Chapter 22 Autoimmune connective tissue diseases
Lupus patients also develop many skin changes that are not specific for LE, termed lupus-nonspecific eruptions (Table 22-1). These eruptions do not help to establish a diagnosis of LE, but they may still be very important to note, as specific systemic findings may be associated with them. For example, cutaneous lesions of palpable purpura in a patient with LE are not lupus-specific, that is, such lesions may be seen in patients who do not have LE; however, they may be associated with vasculitic lesions of the kidney or central nervous system (CNS), and thus they have significance in the evaluation and treatment of lupus.
Table 22-1. Classification of Cutaneous Disease in Lupus Erythematosus
| LUPUS-SPECIFIC ERUPTIONS | LUPUS-NONSPECIFIC ERUPTIONS |
|---|---|

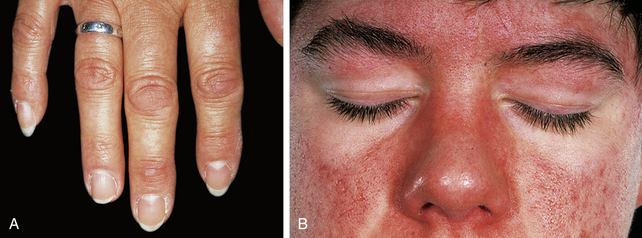
Figure 22-1. Acute cutaneous lupus erythematosus. Note the classic malar erythema (“butterfly rash”).
Wozniacka A, McCauliffe DP: Optimal use of antimalarials in treating cutaneous lupus erythematosus, Am J Clin Dermatol 6:1–11, 2005.
Fraga J, García-Díez A: Lupus erythematosus panniculitis, Dermatol Clin 26:453–463, 2008.
Lee LA: Neonatal lupus erythematosus, J Invest Dermatol 100:9S–13S, 1993.
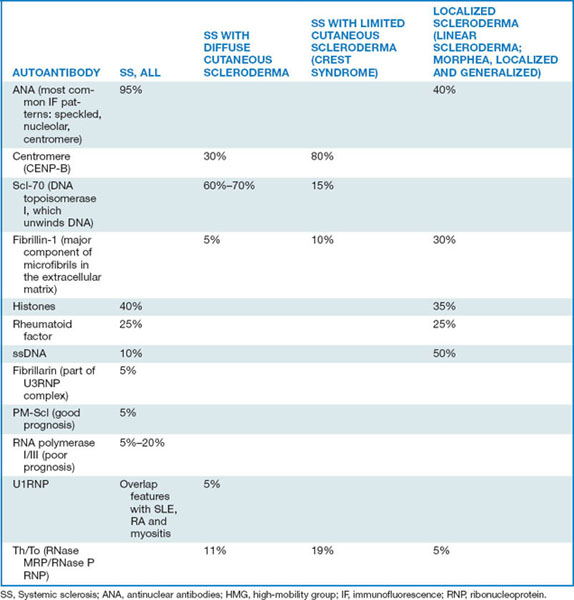
CREST syndrome, or Thibierge-Weissenbach syndrome, is generally considered a type of limited systemic sclerosis. In addition to the cutaneous changes of calcinosis cutis, Raynaud’s phenomenon, sclerodactyly, and telangiectasia, these patients often develop hyperpigmentation, particularly in sun-exposed areas (Fig. 22-7). Most patients with the CREST syndrome have circulating antibodies to centromeres, called anticentromere antibodies.
Callen JP, Wortmann RL: Dermatomyositis, Clin Dermatol 24:363–373, 2006.
Key Points: Dermatomyositis
Venables PJ: Mixed connective tissue disease, Lupus 15:132–137, 2006.