1 Assessing childhood illness
Talking to children and their families
What do families want?
| Parents’ thoughts | Doctor’s thoughts |
| ‘Sam coughs at night’ | ‘Sam coughs at night’ |
| ‘It keeps all of us awake’ | ‘His brother has asthma’ |
| ‘He’s had chest infections before’ | ‘It’s probably viral-induced wheeze’ |
| ‘He needs antibiotics’ | ‘Maybe he needs an inhaler’ |
| ‘The doctor will give me a prescription’ | ‘I need to make a diagnosis’ |
Be prepared
General principles
History of presenting complaint
Past medical history
Family and social history
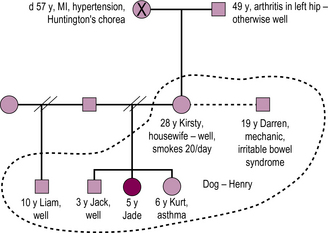
This history is about placing a child within a context (see also Figure 1.1).
Examining children
First impressions
| The well child | The sick child |
| 1. Plays | 1. Quiet |
| 2. Feeds | 2. Still |
| 3. Interacts | 3. Pale |
| 4. Smiles | 4. Drowsy |
| 5. Responds | 5. Unresponsive |
Making friends
 Examine the child while the child is sitting on the parent’s lap
Examine the child while the child is sitting on the parent’s lap
 Play games – incorporate examinations into games
Play games – incorporate examinations into games
 Rehearse examinations on yourself, a parent or a cuddly toy
Rehearse examinations on yourself, a parent or a cuddly toy
 Flexibility – examine available systems first
Flexibility – examine available systems first
 Leave unpleasant examinations until last, e.g. throat examination
Leave unpleasant examinations until last, e.g. throat examination
A practical approach
A practical approach to the examination of a child is shown in Box 1.2.
Box 1.2
Use your senses
| 1. LOOK | Observations: Sick or not? Bright and alert? |
| Distressed? | |
| Appearance: colour, rashes, eyes | |
| Chest movement, respiratory effort | |
| Gait, coordination | |
| 2. FEEL | Fever, hands, pulse, perfusion |
| Vocal fremitus, cardiac apex, abdomen | |
| 3. LISTEN | Cry, cough, stridor |
| Heart sounds, breath sounds, bowel sounds | |
| 4. MOVE | Joints, coordination, neck stiffness |
| 5. CHECK | Ears, nose then throat |
| 6. LAST OF ALL | Plot the child’s height and weight (and, for young children, head circumference) on the growth chart |
Principles of defensible documentation
 Identify the patient – write the child’s name on each sheet of paper
Identify the patient – write the child’s name on each sheet of paper
 Identify yourself; if your signature is illegible, print your name clearly beneath your signature or use a stamp
Identify yourself; if your signature is illegible, print your name clearly beneath your signature or use a stamp
 Use only accepted abbreviations
Use only accepted abbreviations
 Never use the notes to make subjective or abusive remarks about the patient, parents or colleagues
Never use the notes to make subjective or abusive remarks about the patient, parents or colleagues
 Be accurate; patients and parents are rightly angry when information about them is incorrectly or inadequately documented
Be accurate; patients and parents are rightly angry when information about them is incorrectly or inadequately documented
 Take note of what is already documented, e.g. it is indefensible to prescribe penicillin to an allergic patient if that information is in the notes.
Take note of what is already documented, e.g. it is indefensible to prescribe penicillin to an allergic patient if that information is in the notes.
Summary
Finally, consider what you have found from your history and examination. Are there any inconsistencies or concerning features? If so, consider whether the child could be at risk of harm. Take advice from an experienced colleague, and always act in the best interests of the child (see Box 1.2).