22 Atrial septal defect
Salient features
History
Ostium secundum defect (anatomically in the region of the fossa ovalis)
• Asymptomatic particularly small defects with minimal left to right shunting; moderate or large defects often have no symptoms until third or fourth decades despite substantial left-to-right shunting (characterized by a ratio of pulmonary to systemic flow of 1.5 or more)
• Palpitations indicating atrial arrhythmias
• Productive cough indicating recurrent pulmonary infections
Examination
• Diffuse or normal apical impulse
• Ejection systolic flow murmur in the left second and third intercostal space
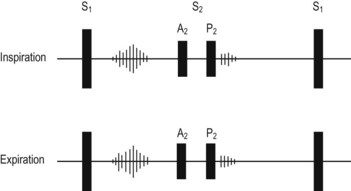
• Wide, fixed, split second heart sound (occasionally a slight movement of P occurs) that does not vary with respiration (Fig. 22.1)
• Infrequently, a mid-diastolic murmur may be heard in the tricuspid area (indicating a large left-to-right shunt)
Advanced-level questions
What are the types of atrial septal defect
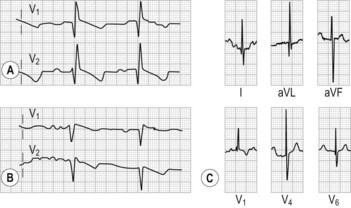
• Ostium secundum defect accounts for 70% of the cases. The defect is in the middle portion of the atrial septum and is usually 2–4 cm in diameter (incomplete right bundle branch block pattern, QRS axis rightward) (Fig. 22.2A,B).
• Sinus venosus type is a defect in the septum just below the entrance of the superior vena cava into the right atrium (leftward P wave axis so that P waves are inverted in at least one inferior lead) (Fig. 22.2C).
• Ostium primum type is a defect in the lower part of the septum and clefts may occur in the mitral and tricuspid valves (QRS axis leftward). A junctional or low atrial rhythm (inverted P waves in the inferior leads) occurs with sinus venosus defects.
In which conditions is an abnormally widely split second sound present?
• ASD, ventricular septal defect (VSD), pulmonary regurgitation (caused by increased right ventricular volume)
• Pulmonary stenosis (caused by increased right ventricular pressure)
• Right bundle branch block (caused by right ventricular conduction delay)
• Mitral regurgitation, VSD (caused by premature left ventricular emptying).
What is Lutembacher syndrome?
ASD with an acquired rheumatic mitral stenosis (Arch Mal Coeur 1916;9:237).
How would you investigate a patient with atrial septal defect?
• Cardiac catheterization is often unnecessary in diagnosis but is useful in determining the magnitude and direction of shunting and to determine the severity and reversibility of pulmonary hypertension
What are the complications of atrial septal defect?
• Atrial arrhythmias: atrial fibrillation is most common. Atrial fibrillation is often accompanied by the appearance of tricuspid regurgitation. Patients are usually in normal sinus rhythm in the first three decades of life, after which atrial arrhythmias including atrial fibrillation and supraventricular tachycardia may appear
• Pulmonary hypertension with the development of right ventricular disease
• Eisenmenger syndrome with reversal of shunt
• Infective endocarditis in patients with ostium primum defects only
How would you manage an uncomplicated atrial septal defect?
• When detected in early childhood, surgical closure is recommended between the age of 5 and 10 years to prevent the late onset of either right ventricular failure, atrial arrhythmias or right heart failure.
• In adults, small ASDs can be left alone, although many believe all ASDs must be closed. Those operated on before the age of 25 years have an excellent prognosis and one may anticipate normal long-term survival, but older patients require regular supervision. In a recent study, surgical repair of atrial septal defects in middle-aged and elderly patients was found to improve longevity and reduce functional limitation caused by heart failure and was, therefore, superior to medical treatment. However, the risk of atrial arrhythmias, especially fibrillation and flutter, and the attendant risk of thromboembolic events were not reduced by closure of the defect.
• Left-to-right shunt saturations of 1.5:1 or more require surgical closure to prevent right ventricular dysfunction.
• Other indications for surgery include evidence of pulmonary vascular reactivity when challenged with pulmonary vasodilators or a lung biopsy with pulmonary arterial changes being potentially reversible.
• A history of a cryptogenic cerebrovascular event in the presence of a small ASD with right-to-left shunting is also recommended for closure.
• Closure in adults results in a reduction in right ventricular size and improves symptoms.
What do you know about ostium primum defects?
They are associated with endocardial cushion defects often resulting in cleft mitral valve (usually anterior leaflet) causing mitral regurgitation. The ECG shows right bundle branch block and left axis deviation (Fig. 22.2C). Treatment is surgical closure with repair of cleft mitral valve, which generally involves simple interrupted suture repair of the cleft or the addition of a mitral annuloplasty for annular reduction and stabilization.