Free-flowing ascites conforms to shape of surrounding structures and flows to dependent recesses
• Exudative ascites: Typically demonstrates increasing density of fluid with increasing protein content
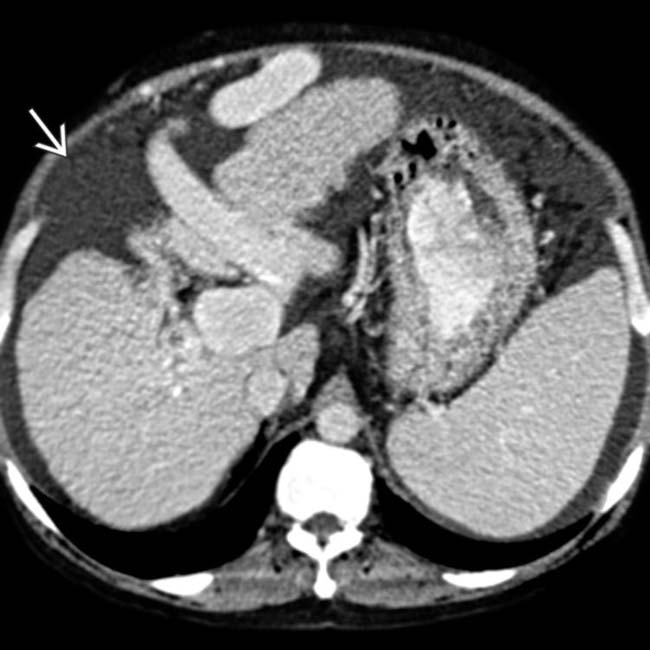
 due to hepatic cirrhosis, with large varices and splenomegaly. Notice the relatively simple, uncomplicated appearance of this transudative ascites.
due to hepatic cirrhosis, with large varices and splenomegaly. Notice the relatively simple, uncomplicated appearance of this transudative ascites.
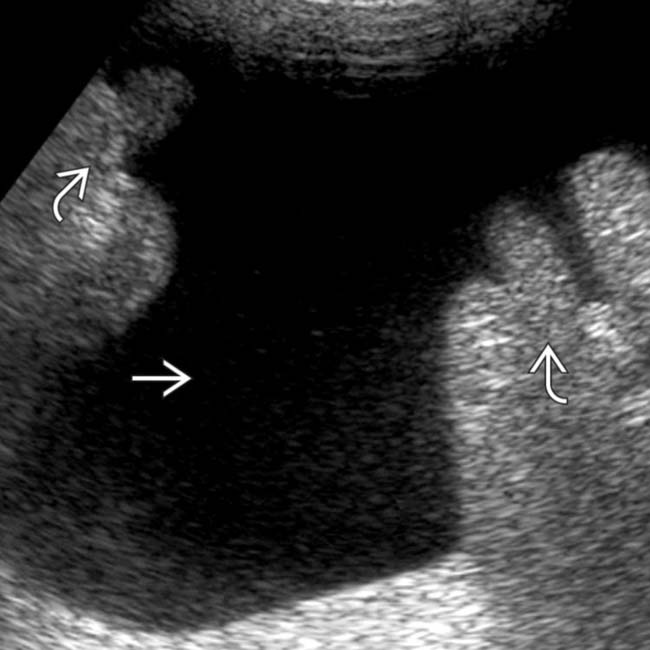
 in the lower abdomen displacing bowel loops
in the lower abdomen displacing bowel loops  in a patient with cirrhosis. As in this case, simple transudative ascites is classically anechoic, freely mobile, and shows acoustic enhancement.
in a patient with cirrhosis. As in this case, simple transudative ascites is classically anechoic, freely mobile, and shows acoustic enhancement.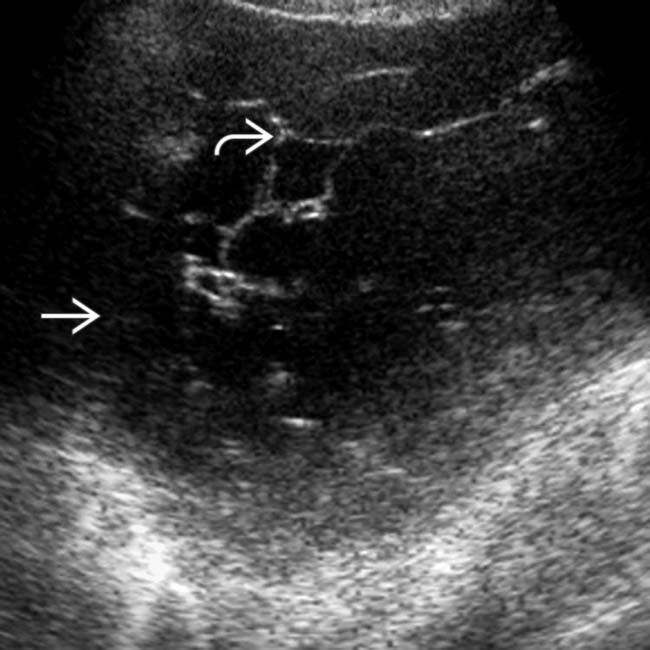
 in a cirrhotic patient. The fluid was non-mobile and loculated on real-time scanning, and there are multiple internal septations
in a cirrhotic patient. The fluid was non-mobile and loculated on real-time scanning, and there are multiple internal septations  , suggesting this is not simple transudative ascites. The ascites fluid was found to be infected.
, suggesting this is not simple transudative ascites. The ascites fluid was found to be infected.IMAGING
General Features
• Morphology
CT Findings
• Transudative ascites
 Small amounts of ascites typically seen in right perihepatic space, Morison pouch, and pouch of Douglas
Small amounts of ascites typically seen in right perihepatic space, Morison pouch, and pouch of Douglas
 Small amounts of ascites typically seen in right perihepatic space, Morison pouch, and pouch of Douglas
Small amounts of ascites typically seen in right perihepatic space, Morison pouch, and pouch of Douglas• Exudative ascites
 Exudative ascites typically demonstrates increasing density of fluid with increasing protein content
Exudative ascites typically demonstrates increasing density of fluid with increasing protein content
 Ascites related to peritoneal carcinomatosis: Complex ascites with nodularity and thickening of adjacent peritoneum and frequent loculation of ascites
Ascites related to peritoneal carcinomatosis: Complex ascites with nodularity and thickening of adjacent peritoneum and frequent loculation of ascites
 Chylous ascites: Intraperitoneal and extraperitoneal fluid usually of water density, but can be < 0 HU or demonstrate fat-fluid levels (due to fat content)
Chylous ascites: Intraperitoneal and extraperitoneal fluid usually of water density, but can be < 0 HU or demonstrate fat-fluid levels (due to fat content)
 Bile ascites: Low density fluid (usually < 15 HU) most typically localized adjacent to liver or biliary structures
Bile ascites: Low density fluid (usually < 15 HU) most typically localized adjacent to liver or biliary structures
 Urinary ascites: Low density fluid (< 15 HU) usually localized adjacent to urinary tract (and site of leak)
Urinary ascites: Low density fluid (< 15 HU) usually localized adjacent to urinary tract (and site of leak)
 Exudative ascites typically demonstrates increasing density of fluid with increasing protein content
Exudative ascites typically demonstrates increasing density of fluid with increasing protein content
 Ascites related to peritoneal carcinomatosis: Complex ascites with nodularity and thickening of adjacent peritoneum and frequent loculation of ascites
Ascites related to peritoneal carcinomatosis: Complex ascites with nodularity and thickening of adjacent peritoneum and frequent loculation of ascites Chylous ascites: Intraperitoneal and extraperitoneal fluid usually of water density, but can be < 0 HU or demonstrate fat-fluid levels (due to fat content)
Chylous ascites: Intraperitoneal and extraperitoneal fluid usually of water density, but can be < 0 HU or demonstrate fat-fluid levels (due to fat content) Bile ascites: Low density fluid (usually < 15 HU) most typically localized adjacent to liver or biliary structures
Bile ascites: Low density fluid (usually < 15 HU) most typically localized adjacent to liver or biliary structures
 Urinary ascites: Low density fluid (< 15 HU) usually localized adjacent to urinary tract (and site of leak)
Urinary ascites: Low density fluid (< 15 HU) usually localized adjacent to urinary tract (and site of leak)
MR Findings
• Exudative: Usually simple fluid signal on T1WI and T2WI, but internal complexity and protein can result in intermediate T1 and T2 signal
Ultrasonographic Findings
• Uncomplicated ascites
 Free fluid forms acute angles where fluid borders organs, should shift with changes in patient position, and should compress with increased transducer pressure
Free fluid forms acute angles where fluid borders organs, should shift with changes in patient position, and should compress with increased transducer pressure
 Free fluid forms acute angles where fluid borders organs, should shift with changes in patient position, and should compress with increased transducer pressure
Free fluid forms acute angles where fluid borders organs, should shift with changes in patient position, and should compress with increased transducer pressureDIFFERENTIAL DIAGNOSIS
Hemoperitoneum
PATHOLOGY
General Features
CLINICAL ISSUES
Presentation
 . Notice the presence of discrete nodules
. Notice the presence of discrete nodules  within the ascites fluid, reflecting the fact that this is malignant ascites in a patient with peritoneal carcinomatosis from appendiceal cancer.
within the ascites fluid, reflecting the fact that this is malignant ascites in a patient with peritoneal carcinomatosis from appendiceal cancer.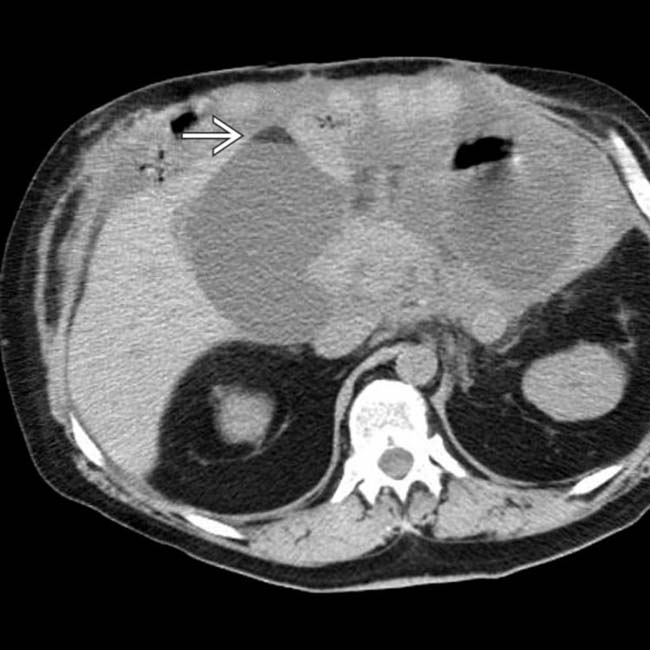
 within fluid collections that indicate the chylous nature of the fluid and that it represents leakage from small bowel lymphatics.
within fluid collections that indicate the chylous nature of the fluid and that it represents leakage from small bowel lymphatics.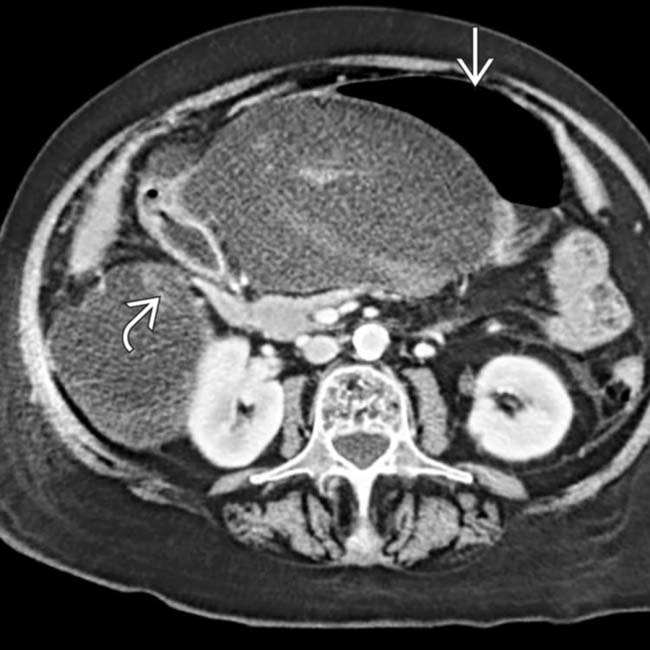
 and duodenum
and duodenum  in this case, is usually due to a local source (e.g., pancreatitis, gastric ulcer), peritonitis, or carcinomatosis.
in this case, is usually due to a local source (e.g., pancreatitis, gastric ulcer), peritonitis, or carcinomatosis.
 in the pelvis. Notice the extensive peritoneal thickening
in the pelvis. Notice the extensive peritoneal thickening  and hyperenhancement more posteriorly in the pelvis, consistent with this patient’s malignant ascites and peritoneal carcinomatosis.
and hyperenhancement more posteriorly in the pelvis, consistent with this patient’s malignant ascites and peritoneal carcinomatosis.
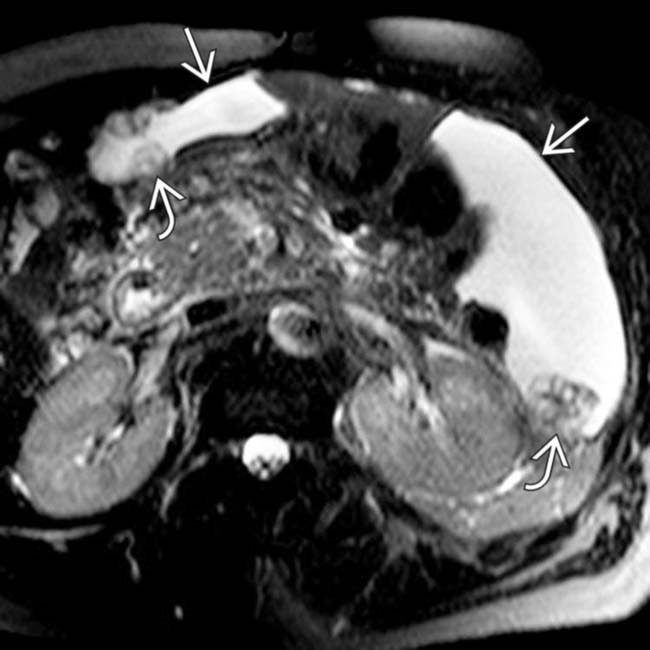
 , compatible with malignancy. Extensive ascites is present with nodular thickening of the parietal peritoneum
, compatible with malignancy. Extensive ascites is present with nodular thickening of the parietal peritoneum  , indicating malignant ascites from gastric carcinoma.
, indicating malignant ascites from gastric carcinoma.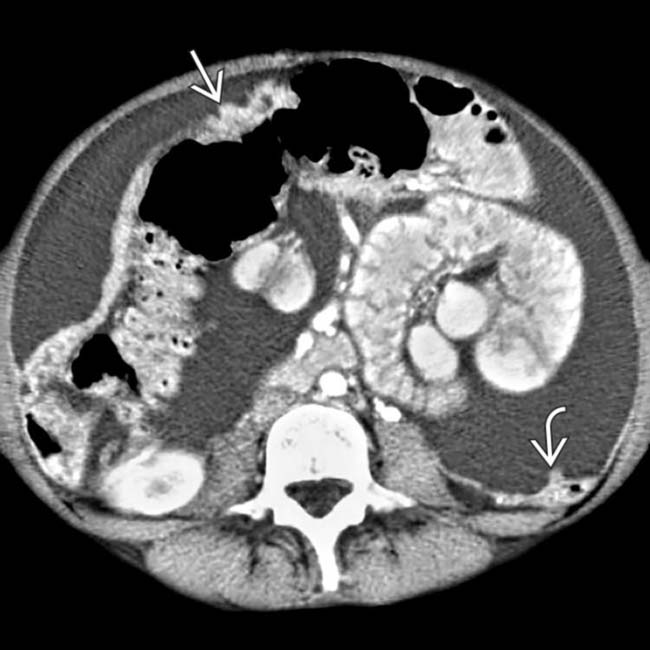
 . Note the nodular thickening of the parietal peritoneum
. Note the nodular thickening of the parietal peritoneum  . GI malignancies are the most common source of malignant ascites in men.
. GI malignancies are the most common source of malignant ascites in men.

 .
.

 . Diagnosis was malignant ascites.
. Diagnosis was malignant ascites.
 , and nodular omentum. Diagnosis was ovarian carcinoma metastases.
, and nodular omentum. Diagnosis was ovarian carcinoma metastases.
 , and varices
, and varices  . The intrahepatic ducts are dilated with an abnormal arborization due to primary sclerosing cholangitis in this case of transudative ascites.
. The intrahepatic ducts are dilated with an abnormal arborization due to primary sclerosing cholangitis in this case of transudative ascites.
 (higher density, heterogeneous) in the perisplenic region and a large hemoperitoneum. The free-flowing blood around the liver
(higher density, heterogeneous) in the perisplenic region and a large hemoperitoneum. The free-flowing blood around the liver  measured 35-45 HU.
measured 35-45 HU.
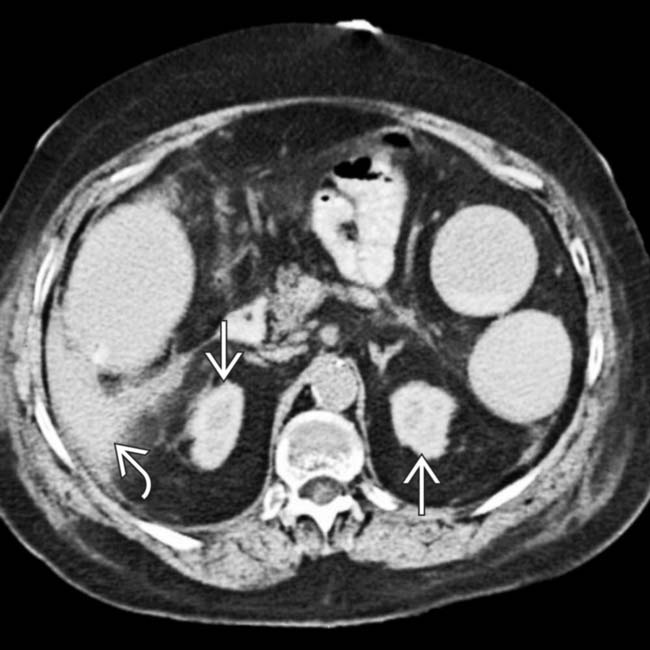
 , mesenteric infiltration, and ascites
, mesenteric infiltration, and ascites  in this patient with Henoch Schönlein purpura. Steroid treatment resulted in prompt resolution of symptoms.
in this patient with Henoch Schönlein purpura. Steroid treatment resulted in prompt resolution of symptoms.
 . Ascites lies medial to the diaphragm and nodular thickening on the diaphragm undersurface represents malignant implants on the parietal peritoneum
. Ascites lies medial to the diaphragm and nodular thickening on the diaphragm undersurface represents malignant implants on the parietal peritoneum  . Note pleural implant
. Note pleural implant  .
.




























































 .
.
 with infiltration of the mesentery, loculated ascites, and enlargement of mesenteric nodes
with infiltration of the mesentery, loculated ascites, and enlargement of mesenteric nodes  .
.
 compatible with contrast-induced nephropathy. Ascites
compatible with contrast-induced nephropathy. Ascites  measured 60 HU due to vicarious excretion of the contrast medium from the peritoneum as a means of compensating for failed renal excretion.
measured 60 HU due to vicarious excretion of the contrast medium from the peritoneum as a means of compensating for failed renal excretion.


