedicles are bony pillars that attach the vertebral arch to the vertebral body.
The two pedicles are bony pillars that attach the vertebral arch to the vertebral body.
 The two laminae are flat sheets of bone that extend from each pedicle to meet in the midline and form the roof of the vertebral arch.
The two laminae are flat sheets of bone that extend from each pedicle to meet in the midline and form the roof of the vertebral arch.
Also projecting from the region where the pedicles join the laminae are superior and inferior articular processes (Fig. 2.19), which articulate with the inferior and superior articular processes, respectively, of adjacent vertebrae.
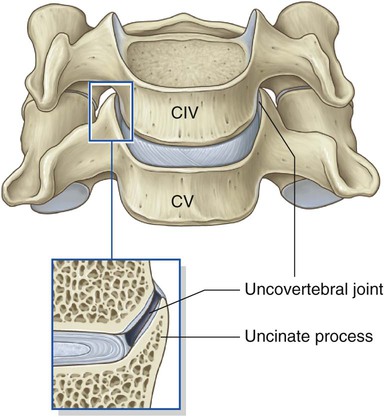
Cervical vertebrae
The seven cervical vertebrae are characterized by their small size and by the presence of a foramen in each transverse process. A typical cervical vertebra has the following features (Fig. 2.20A):
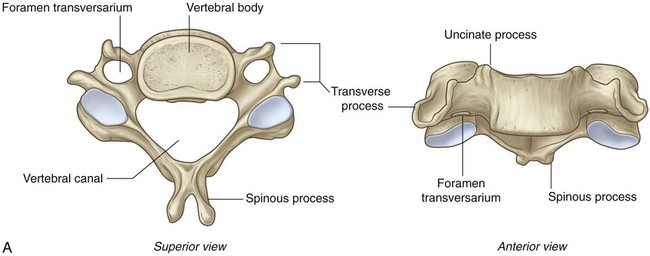
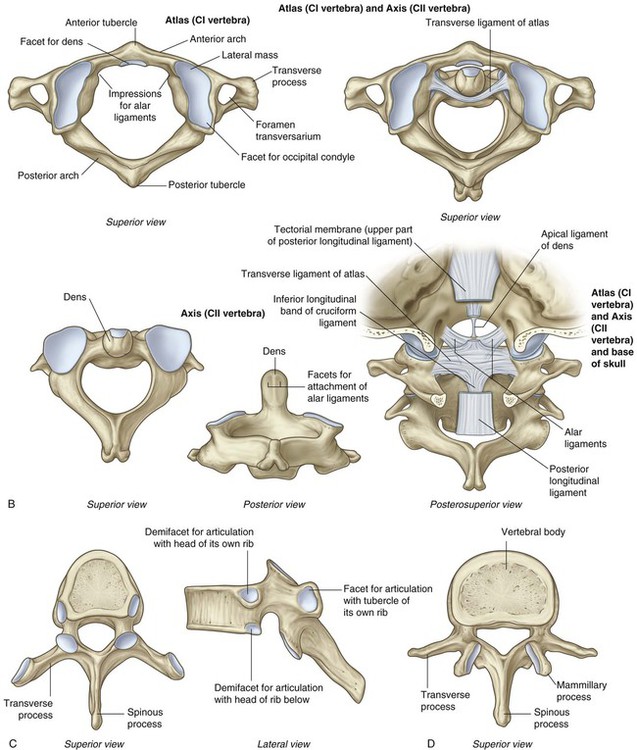
B. Atlas and axis. C. Typical thoracic vertebra. D. Typical lumbar vertebra.
E. Sacrum. F. Coccyx.
 The vertebral body is short in height and square shaped when viewed from above and has a concave superior surface and a convex inferior surface.
The vertebral body is short in height and square shaped when viewed from above and has a concave superior surface and a convex inferior surface.
 Each transverse process is trough shaped and perforated by a round foramen transversarium.
Each transverse process is trough shaped and perforated by a round foramen transversarium.
Atlas and axis
Vertebra CI (the atlas) articulates with the head (Fig. 2.21). Its major distinguishing feature is that it lacks a vertebral body (Fig. 2.20B). In fact, the vertebral body of CI fuses onto the body of CII during development to become the dens of CII. As a result, there is no intervertebral disc between CI and CII. When viewed from above, the atlas is ring shaped and composed of two lateral masses interconnected by an anterior arch and a posterior arch.
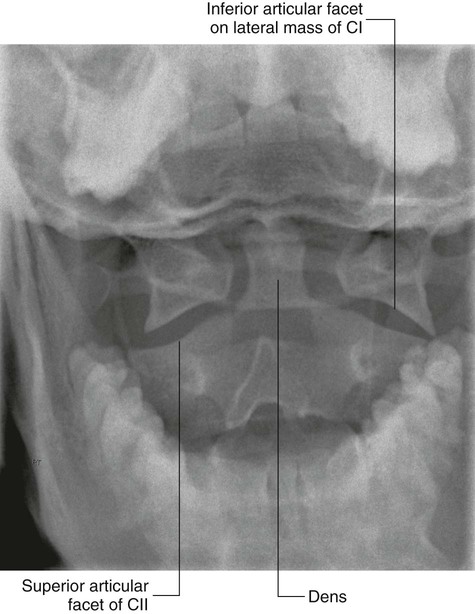
The atlanto-occipital joint allows the head to nod up and down on the vertebral column.
The axis is characterized by the large tooth-like dens, which extends superiorly from the vertebral body (Figs. 2.20B and 2.21). The anterior surface of the dens has an oval facet for articulation with the anterior arch of the atlas.
Thoracic vertebrae
The twelve thoracic vertebrae are all characterized by their articulation with ribs. A typical thoracic vertebra has two partial facets (superior and inferior costal facets) on each side of the vertebral body for articulation with the head of its own rib and the head of the rib below (Fig. 2.20C). The superior costal facet is much larger than the inferior costal facet.
Lumbar vertebrae
The five lumbar vertebrae are distinguished from vertebrae in other regions by their large size (Fig. 2.20D). Also, they lack facets for articulation with ribs. The transverse processes are generally thin and long, with the exception of those on vertebra LV, which are massive and somewhat cone shaped for the attachment of iliolumbar ligaments to connect the transverse processes to the pelvic bones.
Sacrum
The sacrum is a single bone that represents the five fused sacral vertebrae (Fig. 2.20E). It is triangular in shape with the apex pointed inferiorly, and is curved so that it has a concave anterior surface and a correspondingly convex posterior surface. It articulates above with vertebra LV and below with the coccyx. It has two large L-shaped facets, one on each lateral surface, for articulation with the pelvic bones.
The posterior wall of the vertebral canal may be incomplete near the inferior end of the sacrum.
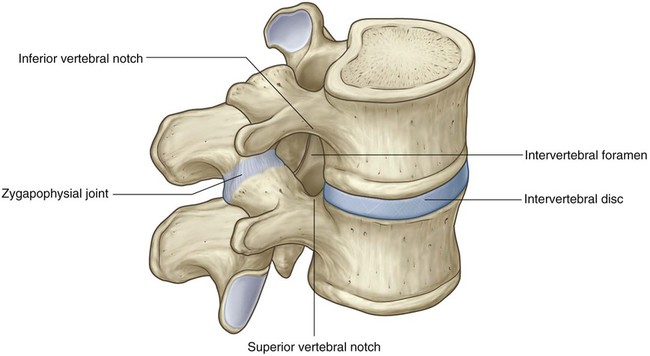
Intervertebral foramina
Intervertebral foramina are formed on each side between adjacent parts of vertebrae and associated intervertebral discs (Fig. 2.22). The foramina allow structures, such as spinal nerves and blood vessels, to pass in and out of the vertebral canal.
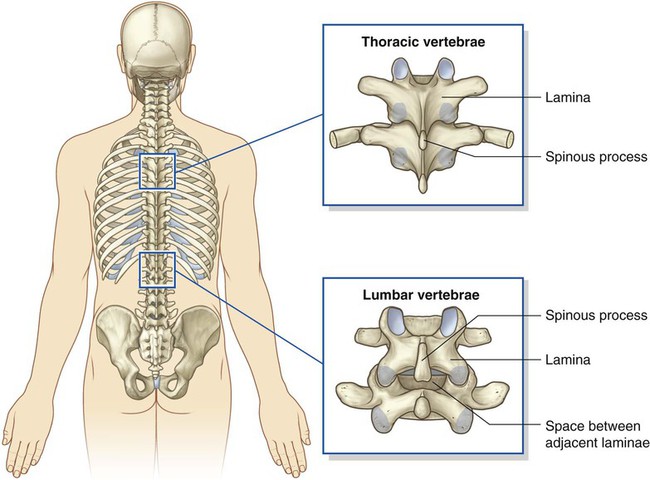
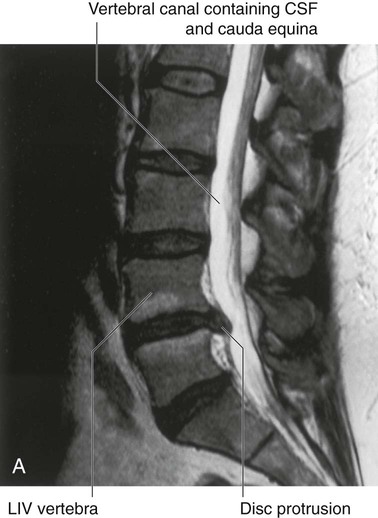
Posterior spaces between vertebral arches
In most regions of the vertebral column, the laminae and spinous processes of adjacent vertebrae overlap to form a reasonably complete bony dorsal wall for the vertebral canal. However, in the lumbar region, large gaps exist between the posterior components of adjacent vertebral arches (Fig. 2.23). These gaps between adjacent laminae and spinous processes become increasingly wide from vertebra LI to vertebra LV. The spaces can be widened further by flexion of the vertebral column. These gaps allow relatively easy access to the vertebral canal for clinical procedures.
Joints
Joints between vertebrae in the back
The two major types of joints between vertebrae are:
Symphyses between vertebral bodies (intervertebral discs)
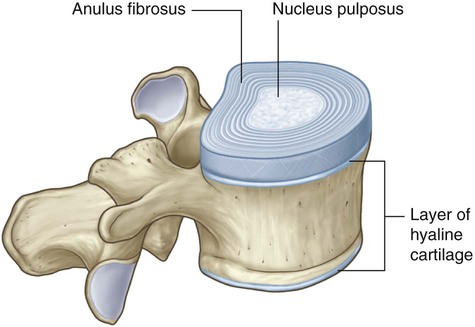
The intervertebral disc consists of an outer anulus fibrosus, which surrounds a central nucleus pulposus (Fig. 2.27).
 The anulus fibrosus consists of an outer ring of collagen surrounding a wider zone of fibrocartilage arranged in a lamellar configuration. This arrangement of fibers limits rotation between vertebrae.
The anulus fibrosus consists of an outer ring of collagen surrounding a wider zone of fibrocartilage arranged in a lamellar configuration. This arrangement of fibers limits rotation between vertebrae.
 The nucleus pulposus fills the center of the intervertebral disc, is gelatinous, and absorbs compression forces between vertebrae.
The nucleus pulposus fills the center of the intervertebral disc, is gelatinous, and absorbs compression forces between vertebrae.
Ligaments
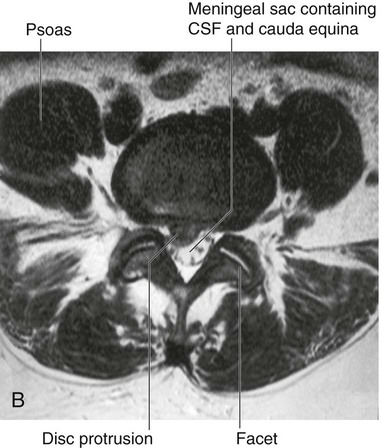
Anterior and posterior longitudinal ligaments
The anterior and posterior longitudinal ligaments are on the anterior and posterior surfaces of the vertebral bodies and extend along most of the vertebral column (Fig. 2.31).
The posterior longitudinal ligament is on the posterior surfaces of the vertebral bodies and lines the anterior surface of the vertebral canal. Like the anterior longitudinal ligament, it is attached along its length to the vertebral bodies and intervertebral discs. The upper part of the posterior longitudinal ligament that connects CII to the intracranial aspect of the base of the skull is termed the tectorial membrane (see Fig. 2.20B).
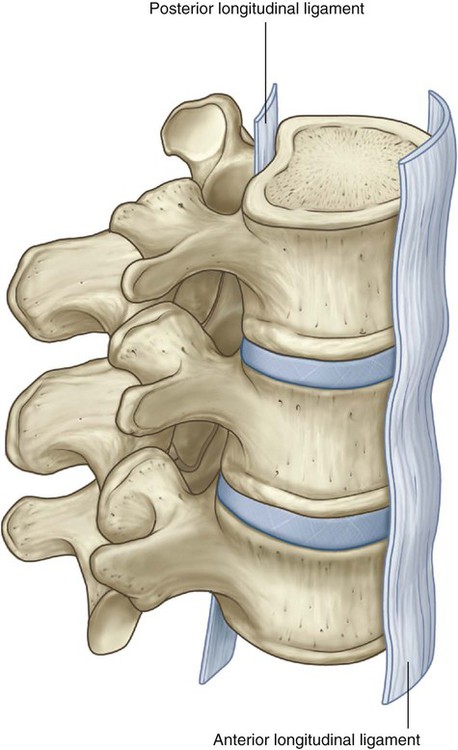
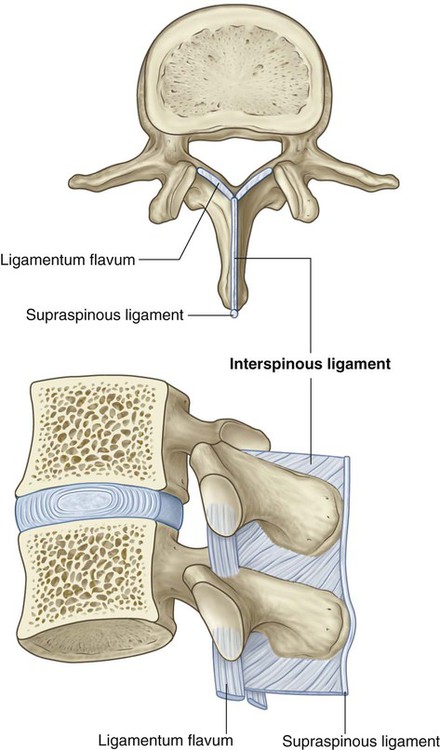
Ligamenta flava
The ligamenta flava, on each side, pass between the laminae of adjacent vertebrae (Fig. 2.32). These thin, broad ligaments consist predominantly of elastic tissue and form part of the posterior surface of the vertebral canal. Each ligamentum flavum runs between the posterior surface of the lamina on the vertebra below to the anterior surface of the lamina of the vertebra above. The ligamenta flava resist separation of the laminae in flexion and assist in extension back to the anatomical position.
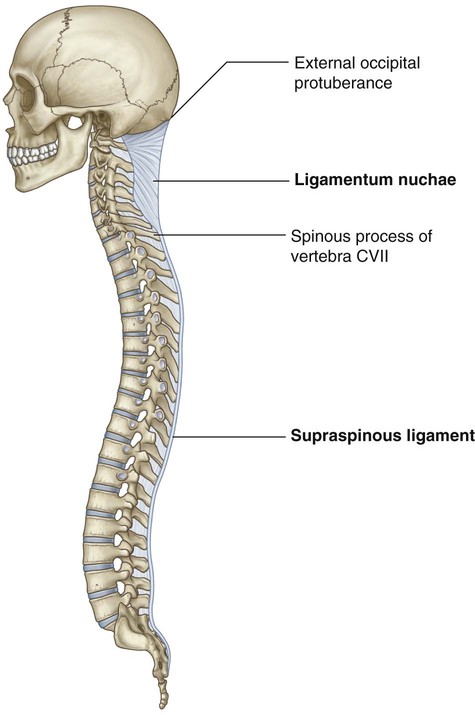
Supraspinous ligament and ligamentum nuchae
The supraspinous ligament connects and passes along the tips of the vertebral spinous processes from vertebra CVII to the sacrum (Fig. 2.33). From vertebra CVII to the skull, the ligament becomes structurally distinct from more caudal parts of the ligament and is called the ligamentum nuchae.
The ligamentum nuchae is a triangular, sheet-like structure in the median sagittal plane:
 The base of the triangle is attached to the skull, from the external occipital protuberance to the foramen magnum.
The base of the triangle is attached to the skull, from the external occipital protuberance to the foramen magnum.
 The apex is attached to the tip of the spinous process of vertebra CVII.
The apex is attached to the tip of the spinous process of vertebra CVII.
 The deep side of the triangle is attached to the posterior tubercle of vertebra CI and the spinous processes of the other cervical vertebrae.
The deep side of the triangle is attached to the posterior tubercle of vertebra CI and the spinous processes of the other cervical vertebrae.
Back musculature
Muscles of the back are organized into superficial, intermediate, and deep groups.
 The superficial group consists of muscles related to and involved in movements of the upper limb.
The superficial group consists of muscles related to and involved in movements of the upper limb.
 The intermediate group consists of muscles attached to the ribs and may serve a respiratory function.
The intermediate group consists of muscles attached to the ribs and may serve a respiratory function.
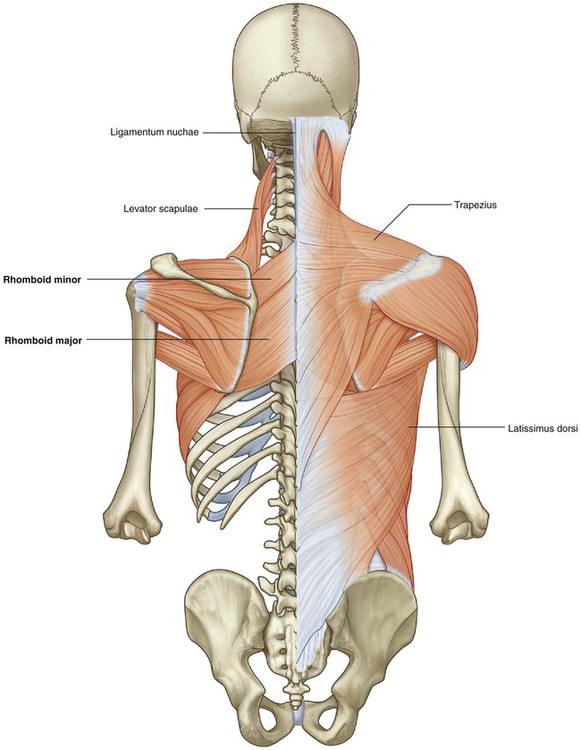
Superficial group of back muscles
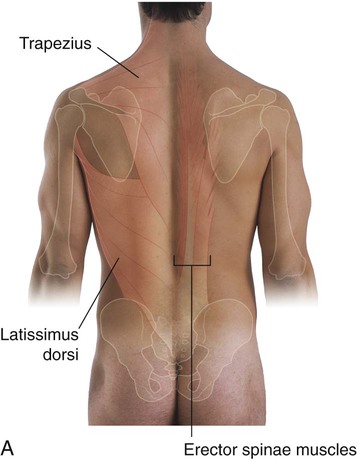
The muscles in the superficial group are immediately deep to the skin and superficial fascia (Figs. 2.36 to 2.39). They attach the superior part of the appendicular skeleton (clavicle, scapula, and humerus) to the axial skeleton (skull, ribs, and vertebral column). Because these muscles are primarily involved with movements of this part of the appendicular skeleton, they are sometimes referred to as the appendicular group.
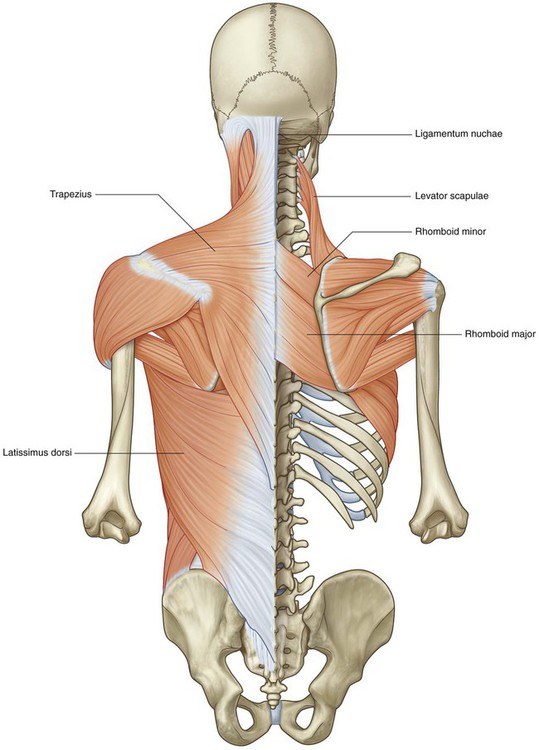
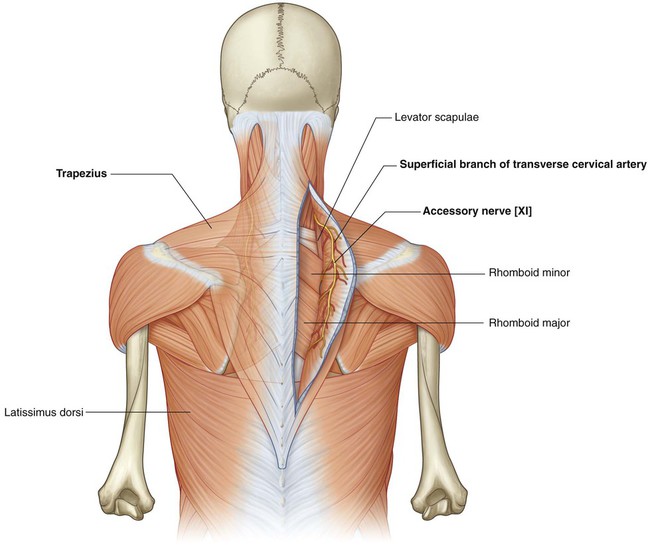
Trapezius
Each trapezius muscle is flat and triangular, with the base of the triangle situated along the vertebral column (the muscle’s origin) and the apex pointing toward the tip of the shoulder (the muscle’s insertion) (Fig. 2.37 and Table 2.1). The muscles on both sides together form a trapezoid.
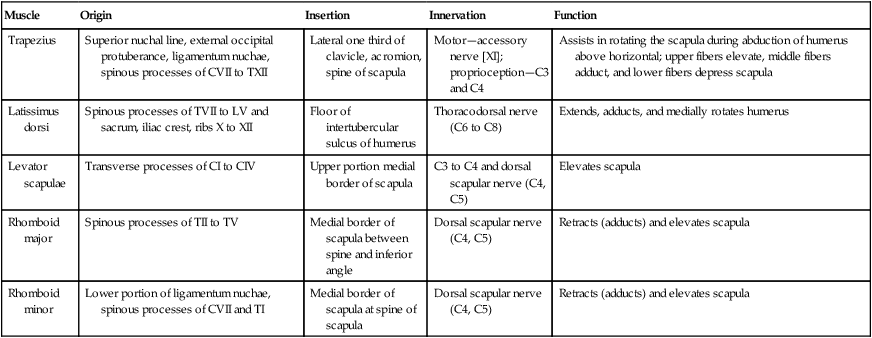
Table 2.1
Superficial (appendicular) group of back muscles
| Muscle | Origin | Insertion | Innervation | Function |
| Trapezius | Superior nuchal line, external occipital protuberance, ligamentum nuchae, spinous processes of CVII to TXII | Lateral one third of clavicle, acromion, spine of scapula | Motor—accessory nerve [XI]; proprioception—C3 and C4 | Assists in rotating the scapula during abduction of humerus above horizontal; upper fibers elevate, middle fibers adduct, and lower fibers depress scapula |
| Latissimus dorsi | Spinous processes of TVII to LV and sacrum, iliac crest, ribs X to XII | Floor of intertubercular sulcus of humerus | Thoracodorsal nerve (C6 to C8) | Extends, adducts, and medially rotates humerus |
| Levator scapulae | Transverse processes of CI to CIV | Upper portion medial border of scapula | C3 to C4 and dorsal scapular nerve (C4, C5) | Elevates scapula |
| Rhomboid major | Spinous processes of TII to TV | Medial border of scapula between spine and inferior angle | Dorsal scapular nerve (C4, C5) | Retracts (adducts) and elevates scapula |
| Rhomboid minor | Lower portion of ligamentum nuchae, spinous processes of CVII and TI | Medial border of scapula at spine of scapula | Dorsal scapular nerve (C4, C5) | Retracts (adducts) and elevates scapula |
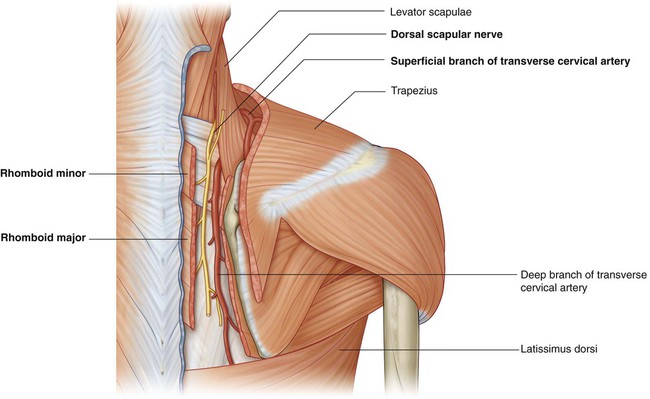
Motor innervation of the trapezius is by the accessory nerve [XI], which descends from the neck onto the deep surface of the muscle (Fig. 2.38). Proprioceptive fibers from the trapezius pass in the branches of the cervical plexus and enter the spinal cord at spinal cord levels C3 and C4.
Latissimus dorsi
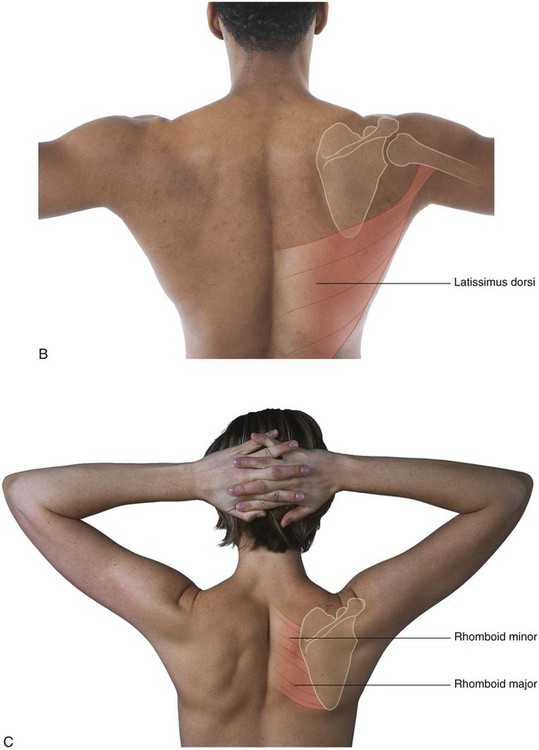
Latissimus dorsi is a large, flat triangular muscle that begins in the lower portion of the back and tapers as it ascends to a narrow tendon that attaches to the humerus anteriorly (Figs. 2.36 to 2.39 and Table 2.1). As a result, movements associated with this muscle include extension, adduction, and medial rotation of the upper limb. The latissimus dorsi can also depress the shoulder, preventing its upward movement.
Levator scapulae
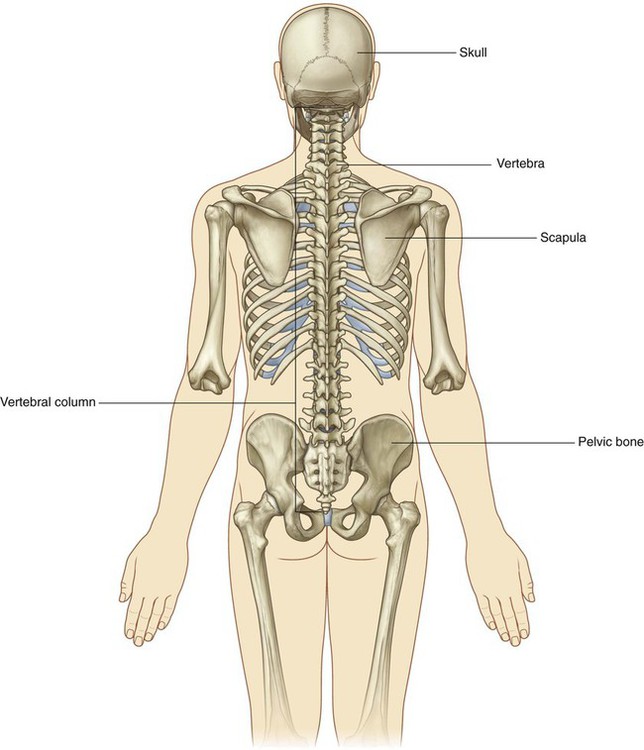
Levator scapulae is a slender muscle that descends from the transverse processes of the upper cervical vertebrae to the upper portion of the scapula on its medial border at the superior angle (Fig. 2.37 and 2.39, and Table 2.1). It elevates the scapula and may assist other muscles in rotating the lateral aspect of the scapula inferiorly.
Rhomboid minor and rhomboid major
The two rhomboid muscles are inferior to levator scapulae (Fig. 2.39 and Table 2.1). Rhomboid minor is superior to rhomboid major, and is a small, cylindrical muscle that arises from the ligamentum nuchae of the neck and the spinous processes of vertebrae CVII and TI and attaches to the medial scapular border opposite the root of the spine of the scapula.
The dorsal scapular nerve, a branch of the brachial plexus, innervates both rhomboid muscles (Fig. 2.40).
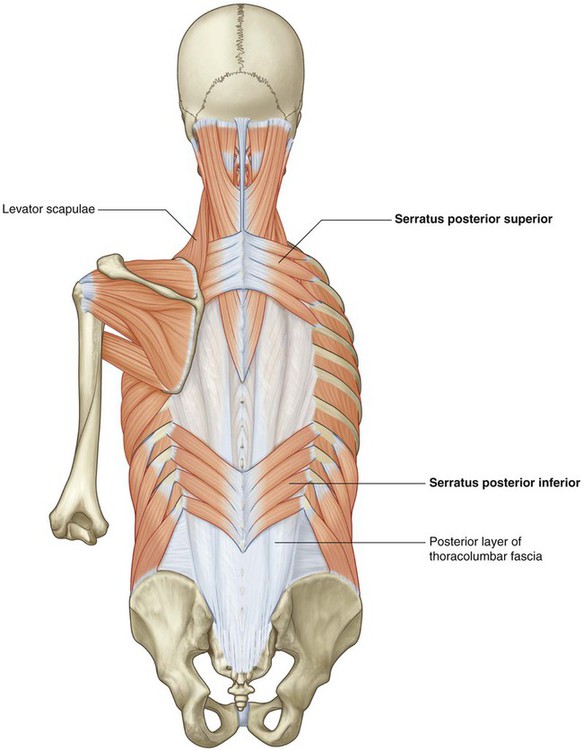
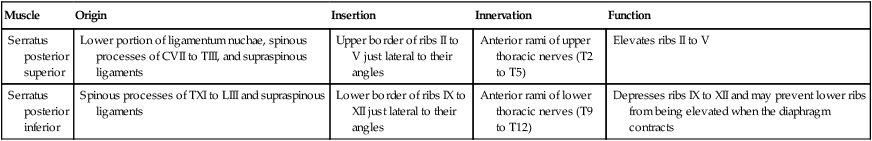
Intermediate group of back muscles
The muscles in the intermediate group of back muscles consist of two thin muscular sheets in the superior and inferior regions of the back, immediately deep to the muscles in the superficial group (Fig. 2.41 and Table 2.2). Fibers from these two serratus posterior muscles (serratus posterior superior and serratus posterior inferior) pass obliquely outward from the vertebral column to attach to the ribs. This positioning suggests a respiratory function, and at times, these muscles have been referred to as the respiratory group.
Table 2.2
Intermediate (respiratory) group of back muscles
| Muscle | Origin | Insertion | Innervation | Function |
| Serratus posterior superior | Lower portion of ligamentum nuchae, spinous processes of CVII to TIII, and supraspinous ligaments | Upper border of ribs II to V just lateral to their angles | Anterior rami of upper thoracic nerves (T2 to T5) | Elevates ribs II to V |
| Serratus posterior inferior | Spinous processes of TXI to LIII and supraspinous ligaments | Lower border of ribs IX to XII just lateral to their angles | Anterior rami of lower thoracic nerves (T9 to T12) | Depresses ribs IX to XII and may prevent lower ribs from being elevated when the diaphragm contracts |
Deep group of back muscles
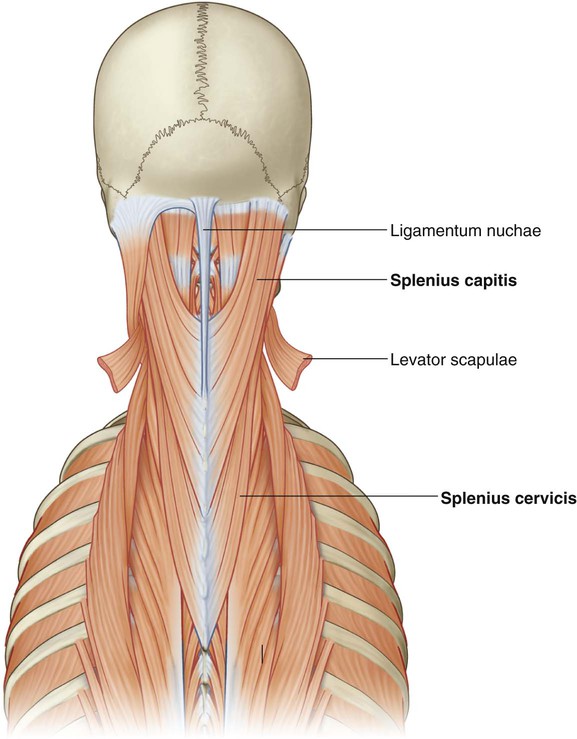
 the extensors and rotators of the head and neck—the splenius capitis and cervicis (spinotransversales muscles),
the extensors and rotators of the head and neck—the splenius capitis and cervicis (spinotransversales muscles),
 the extensors and rotators of the vertebral column—the erector spinae and transversospinales, and
the extensors and rotators of the vertebral column—the erector spinae and transversospinales, and
 the short segmental muscles—the interspinales and intertransversarii.
the short segmental muscles—the interspinales and intertransversarii.
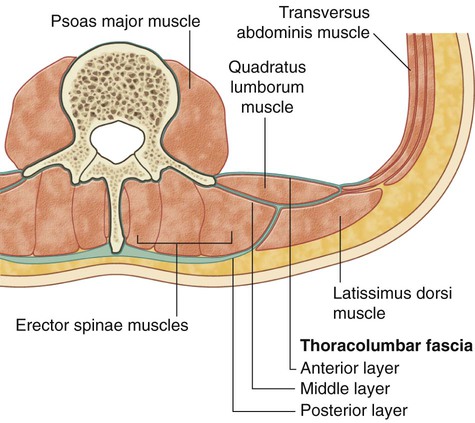
Thoracolumbar fascia
The thoracolumbar fascia covers the deep muscles of the back and trunk (Fig. 2.42). This fascial layer is critical to the overall organization and integrity of the region:
 Superiorly, it passes anteriorly to the serratus posterior muscle and is continuous with deep fascia in the neck.
Superiorly, it passes anteriorly to the serratus posterior muscle and is continuous with deep fascia in the neck.
 In the thoracic region, it covers the deep muscles and separates them from the muscles in the superficial and intermediate groups.
In the thoracic region, it covers the deep muscles and separates them from the muscles in the superficial and intermediate groups.
 Medially, it attaches to the spinous processes of the thoracic vertebrae and, laterally, to the angles of the ribs.
Medially, it attaches to the spinous processes of the thoracic vertebrae and, laterally, to the angles of the ribs.
 The posterior layer is thick and is attached to the spinous processes of the lumbar vertebrae and sacral vertebrae and to the supraspinous ligament—from these attachments, it extends laterally to cover the erector spinae.
The posterior layer is thick and is attached to the spinous processes of the lumbar vertebrae and sacral vertebrae and to the supraspinous ligament—from these attachments, it extends laterally to cover the erector spinae.
 The middle layer is attached medially to the tips of the transverse processes of the lumbar vertebrae and intertransverse ligaments—inferiorly, it is attached to the iliac crest and, superiorly, to the lower border of rib XII.
The middle layer is attached medially to the tips of the transverse processes of the lumbar vertebrae and intertransverse ligaments—inferiorly, it is attached to the iliac crest and, superiorly, to the lower border of rib XII.
 The anterior layer covers the anterior surface of the quadratus lumborum muscle (a muscle of the posterior abdominal wall) and is attached medially to the transverse processes of the lumbar vertebrae—inferiorly, it is attached to the iliac crest and, superiorly, it forms the lateral arcuate ligament for attachment of the diaphragm.
The anterior layer covers the anterior surface of the quadratus lumborum muscle (a muscle of the posterior abdominal wall) and is attached medially to the transverse processes of the lumbar vertebrae—inferiorly, it is attached to the iliac crest and, superiorly, it forms the lateral arcuate ligament for attachment of the diaphragm.
The posterior and middle layers of the thoracolumbar fascia come together at the lateral margin of the erector spinae (Fig. 2.42). At the lateral border of the quadratus lumborum, the anterior layer joins them and forms the aponeurotic origin for the transversus abdominis muscle of the abdominal wall.
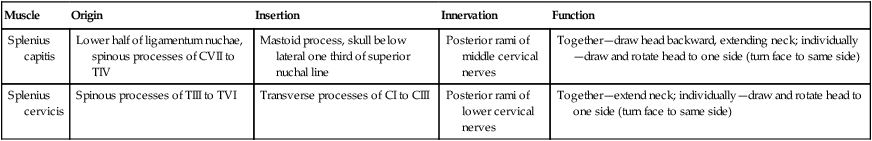
Spinotransversales muscles
The two spinotransversales muscles run from the spinous processes and ligamentum nuchae upward and laterally (Fig. 2.43 and Table 2.3):
Table 2.3
| Muscle | Origin | Insertion | Innervation | Function |
| Splenius capitis | Lower half of ligamentum nuchae, spinous processes of CVII to TIV | Mastoid process, skull below lateral one third of superior nuchal line | Posterior rami of middle cervical nerves | Together—draw head backward, extending neck; individually—draw and rotate head to one side (turn face to same side) |
| Splenius cervicis | Spinous processes of TIII to TVI | Transverse processes of CI to CIII | Posterior rami of lower cervical nerves | Together—extend neck; individually—draw and rotate head to one side (turn face to same side) |
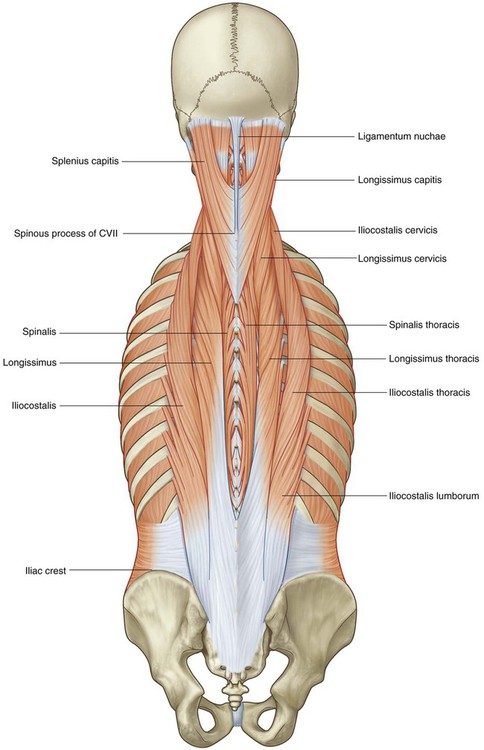
Erector spinae muscles
The erector spinae is the largest group of intrinsic back muscles. The muscles lie posterolaterally to the vertebral column between the spinous processes medially and the angles of the ribs laterally. They are covered in the thoracic and lumbar regions by thoracolumbar fascia and the serratus posterior inferior, rhomboid, and splenius muscles. The mass arises from a broad, thick tendon attached to the sacrum, the spinous processes of the lumbar and lower thoracic vertebrae, and the iliac crest (Fig. 2.44 and Table 2.4). It divides in the upper lumbar region into three vertical columns of muscle, each of which is further subdivided regionally (lumborum, thoracis, cervicis, and capitis), depending on where the muscles attach superiorly.
Table 2.4
Erector spinae group of back muscles
| Muscle | Origin | Insertion |
| Iliocostalis lumborum | Sacrum, spinous processes of lumbar and lower two thoracic vertebrae and their supraspinous ligaments, and the iliac crest | Angles of the lower six or seven ribs |
| Iliocostalis thoracis | Angles of the lower six ribs | Angles of the upper six ribs and the transverse process of CVII |
| Iliocostalis cervicis | Angles of ribs III to VI | Transverse processes of CIV to CVI |
| Longissimus thoracis | Blends with iliocostalis in lumbar region and is attached to transverse processes of lumbar vertebrae | Transverse processes of all thoracic vertebrae and just lateral to the tubercles of the lower nine or ten ribs |
| Longissimus cervicis | Transverse processes of upper four or five thoracic vertebrae | Transverse processes of CII to CVI |
| Longissimus capitis | Transverse processes of upper four or five thoracic vertebrae and articular processes of lower three or four cervical vertebrae | Posterior margin of the mastoid process |
| Spinalis thoracis | Spinous processes of TX or TXI to LII | Spinous processes of TI to TVIII (varies) |
| Spinalis cervicis | Lower part of ligamentum nuchae and spinous process of CVII (sometimes TI to TII) | Spinous process of CII (axis) |
| Spinalis capitis | Usually blends with semispinalis capitis | With semispinalis capitis |
 The outer or most laterally placed column of the erector spinae muscles is the iliocostalis, which is associated with the costal elements and passes from the common tendon of origin to multiple insertions into the angles of the ribs and the transverse processes of the lower cervical vertebrae.
The outer or most laterally placed column of the erector spinae muscles is the iliocostalis, which is associated with the costal elements and passes from the common tendon of origin to multiple insertions into the angles of the ribs and the transverse processes of the lower cervical vertebrae.
 The middle or intermediate column is the longissimus, which is the largest of the erector spinae subdivision extending from the common tendon of origin to the base of the skull. Throughout this vast expanse, the lateral positioning of the longissimus muscle is in the area of the transverse processes of the various vertebrae.
The middle or intermediate column is the longissimus, which is the largest of the erector spinae subdivision extending from the common tendon of origin to the base of the skull. Throughout this vast expanse, the lateral positioning of the longissimus muscle is in the area of the transverse processes of the various vertebrae.
 The most medial muscle column is the spinalis, which is the smallest of the subdivisions and interconnects the spinous processes of adjacent vertebrae. The spinalis is most constant in the thoracic region and is generally absent in the cervical region. It is associated with a deeper muscle (the semispinalis capitis) as the erector spinae group approaches the skull.
The most medial muscle column is the spinalis, which is the smallest of the subdivisions and interconnects the spinous processes of adjacent vertebrae. The spinalis is most constant in the thoracic region and is generally absent in the cervical region. It is associated with a deeper muscle (the semispinalis capitis) as the erector spinae group approaches the skull.
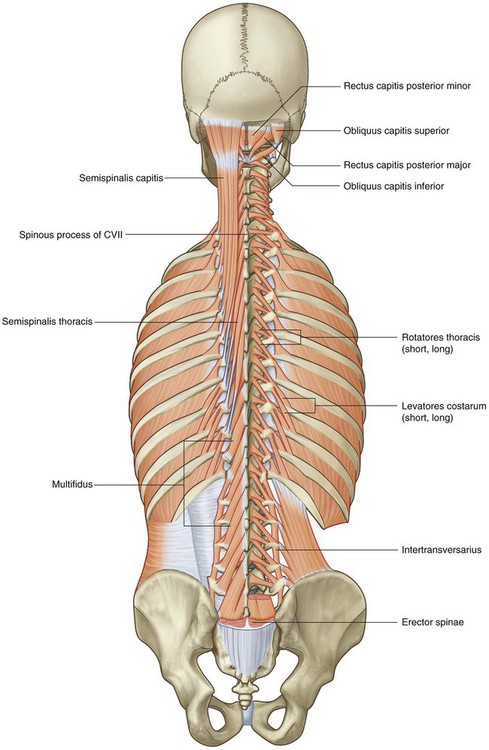
Transversospinales muscles
The transversospinales muscles run obliquely upward and medially from transverse processes to spinous processes, filling the groove between these two vertebral projections (Fig. 2.45 and Table 2.5). They are deep to the erector spinae and consist of three major subgroups—the semispinalis, multifidus, and rotatores muscles.
Table 2.5
Transversospinales group of back muscles
| Muscle | Origin | Insertion |
| Semispinalis thoracis | Transverse processes of TVI to TX | Spinous processes of upper four thoracic and lower two cervical vertebrae |
| Semispinalis cervicis | Transverse processes of upper five or six thoracic vertebrae | Spinous processes of CII (axis) to CV |
| Semispinalis capitis | Transverse processes of TI to TVI (or TVII) and CVII and articular processes of CIV to CVI | Medial area between the superior and inferior nuchal lines of occipital bone |
| Multifidus | Sacrum, origin of erector spinae, posterior superior iliac spine, mammillary processes of lumbar vertebrae, transverse processes of thoracic vertebrae, and articular processes of lower four cervical vertebrae | Base of spinous processes of all vertebrae from LV to CII (axis) |
| Rotatores lumborum | Transverse processes of lumbar vertebrae | Spinous processes of lumbar vertebrae |
| Rotatores thoracis | Transverse processes of thoracic vertebrae | Spinous processes of thoracic vertebrae |
| Rotatores cervicis | Articular processes of cervical vertebrae | Spinous processes of cervical vertebrae |
 The semispinalis muscles are the most superficial collection of muscle fibers in the transversospinales group. These muscles begin in the lower thoracic region and end by attaching to the skull, crossing between four and six vertebrae from their point of origin to point of attachment. Semispinalis muscles are found in the thoracic and cervical regions, and attach to the occipital bone at the base of the skull.
The semispinalis muscles are the most superficial collection of muscle fibers in the transversospinales group. These muscles begin in the lower thoracic region and end by attaching to the skull, crossing between four and six vertebrae from their point of origin to point of attachment. Semispinalis muscles are found in the thoracic and cervical regions, and attach to the occipital bone at the base of the skull.
 Deep to the semispinalis is the second group of muscles, the multifidus. Muscles in this group span the length of the vertebral column, passing from a lateral point of origin upward and medially to attach to spinous processes and spanning between two and four vertebrae. The multifidus muscles are present throughout the length of the vertebral column but are best developed in the lumbar region.
Deep to the semispinalis is the second group of muscles, the multifidus. Muscles in this group span the length of the vertebral column, passing from a lateral point of origin upward and medially to attach to spinous processes and spanning between two and four vertebrae. The multifidus muscles are present throughout the length of the vertebral column but are best developed in the lumbar region.
 The small rotatores muscles are the deepest of the transversospinales group. They are present throughout the length of the vertebral column but are best developed in the thoracic region. Their fibers pass upward and medially from transverse processes to spinous processes crossing two vertebrae (long rotators) or attaching to an adjacent vertebra (short rotators).
The small rotatores muscles are the deepest of the transversospinales group. They are present throughout the length of the vertebral column but are best developed in the thoracic region. Their fibers pass upward and medially from transverse processes to spinous processes crossing two vertebrae (long rotators) or attaching to an adjacent vertebra (short rotators).
Segmental muscles
The two groups of segmental muscles (Fig. 2.45 and Table 2.6) are deeply placed in the back and innervated by posterior rami of spinal nerves.
Table 2.6
| Muscle | Origin | Insertion | Function |
| Levatores costarum | Short paired muscles arising from transverse processes of CVII to TXI | The rib below vertebra of origin near tubercle | Contraction elevates rib |
| Interspinales | Short paired muscles attached to the spinous processes of contiguous vertebrae, one on each side of the interspinous ligament | Postural muscles that stabilize adjoining vertebrae during movements of vertebral column | |
| Intertransversarii | Small muscles between the transverse processes of contiguous vertebrae | Postural muscles that stabilize adjoining vertebrae during movements of vertebral column |
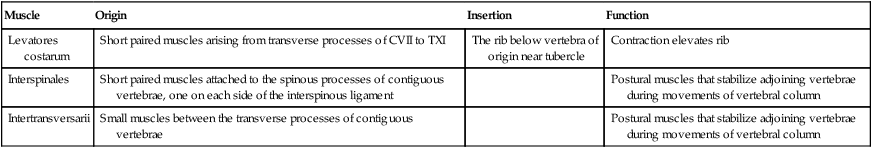
 The first group of segmental muscles are the levatores costarum muscles, which arise from the transverse processes of vertebrae CVII and TI to TXI. They have an oblique lateral and downward direction and insert into the rib below the vertebra of origin in the area of the tubercle. Contraction elevates the ribs.
The first group of segmental muscles are the levatores costarum muscles, which arise from the transverse processes of vertebrae CVII and TI to TXI. They have an oblique lateral and downward direction and insert into the rib below the vertebra of origin in the area of the tubercle. Contraction elevates the ribs.
 The second group of segmental muscles are the true segmental muscles of the back—the interspinales, which pass between adjacent spinous processes, and the intertransversarii, which pass between adjacent transverse processes. These postural muscles stabilize adjoining vertebrae during movements of the vertebral column to allow more effective action of the large muscle groups.
The second group of segmental muscles are the true segmental muscles of the back—the interspinales, which pass between adjacent spinous processes, and the intertransversarii, which pass between adjacent transverse processes. These postural muscles stabilize adjoining vertebrae during movements of the vertebral column to allow more effective action of the large muscle groups.
Suboccipital muscles
A small group of deep muscles in the upper cervical region at the base of the occipital bone move the head. They connect vertebra CI (the atlas) to vertebra CII (the axis) and connect both vertebrae to the base of the skull. Because of their location they are sometimes referred to as suboccipital muscles (Figs. 2.45 and 2.46 and Table 2.7). They include, on each side:
Table 2.7
Suboccipital group of back muscles
| Muscle | Origin | Insertion | Innervation | Function |
| Rectus capitis posterior major | Spinous process of axis (CII) | Lateral portion of occipital bone below inferior nuchal line | Posterior ramus of C1 | Extension of head; rotation of face to same side as muscle |
| Rectus capitis posterior minor | Posterior tubercle of atlas (CI) | Medial portion of occipital bone below inferior nuchal line | Posterior ramus of C1 | Extension of head |
| Obliquus capitis superior | Transverse process of atlas (CI) | Occipital bone between superior and inferior nuchal lines | Posterior ramus of C1 | Extension of head and bends it to same side |
| Obliquus capitis inferior | Spinous process of axis (CII) | Transverse process of atlas (CI) | Posterior ramus of C1 | Rotation of face to same side |
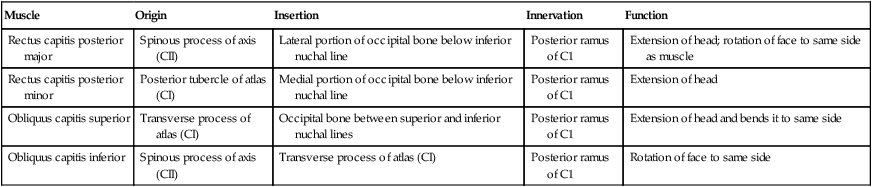
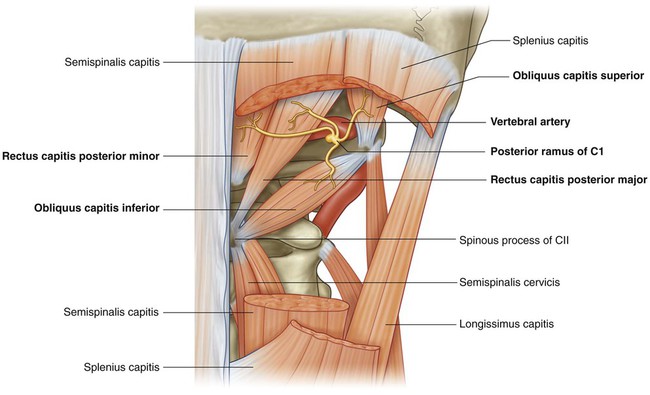
Contraction of the suboccipital muscles extends the head at the atlanto-axial joint.
The suboccipital muscles are innervated by the posterior ramus of the first cervical nerve, which enters the area between the vertebral artery and the posterior arch of the atlas (Fig. 2.46). The vascular supply to the muscles in this area is from branches of the vertebral and occipital arteries.
The suboccipital muscles form the boundaries of the suboccipital triangle, an area that contains several important structures (Fig. 2.46):
Spinal cord
The spinal cord extends from the foramen magnum to approximately the level of the disc between vertebrae LI and LII in adults, although it can end as high as vertebra TXII or as low as the disc between vertebrae LII and LIII (Fig. 2.47). In neonates, the spinal cord extends approximately to vertebra LIII but can reach as low as vertebra LIV. The distal end of the cord (the conus medullaris) is cone shaped. A fine filament of connective tissue (the pial part of the filum terminale) continues inferiorly from the apex of the conus medullaris.
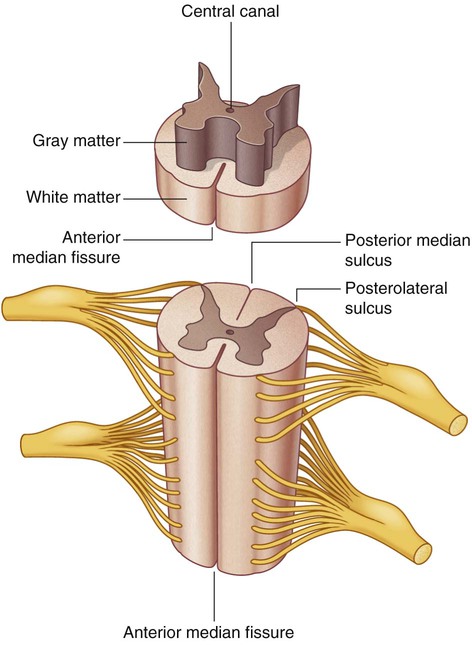
The external surface of the spinal cord is marked by a number of fissures and sulci (Fig. 2.48):
 The anterior median fissure extends the length of the anterior surface.
The anterior median fissure extends the length of the anterior surface.
 The posterior median sulcus extends along the posterior surface.
The posterior median sulcus extends along the posterior surface.
 The posterolateral sulcus on each side of the posterior surface marks where the posterior rootlets of spinal nerves enter the cord.
The posterolateral sulcus on each side of the posterior surface marks where the posterior rootlets of spinal nerves enter the cord.
Internally, the cord has a small central canal surrounded by gray and white matter:
 The gray matter is rich in nerve cell bodies, which form longitudinal columns along the cord, and in cross section these columns form a characteristic H-shaped appearance in the central regions of the cord.
The gray matter is rich in nerve cell bodies, which form longitudinal columns along the cord, and in cross section these columns form a characteristic H-shaped appearance in the central regions of the cord.
 The white matter surrounds the gray matter and is rich in nerve cell processes, which form large bundles or tracts that ascend and descend in the cord to other spinal cord levels or carry information to and from the brain.
The white matter surrounds the gray matter and is rich in nerve cell processes, which form large bundles or tracts that ascend and descend in the cord to other spinal cord levels or carry information to and from the brain.
Vasculature
Arteries
The arterial supply to the spinal cord comes from two sources (Fig. 2.49). It consists of:
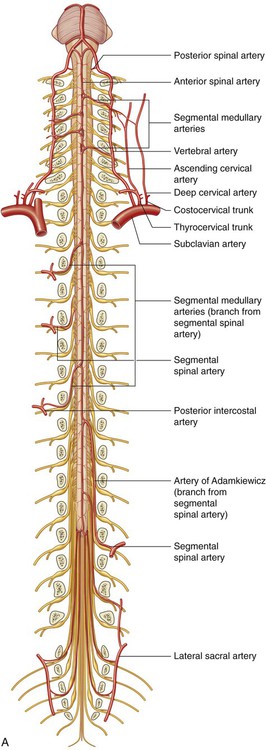
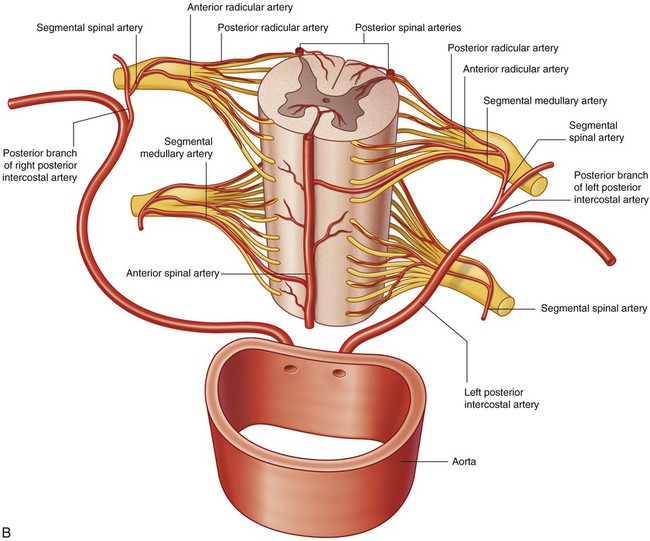
B. Segmental supply of spinal cord.
 longitudinally oriented vessels, arising superior to the cervical portion of the cord, which descend on the surface of the cord; and
longitudinally oriented vessels, arising superior to the cervical portion of the cord, which descend on the surface of the cord; and
 feeder arteries that enter the vertebral canal through the intervertebral foramina at every level; these feeder vessels, or segmental spinal arteries, arise predominantly from the vertebral and deep cervical arteries in the neck, the posterior intercostal arteries in the thorax, and the lumbar arteries in the abdomen.
feeder arteries that enter the vertebral canal through the intervertebral foramina at every level; these feeder vessels, or segmental spinal arteries, arise predominantly from the vertebral and deep cervical arteries in the neck, the posterior intercostal arteries in the thorax, and the lumbar arteries in the abdomen.
After entering an intervertebral foramen, the segmental spinal arteries give rise to anterior and posterior radicular arteries (Fig. 2.49). This occurs at every vertebral level. The radicular arteries follow, and supply, the anterior and posterior roots. At various vertebral levels, the segmental spinal arteries also give off segmental medullary arteries (Fig. 2.49). These vessels pass directly to the longitudinally oriented vessels, reinforcing these.
The longitudinal vessels consist of:
 a single anterior spinal artery, which originates within the cranial cavity as the union of two vessels that arise from the vertebral arteries—the resulting single anterior spinal artery passes inferiorly, approximately parallel to the anterior median fissure, along the surface of the spinal cord; and
a single anterior spinal artery, which originates within the cranial cavity as the union of two vessels that arise from the vertebral arteries—the resulting single anterior spinal artery passes inferiorly, approximately parallel to the anterior median fissure, along the surface of the spinal cord; and
 two posterior spinal arteries, which also originate in the cranial cavity, usually arising directly from a terminal branch of each vertebral artery (the posterior inferior cerebellar artery)—the right and left posterior spinal arteries descend along the spinal cord, each as two branches that bracket the posterolateral sulcus and the connection of posterior roots with the spinal cord.
two posterior spinal arteries, which also originate in the cranial cavity, usually arising directly from a terminal branch of each vertebral artery (the posterior inferior cerebellar artery)—the right and left posterior spinal arteries descend along the spinal cord, each as two branches that bracket the posterolateral sulcus and the connection of posterior roots with the spinal cord.
The anterior and posterior spinal arteries are reinforced along their length by eight to ten segmental medullary arteries (Fig. 2.49). The largest of these is the arteria radicularis magna or the artery of Adamkiewicz (Fig. 2.49). This vessel arises in the lower thoracic or upper lumbar region, usually on the left side, and reinforces the arterial supply to the lower portion of the spinal cord, including the lumbar enlargement.
Veins
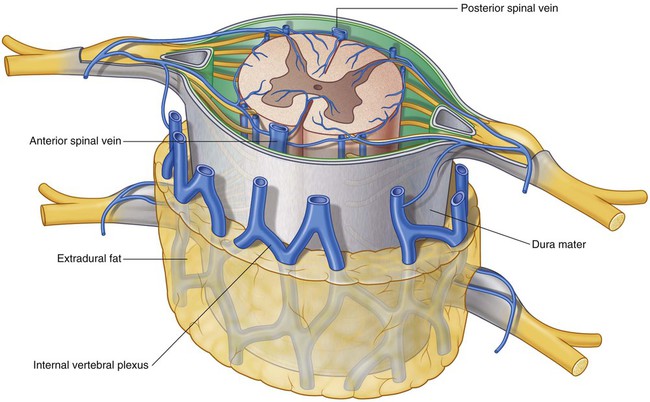
Veins that drain the spinal cord form a number of longitudinal channels (Fig. 2.50):
Meninges
Spinal dura mater
The spinal dura mater is the outermost meningeal membrane and is separated from the bones forming the vertebral canal by an extradural space (Fig. 2.51). Superiorly, it is continuous with the inner meningeal layer of cranial dura mater at the foramen magnum of the skull. Inferiorly, the dural sac dramatically narrows at the level of the lower border of vertebra SII and forms an investing sheath for the pial part of the filum terminale of the spinal cord. This terminal cord-like extension of dura mater (the dural part of the filum terminale) attaches to the posterior surface of the vertebral bodies of the coccyx.
Subarachnoid space
The subarachnoid space between the arachnoid and pia mater contains CSF (Fig. 2.51). The subarachnoid space around the spinal cord is continuous at the foramen magnum with the subarachnoid space surrounding the brain. Inferiorly, the subarachnoid space terminates at approximately the level of the lower border of vertebra SII (see Fig. 2.47).
The subarachnoid space extends further inferiorly than the spinal cord. The spinal cord ends at approximately the disc between vertebrae LI and LII, whereas the subarachnoid space extends to approximately the lower border of vertebra SII (see Fig. 2.47). The subarachnoid space is largest in the region inferior to the terminal end of the spinal cord, where it surrounds the cauda equina. As a consequence, CSF can be withdrawn from the subarachnoid space in the lower lumbar region without endangering the spinal cord.
Pia mater
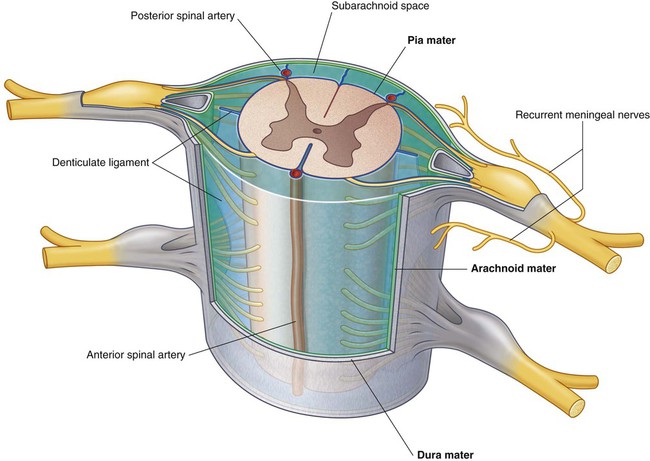
The spinal pia mater is a vascular membrane that firmly adheres to the surface of the spinal cord (Fig. 2.51). It extends into the anterior median fissure and reflects as sleeve-like coatings onto posterior and anterior rootlets and roots as they cross the subarachnoid space. As the roots exit the space, the sleeve-like coatings reflect onto the arachnoid mater.
On each side of the spinal cord, a longitudinally oriented sheet of pia mater (the denticulate ligament) extends laterally from the cord toward the arachnoid and dura mater (Fig. 2.51).
 Medially, each denticulate ligament is attached to the spinal cord in a plane that lies between the origins of the posterior and anterior rootlets.
Medially, each denticulate ligament is attached to the spinal cord in a plane that lies between the origins of the posterior and anterior rootlets.
 Laterally, each denticulate ligament forms a series of triangular extensions along its free border, with the apex of each extension being anchored through the arachnoid mater to the dura mater.
Laterally, each denticulate ligament forms a series of triangular extensions along its free border, with the apex of each extension being anchored through the arachnoid mater to the dura mater.
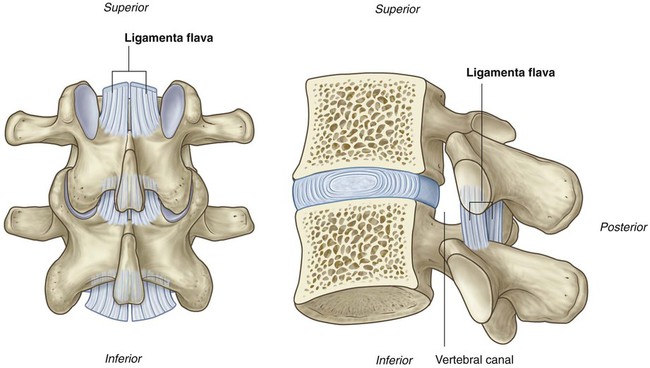
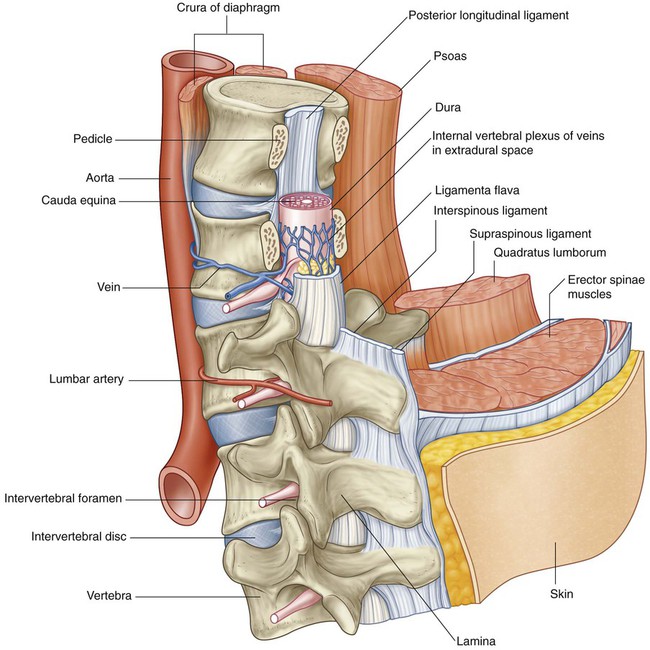
Arrangement of structures in the vertebral canal
The vertebral canal is bordered:
 anteriorly by the bodies of the vertebrae, intervertebral discs, and posterior longitudinal ligament (Fig. 2.52);
anteriorly by the bodies of the vertebrae, intervertebral discs, and posterior longitudinal ligament (Fig. 2.52);
 laterally, on each side by the pedicles and intervertebral foramina; and
laterally, on each side by the pedicles and intervertebral foramina; and
 posteriorly by the laminae and ligamenta flava, and in the median plane the roots of the interspinous ligaments and vertebral spinous processes.
posteriorly by the laminae and ligamenta flava, and in the median plane the roots of the interspinous ligaments and vertebral spinous processes.
Spinal nerves
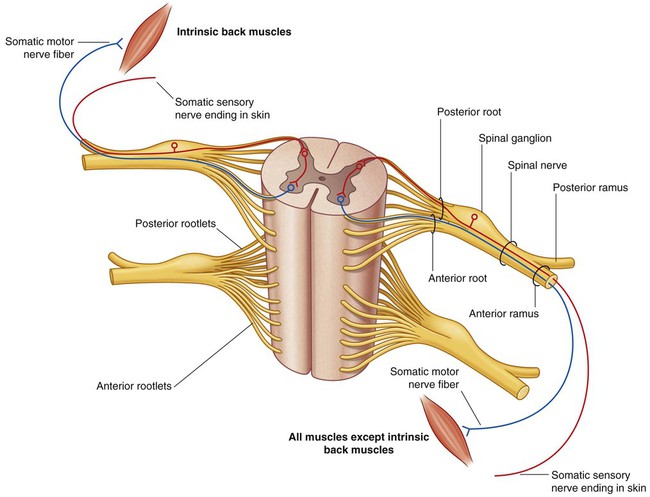
Each spinal nerve is connected to the spinal cord by posterior and anterior roots (Fig. 2.53):
 The posterior root contains the processes of sensory neurons carrying information to the CNS—the cell bodies of the sensory neurons, which are derived embryologically from neural crest cells, are clustered in a spinal ganglion at the distal end of the posterior root, usually in the intervertebral foramen.
The posterior root contains the processes of sensory neurons carrying information to the CNS—the cell bodies of the sensory neurons, which are derived embryologically from neural crest cells, are clustered in a spinal ganglion at the distal end of the posterior root, usually in the intervertebral foramen.
 The anterior root contains motor nerve fibers, which carry signals away from the CNS—the cell bodies of the primary motor neurons are in anterior regions of the spinal cord.
The anterior root contains motor nerve fibers, which carry signals away from the CNS—the cell bodies of the primary motor neurons are in anterior regions of the spinal cord.
Medially, the posterior and anterior roots divide into rootlets, which attach to the spinal cord.
Each spinal nerve divides, as it emerges from an intervertebral foramen, into two major branches: a small posterior ramus and a much larger anterior ramus (Fig. 2.53):
 The posterior rami innervate only intrinsic back muscles (the epaxial muscles) and an associated narrow strip of skin on the back.
The posterior rami innervate only intrinsic back muscles (the epaxial muscles) and an associated narrow strip of skin on the back.
 The anterior rami innervate most other skeletal muscles (the hypaxial muscles) of the body, including those of the limbs and trunk, and most remaining areas of the skin, except for certain regions of the head.
The anterior rami innervate most other skeletal muscles (the hypaxial muscles) of the body, including those of the limbs and trunk, and most remaining areas of the skin, except for certain regions of the head.
Near the point of division into anterior and posterior rami, each spinal nerve gives rise to two to four small recurrent meningeal (sinuvertebral) nerves (see Fig. 2.51). These nerves reenter the intervertebral foramen to supply dura, ligaments, intervertebral discs, and blood vessels.
All major somatic plexuses (cervical, brachial, lumbar, and sacral) are formed by anterior rami.
Because the spinal cord is much shorter than the vertebral column, the roots of spinal nerves become longer and pass more obliquely from the cervical to coccygeal regions of the vertebral canal (Fig. 2.54).
Nomenclature of spinal nerves
There are approximately 31 pairs of spinal nerves (Fig. 2.54), named according to their position with respect to associated vertebrae:
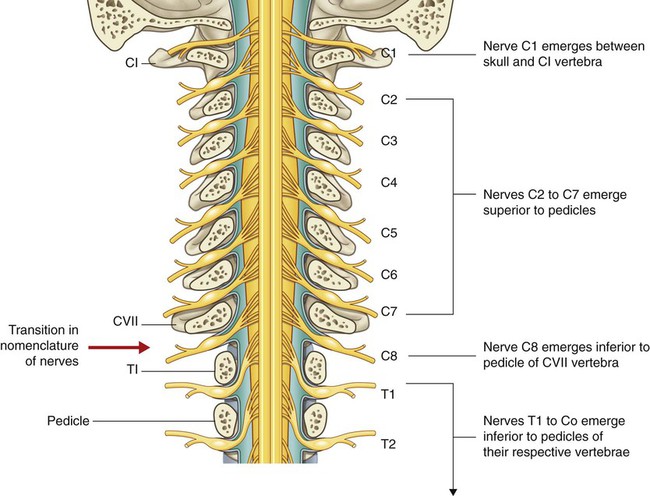
The first cervical nerve (C1) emerges from the vertebral canal between the skull and vertebra CI (Fig. 2.55). Therefore cervical nerves C2 to C7 also emerge from the vertebral canal above their respective vertebrae. Because there are only seven cervical vertebrae, C8 emerges between vertebrae CVII and TI. As a consequence, all remaining spinal nerves, beginning with T1, emerge from the vertebral canal below their respective vertebrae.
Surface anatomy
Primary and secondary curvatures in the sagittal plane
When viewed from the side, the normal vertebral column has primary curvatures in the thoracic and sacral/coccygeal regions and secondary curvatures in the cervical and lumbar regions (Fig. 2.57). The primary curvatures are concave anteriorly. The secondary curvatures are concave posteriorly.
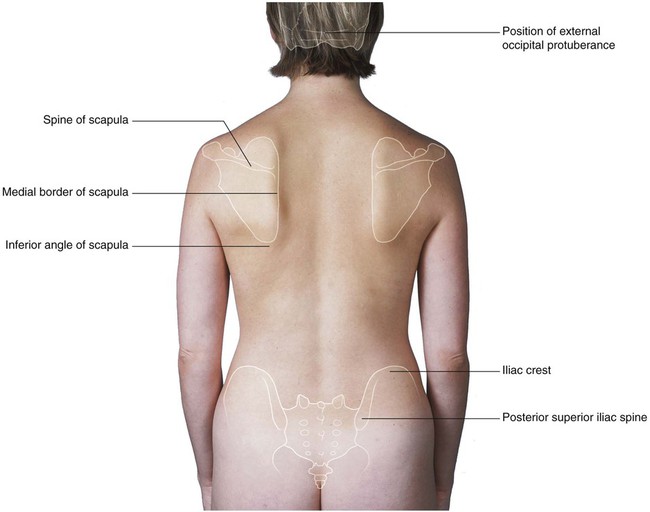
Useful nonvertebral skeletal landmarks
A number of readily palpable bony features provide useful landmarks for defining muscles and for locating structures associated with the vertebral column. Among these features are the external occipital protuberance, the scapula, and the iliac crest (Fig. 2.58).
How to identify specific vertebral spinous processes
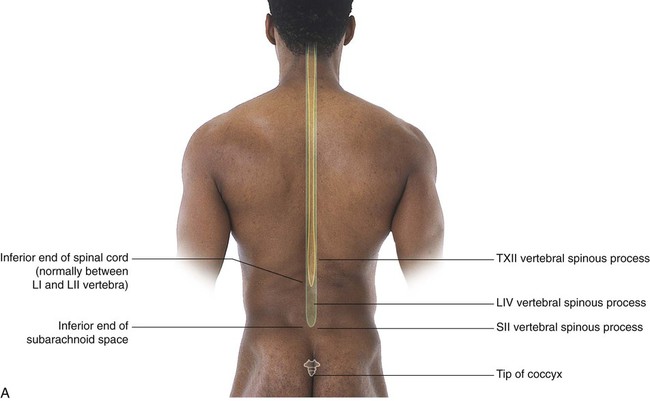
Identification of vertebral spinous processes (Fig. 2.59A) can be used to differentiate between regions of the vertebral column and facilitate visualizing the position of deeper structures, such as the inferior ends of the spinal cord and subarachnoid space.
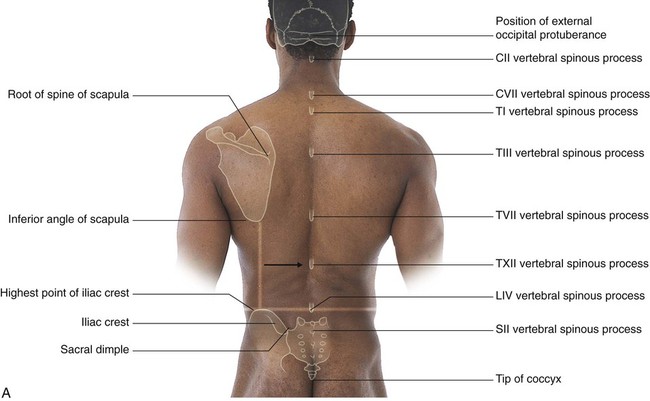
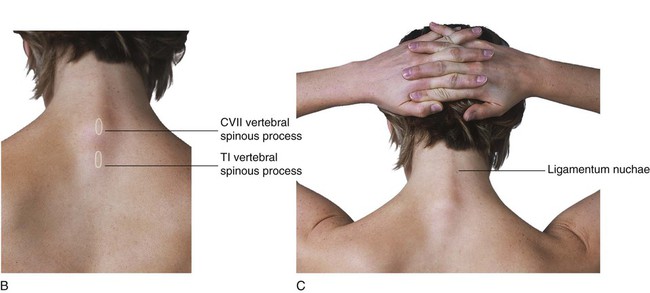
The spinous process of CVII is usually visible as a prominent eminence in the midline at the base of the neck (Fig. 2.59B), particularly when the neck is flexed.
Extending between CVII and the external occipital protuberance of the skull is the ligamentum nuchae, which is readily apparent as a longitudinal ridge when the neck is flexed (Fig. 2.59C).
Inferior to the spinous process of CVII is the spinous process of TI, which is also usually visible as a midline protuberance. Often it is more prominent than the spinous process of CVII (Fig. 2.59A,B).
The root of the spine of the scapula is at the same level as the spinous process of vertebra TIII, and the inferior angle of the scapula is level with the spinous process of vertebra TVII (Fig. 2.59A).
The spinous process of vertebra TXII is level with the midpoint of a vertical line between the inferior angle of the scapula and the iliac crest (Fig. 2.59A).
A horizontal line between the highest point of the iliac crest on each side crosses through the spinous process of vertebra LIV. The LIII and LV vertebral spinous processes can be palpated above and below the LIV spinous process, respectively (Fig. 2.59A).
The sacral dimples that mark the position of the posterior superior iliac spine are level with the SII vertebral spinous process (Fig. 2.59A).
The tip of the coccyx is palpable at the base of the vertebral column between the gluteal masses (Fig. 2.59A).
Visualizing the inferior ends of the spinal cord and subarachnoid space
The spinal cord does not occupy the entire length of the vertebral canal. Normally in adults, it terminates at the level of the disc between vertebrae LI and LII; however, it may end as high as TXII or as low as the disc between vertebrae LII and LIII. The subarachnoid space ends at approximately the level of vertebra SII (Fig. 2.60A).
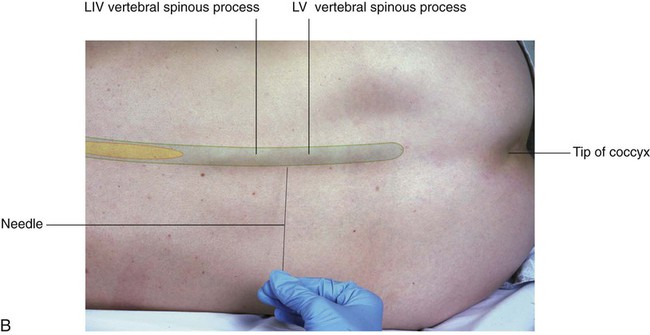
Back with the ends of the spinal cord and subarachnoid space indicated. B. In a woman lying on her side in a fetal position, which accentuates the lumbar vertebral spinous processes and opens the spaces between adjacent vertebral arches. Cerebrospinal fluid can be withdrawn from the subarachnoid space in lower lumbar regions without endangering the spinal cord.
Because the subarachnoid space can be accessed in the lower lumbar region without endangering the spinal cord, it is important to be able to identify the position of the lumbar vertebral spinous processes. The LIV vertebral spinous process is level with a horizontal line between the highest points on the iliac crests. In the lumbar region, the palpable ends of the vertebral spinous processes lie opposite their corresponding vertebral bodies. The subarachnoid space can be accessed between vertebral levels LIII and LIV and between LIV and LV without endangering the spinal cord (Fig. 2.60B). The subarachnoid space ends at vertebral level SII, which is level with the sacral dimples marking the posterior superior iliac spines.
Identifying major muscles
A number of intrinsic and extrinsic muscles of the back can readily be observed and palpated. The largest of these are the trapezius and latissimus dorsi muscles (Fig. 2.61A and 2.61B). Retracting the scapulae toward the midline can accentuate the rhomboid muscles (Fig. 2.61C), which lie deep to the trapezius muscle. The erector spinae muscles are visible as two longitudinal columns separated by a furrow in the midline (Fig. 2.61A).