Assessment and Management of the Newborn
I Clinical Evaluation of the Newborn (Table 26-1)
TABLE 26-1
Normal Vital Signs of the Newborn
| Range | Term | Preterm | |
| Respiratory rate, breaths/min | 30 to 60 | Close to 30 | Close to 60 |
| Heart rate, beats/min | 110 to 160 | Close to 110 | Close to 160 |
| Blood pressure, mm Hg | 50/35 to 65/40 | 65/40 | 50/35 |
| Temperature, °C | 36.5 to 37 | 36.5 to 37 | 36.5 to 37 |
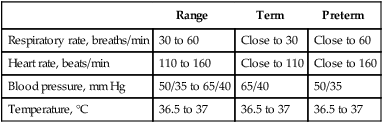
1. Normal rate: 30 to 60 breaths/min
2. Determined when newborn is not crying.
3. Fluctuation of the respiratory rate is normal.
4. Respirations are not necessarily regular.
5. Preterm infants display more erratic respiratory patterns than term infants.
1. Defined as respiration interrupted by short periods of apnea.
2. Apnea can last as long as 10 seconds.
3. Not associated with other abnormalities such as cyanosis or bradycardia.
4. Periodic breathing is common in preterm infants.
5. Usually does not require treatment, but close monitoring is important.
6. Little chest wall movement is observed.
7. An accurate respiratory rate must be counted for 1 full minute.
1. Often seen in premature newborns weighing <1500 g, with respiratory rates <30 breaths/min.
2. May be accompanied by bradycardia, cyanosis, or both.
3. Newborns may respond to gentle shaking or rubbing, or respirations may return spontaneously.
4. Primary apnea may occur immediately after birth; usually associated with bradycardia.
5. Newborns with primary apnea will resume breathing with stimulation.
6. Newborns with secondary apnea do not resume breathing on their own.
7. Heart rate, blood pressure, and Pao2 level decrease during apnea.
1. Heart rate in the newborn is generally determined by auscultation.
2. It can also be determined by tightly compressing the umbilicus with the index finger and thumb proximal to the abdomen.
3. Heart rate is usually higher in preterm infants than in term infants.
4. Normal heart rate fluctuates between 110 and 160 beats/min.
5. Bradycardia is usually secondary to significant apnea.
6. Palpation of the apical pulse is an important indicator of cardiac status.
7. Palpation of the apical pulse is used to locate the position of the heart.
8. Normally felt at the fifth intercostal space in the midclavicular line.
9. Peripheral pulses are found by palpating the brachial, radial, and femoral arteries.
1. Usually measured with a Doppler apparatus and a blood pressure cuff.
2. Blood pressure cuff must be of appropriate size for an infant to obtain an accurate pressure.
3. A cuff ≤1-inch width is used, although larger infants may require a larger cuff.
4. Blood pressure is usually obtained from the leg with the cuff around the thigh, although it may be obtained from the arm.
5. Low birth weight infants’ blood pressure averages 50/35 mm Hg.
6. Infants with birth weights >2000 g have an average blood pressure of 60/35 mm Hg.
7. Infants with birth weights >3000 g have an average blood pressure of 65/40 mm Hg.
8. Peripheral pulses are an important and a quick indicator of blood pressure.
9. Weak peripheral pulses commonly indicate a hypotensive state.
1. An infant’s temperature is usually taken in the axilla or obtained via a probe placed on the infant’s skin.
2. Infant temperature is a vital component in maintaining acid-base status.
3. Maintaining thermoregulation is critical to transition after birth, more so in preterm infants than in term infants.
4. Infant temperatures usually are maintained at 36.5° C to minimize oxygen consumption and prevent acidosis.
II Signs of Respiratory Distress
1. In the newborn defined as a respiratory rate >60 breaths/min.
2. Normal fluctuations in respiratory rate in the newborn can make initial assessment difficult.
3. Close observation and accurate count of respiratory rate for a full minute are needed to quantify the need for further intervention.
1. Cyanosis, or bluish discoloration, may be localized or generalized.
2. Generalized cyanosis usually indicates a more serious problem.
3. A well-lighted environment is essential for evaluation of cyanosis.
4. Central cyanosis, involving the mucous membranes, indicates presence of excessive amounts of desaturated hemoglobin.
5. Peripheral cyanosis (acrocyanosis) of the hands and feet is common in newborns and usually dissipates several hours after birth.
6. Central cyanosis usually indicates an arterial oxygen tension of <40 mm Hg.
7. Oxygen therapy usually required but may be contraindicated if a cardiac diagnosis is made.
8. Cyanosis is more difficult to assess in nonwhite infants.
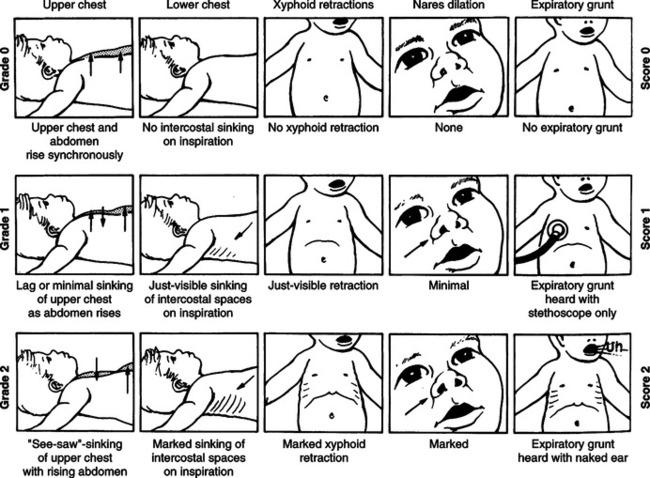
1. Involves flaring of the nostrils (alae nasi) during inspiration.
2. Believed to be a sign of air hunger.
3. The greater the negative intrathoracic pressure that must be generated to move air, the greater the degree of flaring.
1. Is common in the infant with hyaline membrane disease.
2. May also be seen with other disorders.
3. Is presumed to be an attempt by the neonate to maintain positive pressure on expiration and prevent alveolar collapse.
4. Grunting results from exhalation against a partially closed glottis.
5. Is an obvious sound and usually heard without the aid of a stethoscope.
1. Retractions involve inward movement of the chest wall.
2. May occur between the ribs (intercostal), above the clavicles (supraclavicular), or below the rib margins (subcostal).
3. Retractions may also occur at the top (suprasternal) or the bottom (xiphoid) margins of the sternum.
4. Retractions may occur in any age group but are more common in the newborn because of the high compliance of the chest wall.
5. Retractions become more obvious and widespread as respiratory distress worsens.
6. As the infant forcefully contracts the diaphragm in an attempt to move air, the abdomen protrudes.
7. This increased negative pressure results in the entire anterior chest wall and sternum moving inward, producing a characteristic “seesaw” or paradoxical respiratory pattern.
TABLE 26-2
| Score | |||
| Sign | 0 | 1 | 2 |
| Heart rate (beats/min) | Absent | <100 | >100 |
| Respiratory effort | Absent | Weak, irregular | Good, crying |
| Muscle tone | Flaccid | Some flexion of extremities | Well flexed |
| Reflex irritability | No response | Grimace | Cough or sneeze |
| Color | Blue, pale | Body pink, extremities blue | Completely pink |
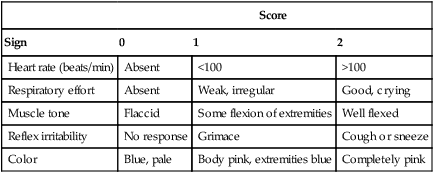
A Evaluation of the newborn begins as soon as the infant is delivered at 1- and 5-minute intervals.
B Standard care procedures are performed, including bulb suction of the upper airway, drying and warming of the infant, and cutting and clamping of the cord.
C A preliminary assessment is done during this time.
D The evaluation uses five factors.
E The infant is given a score of 0, 1, or 2 in all categories.
F The 1-minute score is especially useful to identify the infant who needs immediate intervention.
1. An Apgar score of ≤2 indicates a severely depressed infant who requires immediate resuscitation.
2. Ventilatory assistance will be necessary.
3. If the score is between 3 and 6 the infant may need some assistance, usually more vigorous stimulation and oxygen.
4. Infants with scores of ≥7 are considered stable and require only routine care and close observation.
5. The 5-minute score is useful to assess recovery from depression and the effectiveness of any previous interventions.
6. If the infant remains depressed at 5 minutes, with a score of ≤6, concern regarding cardiopulmonary status should be exercised, and the infant should be placed under special care.
7. These infants are at high risk for further postpartum complications:
8. An Apgar score at 5 minutes of ≤7 will require another Apgar assessment at 10 minutes.
A The appropriate size mask and anesthesia (flow-inflating) bag should be used.
B The jaw is moved upward and away from the neck by placing a towel under the shoulders (if time allows).
C Ensure proper seal with mask over the infant’s nose and mouth.
D An airtight seal between the rim of the mask and the face is essential to achieve effective positive-pressure ventilation of the lungs.
E An orogastric tube may be needed to aspirate air from the stomach.
F Effective ventilation is present when:
1. Breath sounds are heard bilaterally.
2. Heart rate increases to >100 beats/min.
G If no improvement after 30 seconds:
H If inadequate response to these maneuvers, prepare to intubate.
A Intubation should be performed when:
B Estimation of endotracheal tube (ETT) sizes
1. Weight and tube size indicated.
2. Neonatal airways do not contain cuffs.
3. Proper placement of ETTs can be assessed by:
4. ETTs should be securely taped after intubation.
5. Appropriate ventilation, FIO2, and humidification should be provided.
B After obtaining equipment, suction the upper airway.
C Preoxygenate with resuscitation bag to maintain an oxygen saturation of 100%.
D Position infant properly with towel if necessary under the shoulders.
E It is important to properly align infant so that the pharynx and trachea are in the midline position.
F Insert appropriately sized blade, and visualize vocal cords.
G Insert appropriately sized ETT through vocal cords into trachea.
H After placement ventilate with pressures of 20 to 25 cm H2O.
I Evaluate position of tube by visualizing chest wall movement and auscultating with a stethoscope.
J Note centimeter mark at upper lip, and secure tube with proper tape.
K Obtain a chest radiograph to confirm correct ETT position.
L If intubation is unsuccessful after 30 seconds and heart rate decreases to <100 beats/min, reestablish oxygenation with bag/mask ventilation.
A Perform suctioning as needed according to breath sounds, O2 saturation, and clinical presentation of infant.
B Use the appropriate size catheter.
C Preoxygenate infant with 100% oxygen if situation allows.
D Saline may be instilled into the ETT before suctioning to help thin secretions, but this should not be routine for suctioning.
E Suction pressure should not exceed 100 mm Hg.
F Remove thick secretions by repeated saline instillations.
G Monitor heart rate closely while suctioning, and observe for any vagal or bradycardic effects of procedure.
H Newer in-line suction catheters used to minimize carinal irritation and prevent vagal responses.
I Catheters are measured and the centimeter mark noted so that exact catheter placement is achieved each time the infant is suctioned.
J Apply suction only during withdrawal of catheter and for no longer than 10 seconds.
VIII Cardiopulmonary Resuscitation (Modified from the American Heart Association: Neonatal Resuscitation Guidelines, 2000)
A Initiate chest compressions when:
1. The heart rate remains <60 beats/min despite 30 seconds of effective positive-pressure ventilation.
B Two techniques are used for cardiac compression on any newborn.
1. The first technique involves placing the thumbs of both hands over the lower one third of the infant’s sternum while the other fingers are wrapped around the back to provide stability and support.
2. The two-finger technique uses the index and middle fingers to compress the lower one third of the sternum while the other hand is used to support the back.
3. The thumb technique is usually preferred.
4. To ensure proper rate of chest compressions and ventilation, the compressor repeats “one and two and three and breathe and….”
5. During chest compressions, the breathing rate is 30 breaths/min, and the compression rate is 90 compressions/min.
6. This equals 120 “events” per minute; one cycle of three compressions and one breath takes 2 seconds.
C During chest compressions ensure that:
1. Chest movement is adequate during ventilation.
3. Compression depth is one third the diameter of the chest.
4. Thumbs or fingers remain in contact with the chest at all times.
5. Duration of the downward stroke of the compression is shorter than the duration of the release.
D After 30 seconds of chest compressions and ventilation, check the heart rate. If the heart rate is:
1. Greater than 60 beats/min, discontinue compressions and continue ventilation at 40 to 60 breaths/min.
2. Greater than 100 beats/min, discontinue compressions, and gradually discontinue ventilation if the newborn is breathing spontaneously.
3. Less than 60 beats/min, intubate the newborn, if not already done. This provides a more reliable method of continuing ventilation and a route for epinephrine administration.
E Medications used during cardiopulmonary resuscitation (CPR) (Table 26-3)
TABLE 26-3
| Drug | Indication | Dose | Route of Administration |
| Epinephrine | Low heart rate (<60 beats/min) or no heart rate | 0.1 to 0.3 ml/kg of a 1:10,000 solution in 1 ml | Endotracheal tube or intravenous |
| Naloxone hydrochloride (Narcan) | Acute maternal narcotic depression | 0.1 ml/kg of a 1.0 mg/ml solution in a 1 ml volume | Endotracheal tube or intravenous |
| Saline as volume expander | Evidence of blood or fluid loss | 10 ml/kg given slowly over 5-10 min | Intravenous |
| Sodium bicarbonate (NaHCO3) | Metabolic acidosis | 2 mEq/kg of a 4.2% solution | Intravenous |
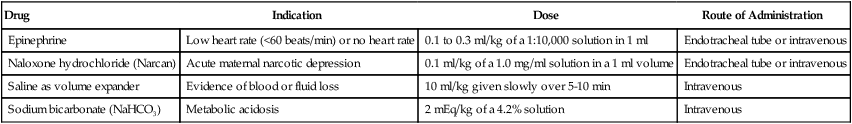
1. Best treatment for brief periods of bradycardia: Ventilation and 100% oxygen.
2. Epinephrine: potent α- and β-receptor stimulation
a. Increases perfusion pressure, coronary blood flow, and oxygen delivery to the heart.
b. Indicated when the heart rate remains <60 beats/min, despite 30 seconds of assisted ventilation and another 30 seconds of coordinated chest compressions and ventilations.
c. Improves cardiac contractility and increases heart rate.
d. Given when the heart rate is 0 beats/min.
e. Dosage is 0.1 to 0.3 ml/kg of a 1:10,000 solution in 1-ml syringe.
f. Given rapidly via ETT or intravenously and can be repeated every 5 minutes until an acceptable heart rate is achieved.
3. Naloxone hydrochloride (Narcan)
a. Indicated for infants with severe respiratory depression after positive-pressure ventilation has restored a normal heart rate and color.
b. Mother with a history of narcotic administration within the past 4 hours.
c. Not indicated for an infant of a mother who is suspected of being addicted to narcotics or is on methadone therapy. If given, it may result in the newborn developing acute severe seizure activity.
d. Other drugs such as magnesium sulfate or nonnarcotic analgesics or general anesthetics will not respond to naloxone.
e. Dosage is 0.1 ml/kg of a 1.0-mg/ml solution in a 1-ml syringe.
f. May be administered via the ETT, but intravenous administration is preferred.
a. Administered for suspected or documented metabolic acidosis.
b. Not to be given unless the lungs are being adequately ventilated.
c. Sodium bicarbonate is caustic and should not be given through an ETT.
d. Recommended dosage: 2 mEq/kg (4 ml/kg of 4.2% solution)
e. Preferred route of administration is umbilical vein, from which there is a good blood return.
a. Indicated for an infant not responding to resuscitation.
b. Evidence of blood loss (e.g., pale color, weak pulses, persistently high or low heart rate, no improvement in circulatory status despite resuscitation efforts).
c. Normal saline volume expander of choice.
6. Drugs that can be given via an ETT are atropine, lidocaine, epinephrine, and naloxone (Narcan).
IX Other Newborn Assessment Scales
1. The Dubowitz scoring method determines gestational age when used within the first 5 days of birth.
2. It is accurate within 2 weeks of the newborn’s gestational age.
3. Each of the following categories is assessed on a graded scale. The higher the score assigned, the greater the gestational age of the newborn (Table 26-4).
TABLE 26-4
| Score | Gestation (wk) |
| 0-9 | 26 |
| 10-12 | 27 |
| 13-16 | 28 |
| 17-20 | 29 |
| 21-24 | 30 |
| 25-27 | 31 |
| 28-31 | 32 |
| 32-35 | 33 |
| 36-39 | 34 |
| 40-43 | 35 |
| 44-46 | 36 |
| 47-50 | 37 |
| 51-54 | 38 |
| 55-58 | 39 |
| 59-62 | 40 |
| 63-65 | 41 |
| 66-69 | 42 |
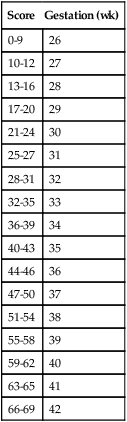
4. Assessment is done bilaterally.
a. External developmental signs (Table 26-5)
TABLE 26-5
External Developmental Signs of the Dubowitz Scoring System
| Signs | Score | Immature | Mature |
| Edema | 0-2 | None (0) | Pitting edema (2) |
| Skin texture | 0-4 | Transparent (0) | Leathery, cracked (4) |
| Skin color | 0-4 | Pale (0) | Dark red (3) |
| Skin opacity | 0-4 | Prominent skin veins (0) | No observable skin veins (4) |
| Lanugo | 0-4 | Large amounts of back hair (0) | None (4) |
| Plantar creases | 0-4 | No crease (0) | Deep crease (4) |
| Nipple formation | 0-3 | No areola (0) | Areola raised and stippled (3) |
| Breast size | 0-3 | No breast tissue (0) | >1 cm tissue (3) |
| Ear form | 0-3 | Pinna flat and shapeless (0) | Well-defined in-curving upper pinna (3) |
| Ear firmness | 0-3 | Soft, easily folded (0) | Firm with cartilage to edge (3) |
| Genitals male | 0-2 | Undescended or minimally descended testes (0) | Rugae or wrinkles in scrotal sac (3) |
| Genitals female | 0-2 | Widely separated labia majora with protruding labia minora (0) | Labia minora are covered by labia majora (2) |
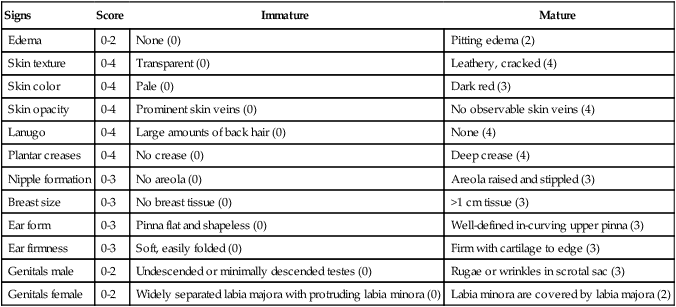
Number in parentheses indicates score.
From Dubowitz LMS, Dubowitz V, Goldberg C: Clinical assessment of gestational age in the newborn infant. J Pediatr 77:1-10, 1979.
(1) Edema: Finger pressure on the dorsum of the foot is done for a few seconds. Assessment compares no edema with pitting edema (score, 0 to 2).
(2) Skin texture: Skin is assessed to determine its texture. A transparent to leathery, cracked appearance is graded (score, 0 to 4).
(3) Skin color: Skin color is assessed during quiet time of the newborn. A pale to dark red appearance over the ears, lips, palms, and soles of the feet is used to determine scores (score, 0 to 3).
(4) Skin opacity: Skin of the abdominal trunk is assessed. More prominent skin veins are given a lower score, and no skin veins seen are given a higher score (score, 0 to 4).
(5) Lanugo: The amount of fine hair over the back of the newborn. Premature infants have large amounts of hair, whereas term and postterm infants have no hair. Score decreases with greater amounts of hair (score, 0 to 4).
(6) Plantar creases: Assessment is made on the soles of the feet. No creases are given a lower score, and deep creases are given a higher score (score, 0 to 4).
(7) Nipple formation: No nipple areola is given a low score, and areola raised and stippled is given a higher score (score, 0 to 3).
(8) Breast size: Assessment is done by palpating the nipple area and determining the approximate area of breast tissue. Measurements range from no breast tissue (low score) to >1 cm, which is given a higher score (score, 0 to 3).
(9) Ear form: Increase in scoring occurs as the form of the ear develops from the pinna being flat and shapeless to a well-defined, in-curving upper pinna (score, 0 to 3).
(10) Ear firmness: Scores increase as the ear develops from a soft, easily folded ear to a firm ear with cartilage to the edge (score, 0 to 3).
(a) Boys: Scores increase as the undescended testes develop into descended testes. Rugae, or wrinkles, in the scrotal sac are seen in the mature newborn.
(b) Girls (with hips half abducted): Scores increase as the widely separated labia majora with protruded labia minora develops to where the labia minora is covered by the labia majora (score, 0 to 2).
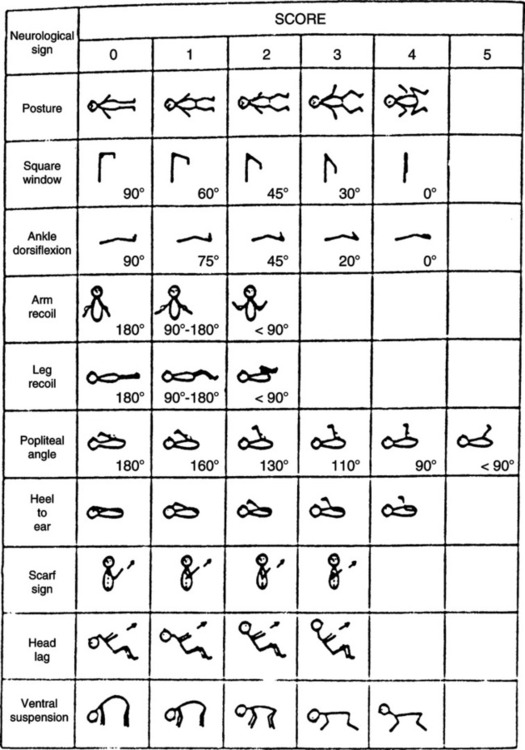
b. Neuromuscular/neurologic signs (Figure 26-1)
(1) Posture: Increased scores are assigned when greater flexion of the newborn is observed without touching.
(2) Square window: Scores are assessed by applying enough pressure to the hand to flex it to the forearm. Scores increase as the angle between the hypothenar eminence and forearm decreases from 90 to 0 degrees.
(3) Ankle dorsiflexion: The newborn’s foot is flexed against the anterior aspect of the leg. Scores increase as this angle decreases from 90 to 0 degrees.
c. Arm recoil: The newborn’s arms are flexed for a few seconds and then extended fully. Recoil is then observed by releasing the hands. Scores increase as the angle of the antecubital space reduces from 180 degrees to <90 degrees.
d. Leg recoil: This assessment is done the same way as the arm recoil. The score increases as the angle between the knees and the hips decreases from 180 degrees to <90 degrees.
e. Popliteal angle: The thigh is held in the high chest position. The leg is extended with the other hand. The score increases as the angle behind the knee decreases from 180 to <90 degrees.
f. Heel to ear: The newborn’s feet are drawn as close to the ears as possible. After releasing the feet, the score is then determined by assessing the popliteal angle and whether the feet can touch the ears.
g. Scarf sign: The newborn’s hand is extended to the opposite shoulder. Scores increase if the elbow of the extended hand does not go past the middle of the chest.
h. Head lag: The newborn is pulled upward by both arms from a supine position. Scores increase if the newborn is able to hold the head forward. The newborn’s head should be supported during this assessment.
i. Ventral suspension: The newborn, in a prone position, is suspended over one hand. The back, legs, arms, and neck are observed for extension. Scores increase as a curved back and neck with extended limp legs progress into a hyperextended back with good flexion of the arms and legs.
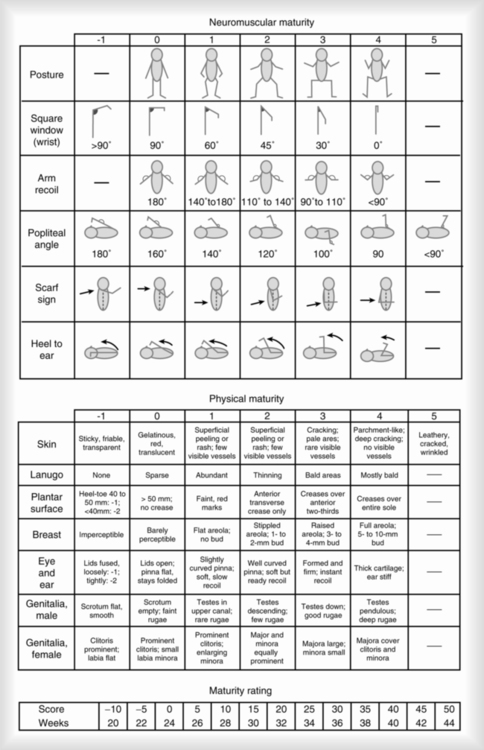
1. The Ballard score includes six neuromuscular/neurologic and six physical signs.
a. Neuromuscular signs: Posture, square window, arm recoil, popliteal angle, scarf sign, and heel to ear.
b. Physical signs: Skin, lanugo, plantar creases, breast, ears, and genitals.
c. It assesses the most useful items from the Dubowitz scoring system.
C Silverman scoring of acute respiratory distress of the neonate (Figure 26-3)
X Oxygen Administration Equipment
1. Most common form of short-term oxygen delivery to the newborn.
2. Oxyhoods are clear plastic boxes or cylinders that usually surround the infant’s head and have an opening for the infant’s neck.
3. For a specific FIO2 an oxyhood is preferred over other oxygen-delivery devices.
4. The device is also used to provide warm humidity.
5. It can be placed inside an isolette or on a warming table.
6. A minimum liter flow of 8 to 10 L/min is needed to adequately prevent rebreathing of exhaled carbon dioxide.
7. An FIO2 between 0.21 and 1.0 can be achieved with this device by delivering oxygen/air flow by an oxygen blender.
1. Becoming more popular for use with smaller infants.
2. Ideal for use in infants requiring long-term oxygen therapy.
3. Also used for infants who have been weaned and extubated from mechanical ventilation and do not tolerate nasal continuous positive airway pressure (CPAP).
4. Should be used with flowmeters calibrated in small increments, such as quarters or tenths of a liter per minute.
5. Flow rates used in infants and children with nasal cannulas range from 0.10 to 4.0 L/min.
6. Easy to deliver moderate FIO2 with this device.
8. Attention should be paid to oxygen saturation levels as monitored by pulse oximetry and flow titrated accordingly to achieve desired saturation.
1. Simple small, tight-fitting O2 masks can be used for short-term O2 therapy.
2. Difficult to apply to the infant’s face.
3. Poorly tolerated by an infant who becomes agitated with the device strapped to the head.
4. Often used to perform hyperoxia tests.
5. Must provide adequate flow (minimum, 6 L/min) to prevent retention of carbon dioxide.
D Flow-inflating resuscitation bags
1. A flow-inflating bag with mask attached is an excellent and effective way to deliver short-term, high FIO2 levels to an infant.
2. Often used in the operating room and delivery room to provide a quick and consistent oxygen source for the postoperative or newborn infant.
3. A flow of 8 to 10 L/min should be maintained for proper effect.
4. Can also be used as a mask CPAP device if infant develops respiratory distress and does not respond to conventional O2 therapy.
1. These devices are used for infants and children who require a cool environment and supplemental oxygen.
2. An FIO2 of 0.30 to 0.50 can be achieved.
3. Mist is provided by a baffle system that is powered by either air or oxygen at 12 to 15 L/min.
4. Difficult to maintain consistent FIO2 level because of large surface area and difficulty sealing plastic canopy around patient.
5. The tent surrounds the bed and is tucked in under the mattress to maintain temperature and FIO2.
6. Mist tents have fallen out of favor and use because of poor tolerance by patients and difficulty maintaining the unit by hospital staff.
XI Equipment for Thermal Control
1. Used to maintain proper temperature of the infant’s environment and to administer humidity.
2. No longer used as a vehicle for the delivery of oxygen therapy.
3. The temperature is monitored and maintained with a skin probe attached to the newborn (servocontrol).
4. Isolettes are now double walled and monitor the inner surface of the isolette and the patient’s skin. If either of these temperatures decreases below a preset value, the unit responds by increasing heat production.
5. Access to the newborn is provided by hand holes on the side of the hood or the hood can be lifted for complete exposure.
6. Humidification is provided by a system that blows air over standing water. Reduced relative humidity and infection are potential problems with this device.
1. Radiant warmers use an open-bed system that provides infrared heat from an overhead source.
2. The device allows procedures to be performed on the newborn and greater accessibility during treatment.
3. The wavelength of the infrared light does not harm the newborn’s eyes.
4. A probe attached to the skin determines the amount of infrared heat. The probe has a reflective patch to prevent inappropriate temperature adjustments.
5. Heat loss can occur from evaporation and convection (personnel passing by or drafts created by vents or opening or closing of doors).
6. Side shields can be placed around the bed to prevent convection and insensible water loss; plastic wrap has also been used to shield the infant and maintain proper temperature.
A Obtaining an arterial blood gas (ABG)
2. Radial artery site of choice
3. Normal ABG values (1 to 7 days) after birth
a. Placement of an indwelling catheter into a peripheral artery provides undisturbed access for frequent blood gas sampling.
b. Catheter also is used for continuous real-time blood pressure monitoring.
c. Provides clinician with unlimited access to numerous blood gas samples.
d. Used mostly in the critically ill and unstable mechanically ventilated patient.
e. Radial and femoral arteries are sites of choice for indwelling catheter.
f. Umbilical artery often is used for catheter placement in the newborn.
g. An umbilical artery line is inserted through the umbilicus into one of the two umbilical arteries.
h. A chest radiograph must be obtained after insertion to confirm proper placement in vessel.
C Obtaining capillary blood gases (CBGs)
D Comparison of CBG and ABG values
1. CBG Po2 values are approximately 10 to 15 mm Hg less than actual ABG values. The difference between CBG and ABG Po2 values becomes greater as the Po2 values increase.
2. The Pco2 values are consistent in most circumstances but may differ up to 3 mm Hg (CBG values greater than ABG values).
3. The CBG pH values tend to be consistent with the ABG pH values but may be 0.01 to 0.02 pH unit lower.
E Blood gas abnormalities of the newborn
a. Metabolic acidosis normally is a result of hypoxemia (lactic acidosis).
b. It is the most common acid-base problem of newborns.
d. These acids are excreted from the kidneys, not the lungs (nonvolatile acids).
e. Premature newborns have immature phosphate and ammonia buffer systems and cannot handle the excessive buildup of metabolic acids.
f. Newborns may develop persistent metabolic acidosis that:
h. Respiratory management includes oxygenation and ventilation if needed.
i. Management of prolonged metabolic acidosis (not responsive to oxygenation) includes: