32 Axillary Block
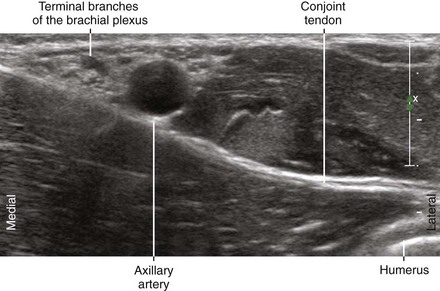
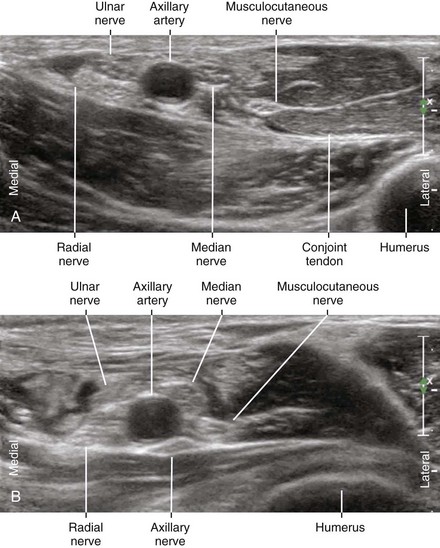
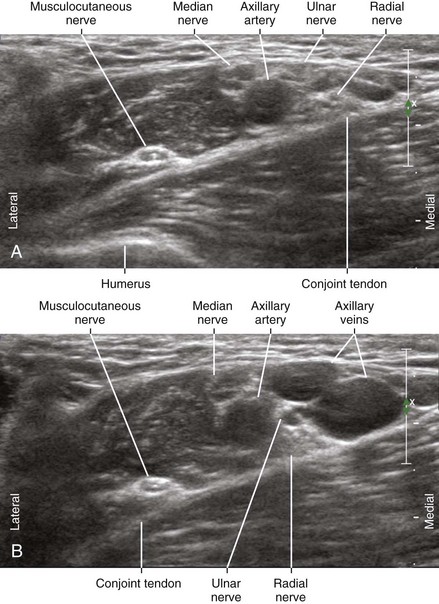
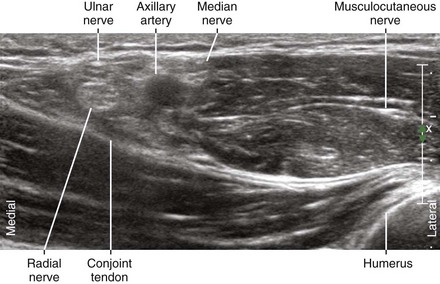
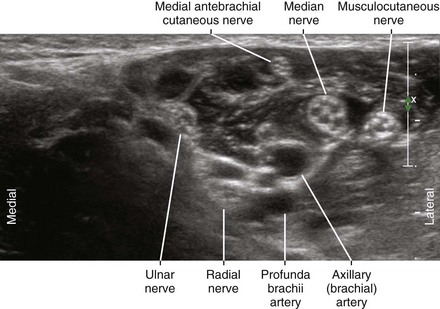
Three terminal branches of the brachial plexus (the median, radial, and ulnar nerves) lie close to the axillary artery in the axilla (Table 32-1). This makes the axilla a convenient place to block the brachial plexus (Table 32-2). Axillary block is traditionally performed by transarterial injection of local anesthetic around the axillary artery or by use of nerve stimulation to evoke motor responses. Transarterial block necessitates puncturing the axillary artery. Another weakness is failure to anesthetize the musculocutaneous nerve, which leaves the neurovascular bundle proximally underneath the pectoralis minor muscle at the level of the coracoid process.
Table 32-1 Characteristics of Terminal Branches of the Brachial Plexus in the Axilla
| Nerve | Characteristics |
|---|---|
| Axillary |
Table 32-2 Clinical Considerations for Axillary Block with Ultrasound
| Advantages | Disadvantages |
|---|---|
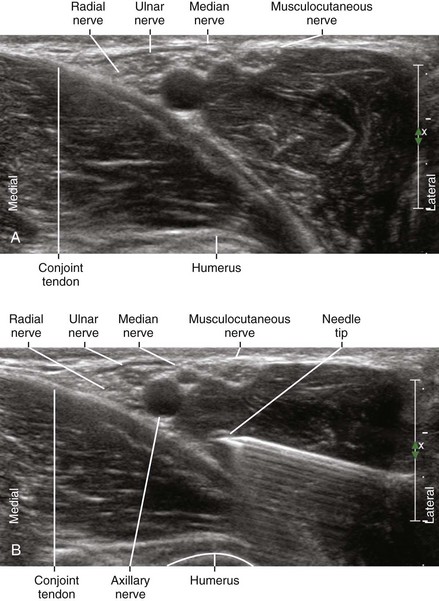
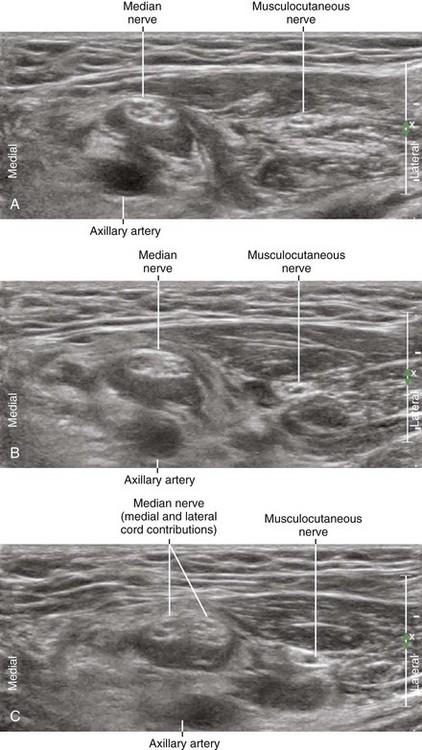
Ultrasound imaging improves axillary block of the brachial plexus. Almost all institutions have reported advantages to using ultrasound to guide this procedure.1,2 Ultrasound can be used to guide injections around the axillary artery. In addition, the musculocutaneous nerve can be directly imaged to complete the axillary block (see Chapter 33).
Suggested Technique
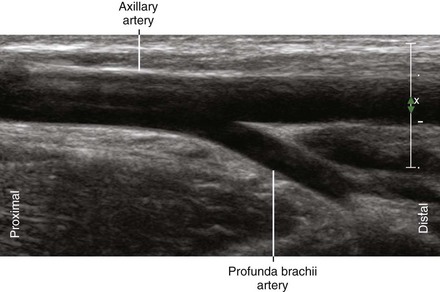
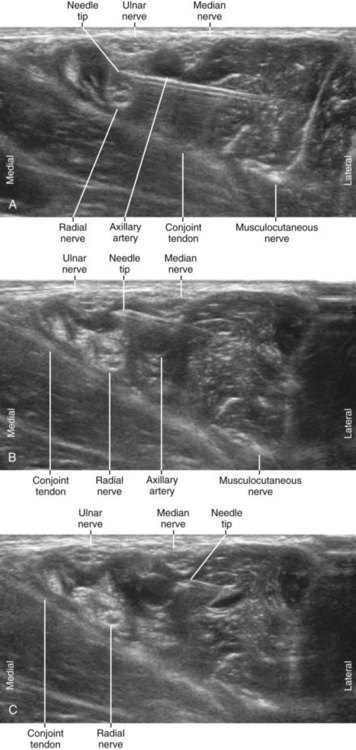
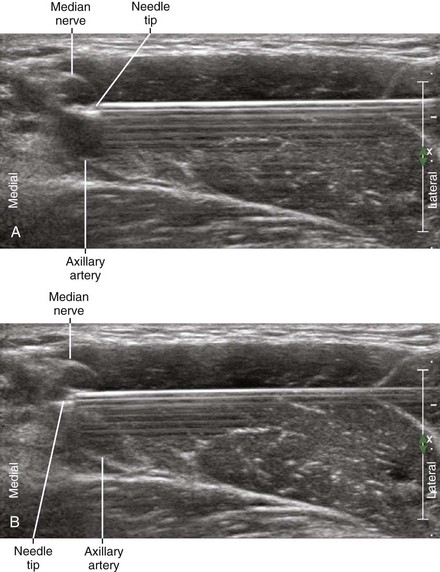
Local anesthetic injections are made in front and in back of the axillary artery. The injection in back of the artery is typically done first. This brings the neurovascular bundle even closer to the skin surface. The musculocutaneous nerve is blocked separately (see Chapter 33).
Key Points
| Axillary Block | The Essential Points |
|---|---|
| Anatomy | There are three wall-hugging nerves in the axilla (MN, RN, UN). |
| All terminal branches lie superficial to the CT in the axilla (MN, RN, UN, MCN). | |
| The nerves are about 3 mm in diameter. | |
| Image orientation | The CT has a medial (superficial) to lateral (deep) inclination. |
| Positioning | Supine, with arm abducted |
| A blue foam headrest provides working room. | |
| Operator | Standing on the lateral (cephalad) side of armboard (for laptop system) |
| At the side of the patient (for system with movable display) | |
| Display | Across the armboard (for laptop system) |
| Across the table (for system with movable display) | |
| Transducer | High-frequency linear, 23- to 38-mm footprint |
| Initial depth setting | 25 mm |
| Needle | 20 to 21 gauge, 70 mm in length |
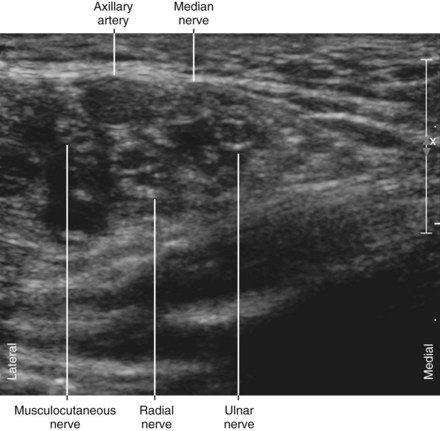
| Anatomic location | Begin by scanning the axilla to identify the AA in SAX view. |
| Slide transducer to obtain view of CT underneath AA | |
| Approach | SAX view of AA, in-plane from lateral to medial |
| Place the needle tip between the nerves and AA. | |
| Sonographic assessment | The injections should separate the nerves from artery. |
| Anatomic variation | MCN-median fusion (5%-10%). The MCN can be fused with the median nerve in the axilla. This is sometimes referred to as a low-lying lateral cord. |
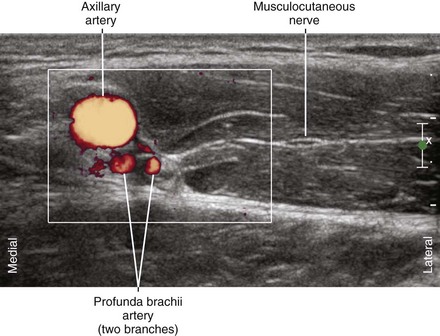
| Duplicate axillary artery can occasionally be seen. |
Clinical Pearls
• With this proximal approach to axillary block, the needle is naturally channeled into the space between the axillary artery and conjoint tendon of the latissimus dorsi and teres major for the posterior injection. A slight upward trajectory is all that is needed to steer the needle along and above this tendon complex.
• With classic approaches to axillary block, the radial nerve and musculocutaneous nerves are often spared.3
1 Soeding PE, Sha S, Royse CE, et al. A randomized trial of ultrasound-guided brachial plexus anaesthesia in upper limb surgery. Anaesth Intensive Care. 2005;33:719–725.
2 Lo N, Brull R, Perlas A, et al. Evolution of ultrasound guided axillary brachial plexus blockade: retrospective analysis of 662 blocks. Can J Anaesth. 2008;55:408–413.
3 Lanz E, Theiss D, Jankovic D. The extent of blockade following various techniques of brachial plexus block. Anesth Analg. 1983;62:55–58.