Chapter 402 Atelectasis
Pathophysiology
The causes of atelectasis can be divided into five groups (Table 402-1). Respiratory syncytial virus (RSV) and other viral infections in young children can cause multiple areas of atelectasis. Mucous plugs are a common predisposing factor to atelectasis. Massive collapse of one or both lungs is most often a postoperative complication but occasionally results from other causes, such as trauma, asthma, pneumonia, tension pneumothorax (Chapter 405), aspiration of foreign material (Chapters 379 and 389), and paralysis, or after extubation. Massive atelectasis is usually produced by a combination of factors, including immobilization or decreased use of the diaphragm and the respiratory muscles, obstruction of the bronchial tree, and abolition of the cough reflex.
| CAUSE | CLINICAL EXAMPLES |
|---|---|
| External compression on the pulmonary parenchyma | Pleural effusion, pneumothorax, intrathoracic tumors, diaphragmatic hernia |
| Endobronchial obstruction completely obstructing the ingress of air | Enlarged lymph node, tumor, cardiac enlargement, foreign body, mucoid plug, broncholithiasis |
| Intraluminal obstruction of a bronchus | Foreign body, granulomatous tissue, tumor, secretions, including mucous plugs, bronchiectasis, pulmonary abscess, asthma, chronic bronchitis, acute laryngotracheobronchitis |
| Intrabronchiolar obstruction | Bronchiolitis, interstitial pneumonitis, asthma |
| Respiratory compromise or paralysis | Neuromuscular abnormalities, osseous deformities, overly restrictive casts and surgical dressings, defective movement of the diaphragm, or restriction of respiratory effort |
Diagnosis
In foreign body aspiration, atelectasis is one of the most common radiographic findings. The site of atelectasis usually indicates the site of the foreign body (Chapter 369.1). Atelectasis is more common when diagnosis of foreign body aspiration is >2 wk.
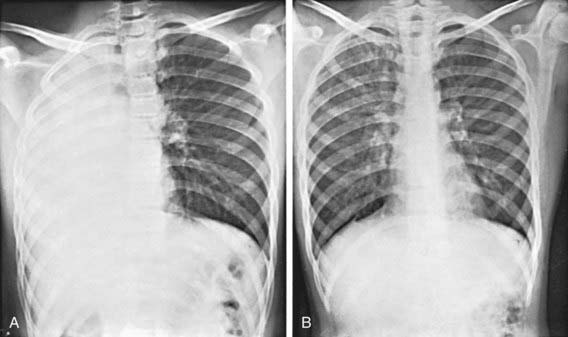
Massive pulmonary atelectasis is generally diagnosed on chest radiograph. Typical findings include elevation of the diaphragm, narrowing of the intercostal spaces, and displacement of the mediastinal structures and heart toward the affected side (Fig. 402-1).
Treatment
Lobar atelectasis in cystic fibrosis is discussed in Chapter 395.
Airway clearance therapies utilized for adults are often recommended and/or utilized in pediatric populations. However, given the differences in respiratory physiology and anatomy between children and adults, practices applicable to one may or may not apply to the other. Atelectasis due to cystic fibrosis is the only pediatric entity that clearly benefits from airway clearance therapy, although that due to neuromuscular disease, cerebral palsy, or mechanical ventilation probably benefits from such therapy (Table 402-2). Thus far no specific airway clearance therapy has been demonstrated to be superior.
Table 402-2 BENEFIT OF AIRWAY CLEARANCE THERAPIES IN PEDIATRIC CONDITIONS
CLEAR AND PROVEN BENEFIT
Cystic fibrosis
PROBABLE BENEFIT
POSSIBLE BENEFIT
Prevention of post-extubation atelectasis in neonates
MINIMAL TO NO BENEFIT
From Schechter MS: Airway clearance applications in infants and children, Resp Care 52:1382–1390, 2007.
Ashizawa K, Hayashi K, Aso N, et al. Lobar atelectasis: diagnostic pitfalls on chest radiography. Br J Radiol. 2001;74:89-97.
Birnkrant DJ. The assessment and management of the respiratory complications of pediatric neuromuscular diseases. Clin Pediatr. 2002;41:301-308.
Engoren M. Lack of association between atelectasis and fever. Chest. 1995;107:81-84.
Girardi G, Contador AM, Castro-Rodriguez JA. Two new radiological findings to improve the diagnosis of bronchial foreign-body aspiration in children. Pediatr Pulmonol. 2004;38:261-264.
Hendriks T, de Hoog M, Lequin MH, et al. DNase and atelectasis in non-cystic fibrosis pediatric patients. Critical Care. 2005;9:R351-R356.
Miske LJ, Hickey EM, Kolb SM, et al. Use of the mechanical In-Exsufflator in pediatric patients with neuromuscular disease and impaired cough. Chest. 2004;125:1406-1412.
Scolieri P, Adappa ND, Coticchia JM. Value of rigid bronchoscopy in the management of critically ill children with acute lung collapse. Pediatr Emerg Care. 2004;20:384-386.
Thomas K, Habibi P, Britto J, et al. Distribution and pathophysiology of acute lobar collapse in the pediatric intensive care unit. Crit Care Med. 1999;27:1594-1597.
Tokar B, Ozkan R, Ilhan H. Tracheobronchial foreign bodies in children: importance of accurate history and plain chest radiography in delayed presentation. Clin Radiol. 2004;59:609-615.
Tsai SL, Crain EF, Silver EJ, et al. What can we learn from chest radiographs in hypoxemic asthmatics? Pediatr Radiol. 2002;32:498-504.
Yen Ha TK, Bui TD, Tran AT, et al. Atelectatic children treated with intrapulmonary percussive ventilation via a face mask: clinical trial and literature overview. Pediatr Int. 2007;49:502-507.