Chapter 17 Atrioventricular Conduction Abnormalities Delays, Blocks, and Dissociation Syndromes
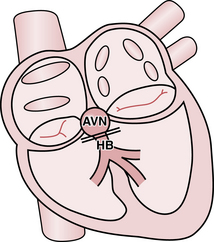
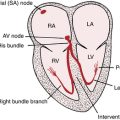
With normal cardiac anatomy (see Chapter 1), the only means of electrical communication between the atria and ventricles is via the specialized conduction system of the heart. This relay network comprises the atrioventricular (AV) node, which is connected to the His bundle, which in turn is connected to the bundle branches (Fig. 17-1). The atria and ventricles are otherwise electrically isolated from each other by connective tissue in the indented rings (grooves) between the upper and lower chambers. The key exception occurs with Wolff-Parkinson-White (WPW) preexcitation syndrome, described in Chapters 12 and 14.
The slight physiologic delay, reflected in the normal PR interval, between atrial and ventricular activation allows the ventricles optimal time to fill with blood during and after atrial contraction. Excessive slowing or actual interruption of electrical signal propagation across the heart’s conduction system is abnormal and termed AV (atrioventricular) block or heart block. The closely related (and often confusing to students and experienced clinicians!) topic of AV dissociation is discussed at the end of this chapter and in Chapter 10.
What is the Degree of AV Block?
Depending on the severity of conduction impairment, there are three major degrees of AV block:
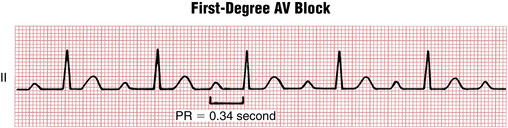
• First-degree (PR interval prolongation): uniform slowing of conduction between the atria and ventricles (an increase in the normal AV delay described earlier), but without its interruption
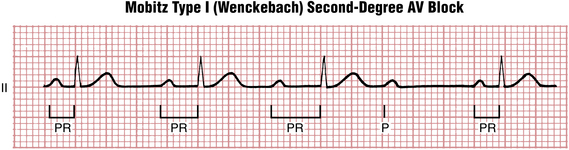
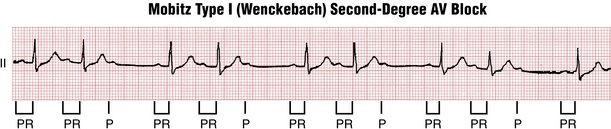
• Second-degree: intermittent interruption of conduction, which may be further designated as Mobitz I (AV Wenckebach) or Mobitz II varieties
• Third-degree: complete interruption of AV conduction, with a nodal or infranodal escape rhythm, or with asystole
Two other important subtypes of second-degree AV block, namely 2:1 block and high-grade block (also referred to as “advanced second-degree AV block”) will also be discussed.
Prolonged PR Interval (First-Degree AV Block)
First-degree AV block (Fig. 17-2) is characterized by a P wave (usually sinus in origin) followed by a QRS complex with a uniformly prolonged PR interval greater than 200 msec. The preferred term is PR interval prolongation because the signal is not really blocked, but rather it is delayed. The PR interval can be slightly prolonged (e.g., 240 msec) or it can become markedly long (up to 400 msec or longer).
Second-Degree AV Block Syndromes
With Mobitz type I, the classic AV Wenckebach pattern (Figs. 17-3 and 17-4), each stimulus from the atria has progressive difficulty traversing the AV node to the ventricles (i.e., the node becomes increasingly refractory). Finally, the atrial stimulus is not conducted at all, such that the expected QRS complex is blocked (“dropped QRS”). This cycle is followed by relative recovery of the AV junction, and then the whole cycle starts again.
The number of P waves occurring before a QRS complex is “dropped” may vary. The nomenclature is in terms of a ratio that gives the number of P waves to QRS complexes in a given cycle. The numerator is always one higher than the denominator. In many cases just two or three conducted P waves are seen before one is not conducted (e.g., 3:2, 4:3 block). In other cases, longer cycles are seen (e.g., 5:4, 10:9, etc.).∗
As you can see from the examples, the Wenckebach cycle also produces a distinct clustering of QRS complexes separated by a pause (the dropped beat). Any time you encounter an ECG with this type of group beating, you should suspect AV Wenckebach block and look for the diagnostic pattern of lengthening PR intervals and the presence of a nonconducted P wave. As discussed in the following text, infranodal second-degree AV block (Mobitz type II) also demonstrates grouped beating with dropped QRS complexes, but without significant progressive PR interval prolongation (Fig. 17-5).
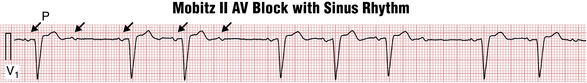
Figure 17-5 Mobitz type II atrioventricular (AV) second-degree heart block. Lead V1 recording shows sinus rhythm (P wave; arrows) at a rate of about 75 beats/min (with left atrial abnormality). Most important, note the abrupt appearance of sinus P waves that are not followed by QRS complexes (nonconducted or “dropped” beats). Furthermore, the PR interval before the nonconducted P wave and the PR of the beat after (about 0.14 sec) are the same. This finding contrasts with AV Wenckebach with 3:2 or higher ratios of conduction in which the PR interval after the nonconducted beat is noticeably shorter than the one before (see Figs. 17-3 and 17-4). The QRS of the conducted beats is also wide because of a left ventricular conduction delay. Mobiz II block is often associated with bundle branch abnormalities because the conduction delay is infranodal. Finally, note that the intermittent AV conduction pattern here gives rise to “group beating,” also a feature of AV Wenckebach block.
Caution! Be careful not to mistake group beating due to blocked atrial premature beats (APBs) for second-degree AV block. In the former, the nonconducted P waves come “early”; in the latter they come “on time” (see Chapter 14).
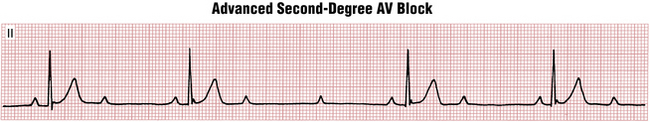
A subset of second-degree heart block occurs when there are multiple consecutive nonconducted P waves present (e.g., P-QRS ratios of 3:1, 4:1, etc.). This finding is referred to as high-degree (or advanced) AV block. It can occur at any level of the conduction system (Fig. 17-6). A common mistake is to call this pattern Mobitz II block.
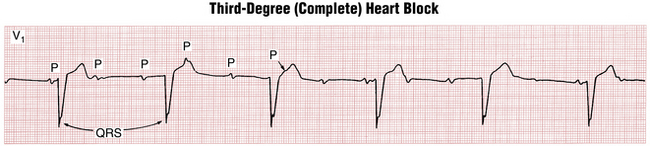
Third-Degree (Complete) AV Block
First- and second-degree heart blocks are examples of incomplete block because the AV junction conducts some stimuli to the ventricles. With third-degree, or complete, heart block, no stimuli are transmitted from the atria to the ventricles. Instead, the atria and ventricles are paced independently. The atria often continue to be paced by the sinoatrial (SA) node. The ventricles, however, are paced by a nodal or infranodal escape pacemaker located somewhere below the point of block. The resting ventricular rate with complete heart block may be around 30 beats/min or lower or as high as 50 to 60 beats/min. This situation, when there is no “cross-talk” between the atria and ventricles and each of them is driven independently by a separate pacemaker at a different rate, is one example of AV dissociation. In the setting of complete heart block, AV dissociation almost always produces more P waves than QRS complexes (Box 17-1). However, as discussed later, AV dissociation is not unique to complete heart block.
BOX 17-1 ECG with Sinus Rhythm and Complete Heart Block: Three Key Features
• P waves (upright in lead II) are present, with a relatively regular sinus rate that is typically much faster than the ventricular rate.
• QRS complexes are present, with a slow (usually near-constant) ventricular rate.
• The P waves bear no relation to the QRS complexes; thus, the PR intervals are variable.
Examples of complete heart block are shown in Figures 17-7 and 17-8.
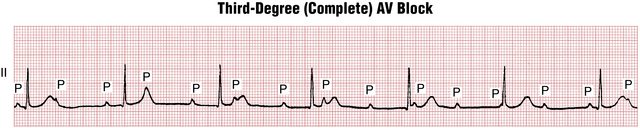
Figure 17-7 Complete heart block is characterized by independent atrial (P) and ventricular (QRS complex) activity. The atrial rate (sinus rate, here) is always faster than the ventricular rate. The PR intervals are completely variable. Some sinus P waves fall on the T wave, distorting its shape. Others may fall in the QRS complex and be “lost.” Notice that the QRS complexes are of normal width, indicating that the ventricles are being paced from the atrioventricular junction. Compare this example with Figure 17-8, which shows complete heart block with wide, very slow QRS complexes because the ventricles are most likely being paced from below the atrioventricular junction (idioventricular pacemaker).
Complete heart block may also occur in patients whose basic atrial rhythm is flutter or fibrillation. In these cases, the ventricular rate is very slow and almost completely regular (see Fig. 15-8).
What is the Location of the Block? Nodal Vs. Infranodal
Interruption of electrical conduction (see Fig. 17-1) can occur at any level starting from the AV node itself (“nodal block”) down to the His bundle and its branches (“infranodal” block). Although the AV node and infranodal structures represent a single, continuous “electrical wire,” their physiology is quite different. These differences often allow you to localize the level of block (nodal vs. infranodal), which has important clinical implications.
In general, block at the level of the AV node:
• Is often caused by reversible factors (Box 17-2)
• Progresses more slowly, if at all
• In the case of complete heart block, is associated with a relatively stable escape rhythm
BOX 17-2 Some Conditions That May Cause Temporary AV Conduction Impairment
• Autonomic factors (increased vagal tone with vasovagal syncope or sleep apnea). Trained athletes at rest may show a prolonged atrioventricular (AV) interval and even AV Wenckebach with sinus bradycardia that resolve with exercise.
• Medications (especially, beta blockers; digoxin, certain calcium channel blockers) and electrolyte abnormalities (especially hyperkalemia)
• Acute myocardial infarction, especially inferior (see text discussion)
• Inflammatory processes (e.g., myocarditis, rheumatic fever, lupus)
In contrast, infranodal block:
• Is usually irreversible (Box 17-3)
• May progress rapidly and unexpectedly to complete heart block with a slow, unstable escape mechanism
BOX 17-3 Some Causes of Permanent AV Conduction System Damage
• Acute myocardial infarction, especially anterior wall
• Infiltrative diseases (e.g., amyloid, sarcoid, lymphomas)
• Degeneration of the conduction system, usually with advanced age (Lenègre’s disease) or associated with cardiac calcification around the aortic and mitral valves (Lev’s disease)
• Hereditary neuromuscular diseases (e.g., myotonic dystrophy, Kearns-Sayre syndrome, Erb’s dystrophy)
• Iatrogenic damage to the conduction system as the result of valve surgery or arrhythmia ablations in the area of atrioventricular (AV) node and His bundle; ethanol septal ablation for obstructive hypertrophic cardiomyopathy
Therefore, infranodal block (even second-degree) generally requires pacemaker implantation.
Clues to nodal versus infranodal mechanisms of AV block include the following:
• Onset and progression of block
• Autonomic and drug influences
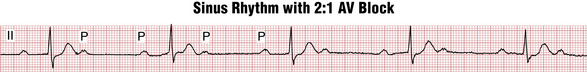
2:1 AV Block: A Special and Often Confusing Subtype of Second-Degree Heart Block
2:1 AV block occurs when every other QRS complex is “dropped” or, equivalently, every other P wave is not conducted. In such cases, it becomes difficult or impossible from the surface ECG to tell Mobitz I from Mobitz II type block simply because there are not two consecutive conducted PR intervals to compare with the subsequent nonconducted one. Very prolonged PR interval in conducted beats (>280 msec) strongly suggests nodal (type I) block (Fig. 17-9), although a relatively short PR interval (≤140 msec), especially in association with QRS widening, suggests infranodal (type II) block (Fig. 17-10). Intermediate values are not diagnostic.∗
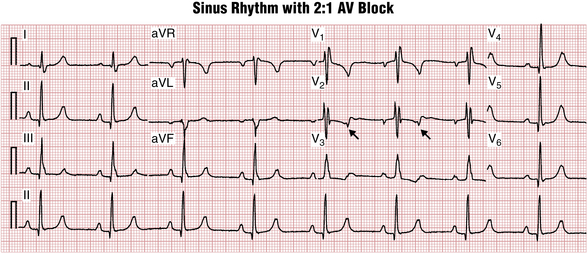
Figure 17-10 Sinus rhythm with 2:1 atrioventricular (AV) block. In this case, compared with Figure 17-9, the QRS is wide due to a right bundle branch block. This finding increases the likelihood (but does not prove) that the block here is infranodal. This important pattern is easily missed because the nonconducted P waves (arrows) fall near the T wave of the preceding beats and therefore may be overlooked.
Cautions: 2:1 AV block may present a very common pitfall in ECG analysis when the nonconducted P wave is hidden in the preceding T wave (see Chapter 23). The rhythm may be misdiagnosed as “normal sinus” or “sinus bradycardia.” If the PR interval of conducted beats is not prolonged (as usually seen in infranodal block) the presence of AV block can be completely missed while the patient, in fact, urgently needs a permanent pacemaker.
Blocked atrial bigeminy (see Chapter 14) can appear similar to 2:1 AV block, but PP interval differences usually allow you to distinguish between these two distinct diagnoses. In 2:1 AV block, the P waves come “on time,” but with atrial bigeminy and blocked APBs, every other P′ wave is early.
Atrial Fibrillation or Flutter with AV Heart Block
Important Clinical Considerations
Symptoms
Symptoms of heart block vary depending on its degree as well as the time course of its development.
PR interval prolongation (first-degree AV block) is usually asymptomatic (see Box 17-4). Occasionally, if the PR interval becomes so long that the P waves move close to the preceding QRS complexes, the patient might feel pulsation in the neck and dizziness, similar to that seen in the pacemaker syndrome, due to near simultaneous atrial and ventricular contractions (see Chapter 21).
BOX 17-4 Infections and Heart Block
• Progressive PR prolongation in a patient with infective endocarditis is an ominous sign, suggesting the development of a peri-valvular abscess.
• Lyme disease can produce any degree of heart block at the level of AV node, including complete heart block, often associated with severe symptoms. Occasionally syncope can be the first presentation of the disease. Almost always the block resolves with antibiotic therapy, but sometimes temporary pacing is required.
Development of a complete heart block can be a life-threatening event presenting with presyncope or syncope (Adams-Stokes attacks) due to a very slow escape rate or even to prolonged asystole. This severe bradycardia is more likely to happen with infranodal complete blocks due to their more abrupt onset and the slower rate of the escape rhythms (see Chapter 13).
In addition, very slow rates can induce severe QT interval prolongation and torsades de pointes ventricular tachycardia (see Chapter 16), culminating in cardiac arrest due to ventricular fibrillation (see Chapter 19). If the patient survives this initial episode of complete heart block, the primary complaints are usually severe exertional dyspnea and fatigue due to inability to augment heart rate and cardiac output with exercise, similar to that of second-degree AV block.∗
Treatment Considerations
The initial, emergency approach to a symptomatic patient with complete heart block should follow the current ACLS algorithms and appropriate measures, including preparation for transcutaneous pacing if indicated. If the patient is hemodynamically stable, the level of block should be determined and potential causes reviewed (see Boxes 17-2 and 17-3).
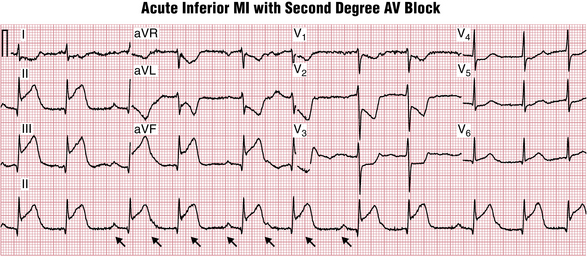
AV Heart Block in Acute Myocardial Infarction
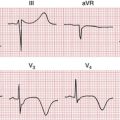
The AV node is usually supplied from the right coronary artery (and less frequently from the circumflex coronary artery). Occlusion of these vessels produces inferior myocardial infarction and block at the level of AV node (Fig. 17-11). This block is usually transient and almost always resolves with time so that a permanent pacemaker is rarely needed, although temporary pacing might be necessary.
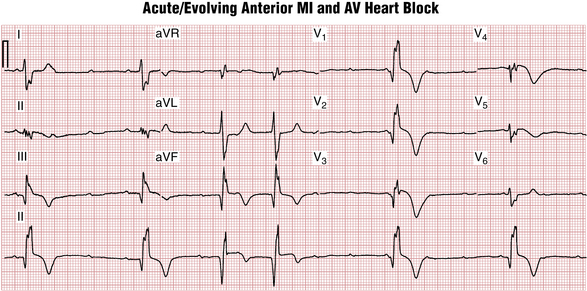
In contrast, the His bundle, proximal portions of the right bundle branch, and left anterior fascicle of the left bundle branch are supplied by the septal branches of the left anterior descending (LAD) artery. Very proximal LAD artery occlusion producing anterior infarction may also cause infranodal heart block, often preceded by right bundle branch block (RBBB) or bifascicular blocks. This condition can progress abruptly to a complete heart block and often requires prophylactic pacemaker implantation (Fig. 17-12).
AV Dissociation Syndromes
• AV dissociation is widely used as a general term for any arrhythmia in which the atria and ventricles are controlled by independent pacemakers. The definition includes complete heart block, as described previously, as well as some instances of ventricular tachycardia or accelerated idioventricular rhythm in which the atria remain in sinus rhythm (see Chapter 16).
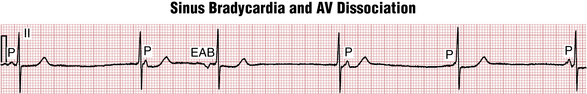
• AV dissociation is also used as a more specific term to describe a particular family of arrhythmias that are often mistaken for complete heart block. With this type of AV dissociation, the SA node and AV junction appear to be “out of synch”; thus, the SA node loses its normal control of the ventricular rate. As a result the atria and ventricles are paced independently—the atria from the SA node, the ventricles from the AV junction. This situation is similar to what occurs with complete heart block. However, in this instance, the ventricular rate is the same as or slightly faster than the atrial rate. When the atrial and ventricular rates are almost the same, the term isorhythmic AV dissociation is used. (Iso is the Greek root for “same.”)
AV dissociation (Fig. 17.13) when used in this more specific context, therefore, can be regarded as a “competition” between the SA node and the AV node for control of the heartbeat. It may occur either when the SA node slows down (e.g., because of the effects of beta blockers or calcium channel blockers or with increased vagal tone) or when the AV node is accelerated (e.g., by ischemia or digitalis toxicity). Not uncommonly, isorhythmic AV dissociation is seen in healthy young individuals, particularly when they are sleeping.
Figure 17-14 presents an example of isorhythmic AV dissociation, a common benign arrhythmia easily confused with complete heart block. Notice the P waves with a variable PR interval because the ventricular (QRS) rate is nearly the same as the atrial rate. At times the P waves may merge with the QRS complexes and become imperceptible for several beats. If the sinus rate speeds up sufficiently (or the AV junctional rate slows), the atrial stimulus may be able to penetrate the AV junction, reestablishing sinus rhythm.
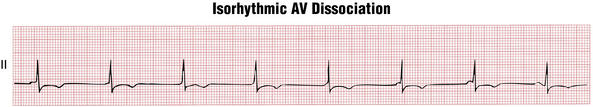
Figure 17-14 This common type of atrioventricular (AV) dissociation is characterized by transient desynchronization of the sinus and AV node pacemakers, such that they beat at nearly the same rate. Because they are “out of synch” with each other, the P waves (representing the sinus node pacemaker) appear to “slide” in and out of the QRS (representing the AV node “escape” pacemaker). This type of AV dissociation, a minor arrhythmia, must be distinguished from actual complete AV block, a life-threatening conduction problem (compare with Figs. 17-7 and 17-8).
∗ In some cases, however, the PR interval may not prolong noticeably, or it may even shorten. This atypical pattern is most common with very long cycles and long PR intervals. However, even in such atypical cases, the PR interval following the nonconducted beat will always be shorter than the PR interval before it.
∗ In uncertain cases, in which the need for a pacemaker is being assessed, an invasive electrophysiologic study can be done to record directly the signals from the conduction system of the heart. In Mobitz I block the signal blocks in the AV node without reaching the His bundle area. In Mobitz II block the signal reaches the His bundle, producing a typical deflection on the intracardiac recording.
∗ Rarely, patients may have congenital complete heart block (which is usually at the AV nodal level, associated with a narrow and not excessively slow QRS escape mechanism). These individuals may be asymptomatic (other than noting a slow pulse) because of adaptation including increased left ventricular dimension and stroke volume.