Chapter 9 Atlantooccipital and Atlantoaxial Joint Block for Cervicogenic Headache
Cervicogenic headache
Cervicogenic headache is defined a unilateral headache defined by the following characteristics:
Diagnostic Criteria for Cervicogenic Headache
Tables 9.1and 9.2 summarize the various levels of criteria and the minimum requirements for the diagnosis of cervicogenic headache.
Table 9.1 Sensitivity and Specificity of Diagnostic Criteria in Patients Fulfilling the Criteria for Cervicogenic Headache
| Diagnostic Criteria | Specificity | Sensitivity |
|---|---|---|
| Major Symptoms and Signs | ||
| Unilateral headache | 0 | 1.00 |
| Pain triggered by neck movements and/or sustained awkward head positioning | 0.75 | 0.44 |
| Pain elicited by external pressure over the greater occipital nerve (GON) or the ipsilateral upper, posterior neck region C2-C3 | 1 | 0.17 |
| Ipsilateral neck, shoulder and arm pain of a rather vague, nonradicular nature | 0.88 | 0.65 |
| Reduced range of motion in the cervical spine | 0.38 | 0.91 |
| Pain Characteristics | ||
| Pain episodes of varying duration or fluctuating continuous pain | 0.88 | 0.78 |
| Moderate, nonexcruciating pain, usually of a nonthrobbing nature | 0.86 | 0.91 |
| Pain starting in the neck, eventually spreading to the oculofrontotemporal area | 0 | 1.00 |
| Other Important Criteria | ||
| Anesthetic blockades of the GON or C2 root | 1.0 | 0.18 |
| Patient has sustained neck trauma a relatively short time prior to the onset | 0.88 | 0.65 |
| Minor, More Rarely Occurring, Nonobligatory Symptoms and Signs | ||
| Rarely occurring nausea, vomiting, and photophobia and phonophobia | 0.88 | 0.48 |
| Ipsilateral edema and, less frequently, flushing, mostly in the periocular area | 0.88 | 0.09 |
| Dizziness | 0.75 | 0.26 |
| “Blurred vision” in the eye ipsilateral to the pain | 1.00 | 0.22 |
| Difficulty on swallowing | 0.88 | 0.09 |
Table 9.2 Summary of Minimum Requirements for Diagnosis of Cervicogenic Headache
| Definitive for cervicogenic headache (CGH) | Precipitating factors as described by patient and observed by physician Positive result of anesthetic blockade Unilateral pain without side shift |
| Combination of factors provisional/tentative for CGH | Reduced range of neck motion; ipsilateral shoulder/arm pain Positive result of anesthetic blockade Unilateral pain without side shift |
The major criteria of cervicogenic headache are as follows:
Characteristics of headache may be described as follows:
Other important characteristics are as follows:
Other features of lesser importance.
The following attack-related phenomena are rare and moderate when present:
Clinical Characteristics of Cervicogenic Headache
Cervicogenic headache has the following clinical characteristics:
Atlantooccipital and atlantoaxial joint pain
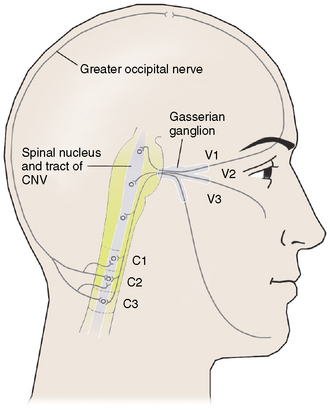
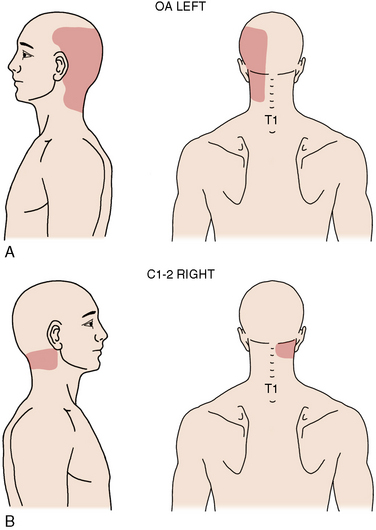
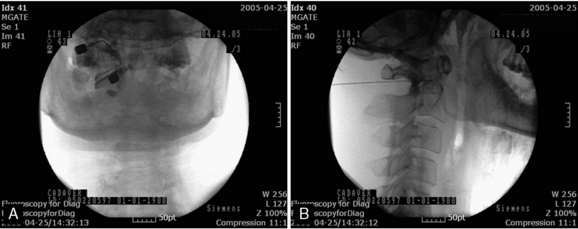
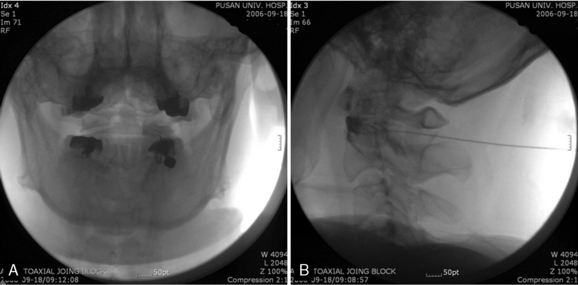
Atlantooccipital (AO) and atlantoaxial (AA) joint pain is defined as pain arising from the atlantooccipital and atlantoaxial joints. Patients typically present with occipital headaches, which are often associated with suboccipital pain and aggravated by lateral rotation, flexion, and/or extension of the cervical spine (Figs. 9-1 and 9-2) [1].
Common causes of pain in the AO and AA joints caused by inflammation and adhesion are as follows:
Box 9.1 summarizes the clinical presentation of AO and AA joint pain.
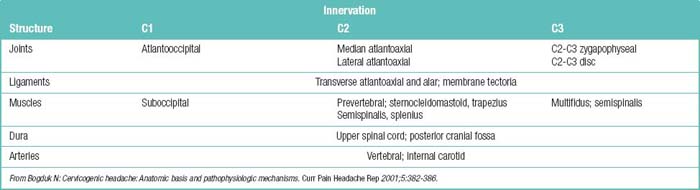
The mechanisms of AO and AA join pain are summarized in Table 9.4.
Table 9.4 Mechanisms of Atlantooccipital and Atlantoaxial Joint Pain
| Atlantooccipital joint pain |
Table 9.5 lists the disorders in the differential diagnosis of AO and AA joint pain.
Table 9.5 Differential Diagnosis of Atlantooccipital and Atlantoaxial Joint Pain
| Vascular | Vertebral artery aneurysm Temporal arteritis Basilar artery spasm (migraine) |
| Central nervous system | Inflammation of dura by blood or infection C1-C3 nerve root irritation Arnold-Chiari malformation |
| Intracranial | Tumor Arteriovenous malformation Hemorrhage |
| Musculoskeletal | Discopathy of upper cervical spine, e.g., C2-C3 degenerative disc disease and C2-C3 herniation Atlantooccipital and atlantoaxial inflammatory arthropathy (facet) Tender muscle ligaments C2-C3 facet arthropathy |
Related anatomy and physiology
The Atlantooccipital Joint
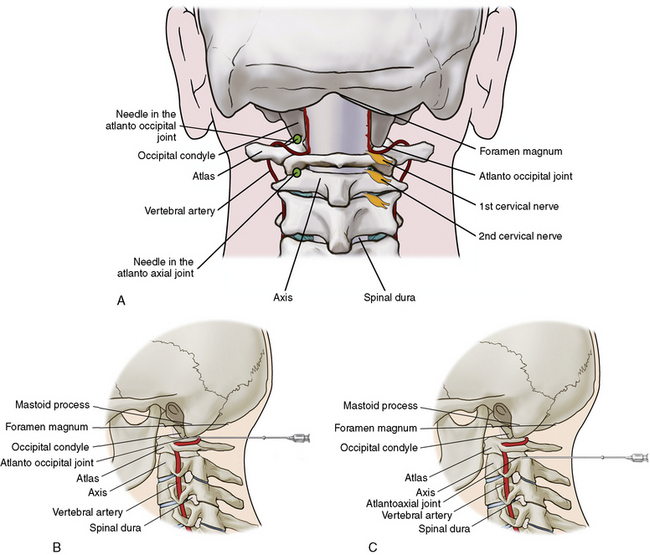
The vertebral artery runs medially and diagonally (to enter the skull’s foramen magnum) and is often located overlying the medial third of the joint. Other surrounding structures are the carotid artery and jugular veins anterolaterally (Fig. 9-3). The AO joint permits flexion of about 10 degrees and extension of about 25 degrees in passive range of motion (ROM) [2].
The Atlantoaxial Joint
The vertebral artery runs on the lateral third of the joint dorsally and then goes through the C1 vertebra (atlas) superiorly to pass into the foramen magnum medially. The AA joint permits lateral rotation of about 70 degrees on either side around the odontoid process. The AA joint also allows isolated flexion and extension of 5 degrees and 10 degrees, respectively, in and of itself [2].
Atlantooccipital and atlantoaxial joint block
Complications
The complications of AO and AA joint block are as follows:
Preoperative Preparation
The preoperative preparation required prior to AA or AO joint blocks involve the same examination and imaging as those before other neural blockade procedures. Please see Chapters 6 and 8 for discussion of the preoperative preparation required.
Procedure
Figures 9-4 and 9-5 illustrate examples of AO and AA joint block.