Chapter 50 Arthroscopy of the Foot and Ankle
Ankle Arthroscopy
Arthroscopic Examination and Débridement of the Ankle Joint
 For routine ankle arthroscopy, place the patient supine, with the operative extremity in a leg holder such that the hip and knee are flexed, with the foot hanging free, resulting in gravity-assisted distraction. This also allows free ankle range of motion, which can assist in access to different parts of the ankle (Fig. 50-1).
For routine ankle arthroscopy, place the patient supine, with the operative extremity in a leg holder such that the hip and knee are flexed, with the foot hanging free, resulting in gravity-assisted distraction. This also allows free ankle range of motion, which can assist in access to different parts of the ankle (Fig. 50-1).
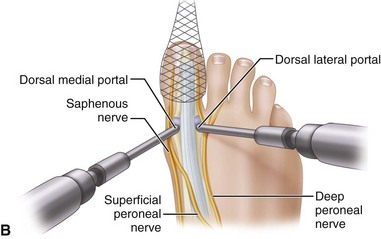
 Mark portal placement after establishing the path of the superficial peroneal nerve, which can be seen subcutaneously after plantar flexion and inversion of the foot (Fig. 50-2).
Mark portal placement after establishing the path of the superficial peroneal nerve, which can be seen subcutaneously after plantar flexion and inversion of the foot (Fig. 50-2).
 Mark anterolateral and anteromedial portals at the joint line, which can be palpated, staying away from the peroneal nerve (Fig. 50-3).
Mark anterolateral and anteromedial portals at the joint line, which can be palpated, staying away from the peroneal nerve (Fig. 50-3).
 After Esmarch exsanguination of the extremity and inflation of the thigh tourniquet, establish the anteromedial portal by inserting an 18-gauge spinal needle at the marked site and insufflating the joint with saline to ensure intraarticular placement and to provide more space for introduction of the blunt trocar (Fig. 50-4). Successful insufflation occurs when there is minimal resistance to the introduction of saline, when the foot dorsiflexes as the joint capsule becomes tight, and when there is backflow of the saline into the syringe after the joint is maximally distended. The anteromedial portal is established first, because there are fewer structures at risk than with the anterolateral portal.
After Esmarch exsanguination of the extremity and inflation of the thigh tourniquet, establish the anteromedial portal by inserting an 18-gauge spinal needle at the marked site and insufflating the joint with saline to ensure intraarticular placement and to provide more space for introduction of the blunt trocar (Fig. 50-4). Successful insufflation occurs when there is minimal resistance to the introduction of saline, when the foot dorsiflexes as the joint capsule becomes tight, and when there is backflow of the saline into the syringe after the joint is maximally distended. The anteromedial portal is established first, because there are fewer structures at risk than with the anterolateral portal.
 After localization of the anteromedial portal with the spinal needle, make a skin incision just large enough to insert the cannula. A large incision allows more extravasation of fluid into the surrounding soft tissues and can make the procedure more difficult.
After localization of the anteromedial portal with the spinal needle, make a skin incision just large enough to insert the cannula. A large incision allows more extravasation of fluid into the surrounding soft tissues and can make the procedure more difficult.
 Further penetrate the joint with a blunt straight hemostat to avoid damage to the saphenous nerve, which is at risk in this area.
Further penetrate the joint with a blunt straight hemostat to avoid damage to the saphenous nerve, which is at risk in this area.
 Place a 2.7-mm 30-degree arthroscope into the anteromedial portal, and establish the anterolateral portal by direct visualization of a spinal needle introduced at the site of the anticipated portal placement.
Place a 2.7-mm 30-degree arthroscope into the anteromedial portal, and establish the anterolateral portal by direct visualization of a spinal needle introduced at the site of the anticipated portal placement.
 When appropriate needle placement is seen, make the skin incision for the anterolateral portal and penetrate the joint with a blunt instrument (Fig. 50-5); then introduce the arthroscopic shaver in this portal.
When appropriate needle placement is seen, make the skin incision for the anterolateral portal and penetrate the joint with a blunt instrument (Fig. 50-5); then introduce the arthroscopic shaver in this portal.
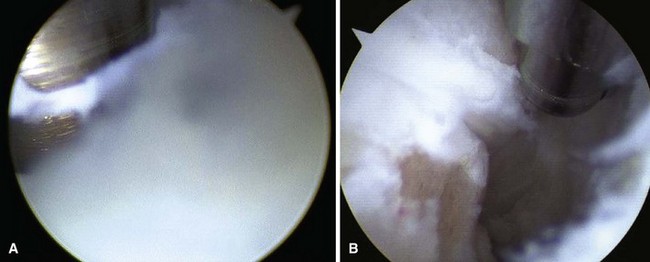
 Inspect the lateral aspect of the joint with use of instruments in the anterolateral portal as needed for débridement (Fig. 50-6), and then switch portals (arthroscope in the anterolateral portal and instruments in the anteromedial portal) for treatment of the medial side of the joint (Fig. 50-7).
Inspect the lateral aspect of the joint with use of instruments in the anterolateral portal as needed for débridement (Fig. 50-6), and then switch portals (arthroscope in the anterolateral portal and instruments in the anteromedial portal) for treatment of the medial side of the joint (Fig. 50-7).
 Noninvasive distraction can be used if needed to access the deeper aspects of the joint (Fig. 50-8). Occasionally, a posterolateral portal is needed to treat pathological processes in the posterior aspect of the ankle that cannot be reached even after distraction is applied.
Noninvasive distraction can be used if needed to access the deeper aspects of the joint (Fig. 50-8). Occasionally, a posterolateral portal is needed to treat pathological processes in the posterior aspect of the ankle that cannot be reached even after distraction is applied.
 After the procedure is completed, close the portals with suture to avoid the development of a fistula, which is a reported complication of ankle arthroscopy.
After the procedure is completed, close the portals with suture to avoid the development of a fistula, which is a reported complication of ankle arthroscopy.
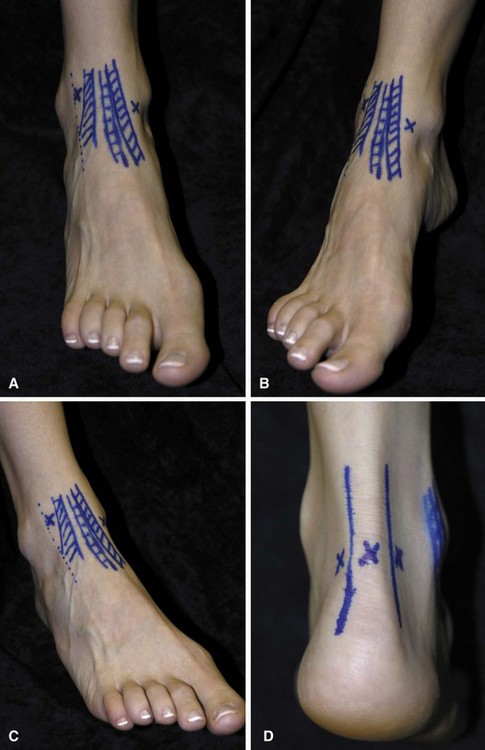
FIGURE 50-3 A, Two anterior portals for ankle arthroscopy are marked in relation to anterior tibial and other extensor tendons where they cross anterior aspect of ankle. B, Anteromedial portal site. C, Anterolateral portal site. D, Posterior portals. SEE TECHNIQUE 50-1.
Ankle Impingement Syndromes
Posterior Ankle Impingement
Patients with posterior ankle impingement point to the back of the ankle as the area of pain and have tenderness in the deep posterior aspect of the ankle and pain with a forced plantar flexion test (Fig. 50-9). Studies may show an os trigonum or hypertrophic posterior process of the talus, and patients obtain relief with a fluoroscopic-guided injection in the area.
Posterior Débridement for Ankle Impingement
 Place the patient prone with the foot at the end of the bed and a support under the lower leg so that the foot hangs freely (Fig. 50-10A). Keeping the foot in neutral with respect to dorsiflexion/plantar flexion and varus/valgus is the safest position in which to avoid neurovascular damage.
Place the patient prone with the foot at the end of the bed and a support under the lower leg so that the foot hangs freely (Fig. 50-10A). Keeping the foot in neutral with respect to dorsiflexion/plantar flexion and varus/valgus is the safest position in which to avoid neurovascular damage.
 Make the posterolateral portal just superior to a line from the tip of the lateral malleolus to the Achilles tendon, just lateral to the tendon (Fig. 50-10B). Insert a hemostat through a small skin incision, aiming along a line directed to the first web space of the forefoot, until it hits bone (Fig. 50-10C).
Make the posterolateral portal just superior to a line from the tip of the lateral malleolus to the Achilles tendon, just lateral to the tendon (Fig. 50-10B). Insert a hemostat through a small skin incision, aiming along a line directed to the first web space of the forefoot, until it hits bone (Fig. 50-10C).
 Make the posteromedial portal at the same level, just medial to the Achilles tendon, and insert a hemostat through the skin incision, directing it to contact the arthroscope at a 90-degree angle (Fig. 50-10D). Once the hemostat contacts the arthroscope, move it down the shaft until it hits bone and can be seen through the scope. If desired, use fluoroscopy to confirm appropriate placement.
Make the posteromedial portal at the same level, just medial to the Achilles tendon, and insert a hemostat through the skin incision, directing it to contact the arthroscope at a 90-degree angle (Fig. 50-10D). Once the hemostat contacts the arthroscope, move it down the shaft until it hits bone and can be seen through the scope. If desired, use fluoroscopy to confirm appropriate placement.
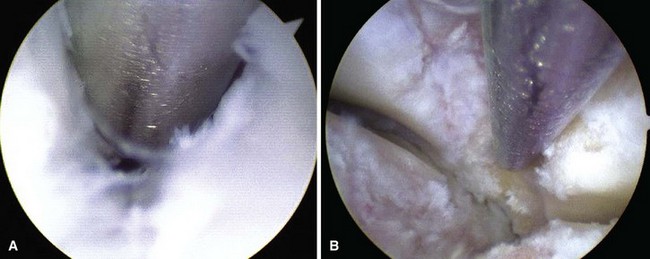
 Place a shaver in this portal and remove the posterior subtalar capsule (Fig. 5-10E). Take care to stay lateral to the flexor hallucis longus tendon to avoid damage to the neurovascular bundle (Fig. 5-10F).
Place a shaver in this portal and remove the posterior subtalar capsule (Fig. 5-10E). Take care to stay lateral to the flexor hallucis longus tendon to avoid damage to the neurovascular bundle (Fig. 5-10F).
 To remove the os trigonum, partially detach the posterior talofibular ligament and posterior talocalcaneal ligament and release the flexor retinaculum to expose the bone to be removed (Fig. 50-10G).
To remove the os trigonum, partially detach the posterior talofibular ligament and posterior talocalcaneal ligament and release the flexor retinaculum to expose the bone to be removed (Fig. 50-10G).
 If distraction is needed, a transcalcaneal traction pin can be hooked to a traction device.
If distraction is needed, a transcalcaneal traction pin can be hooked to a traction device.


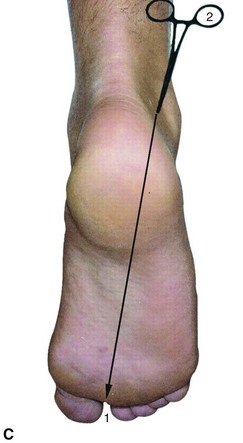
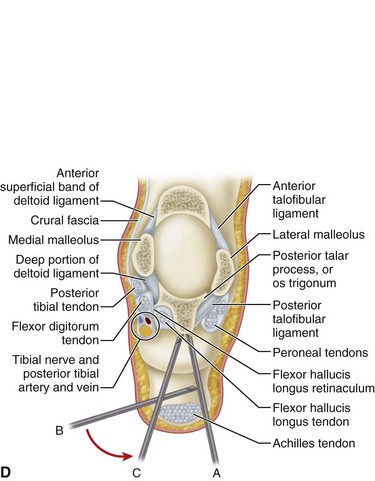

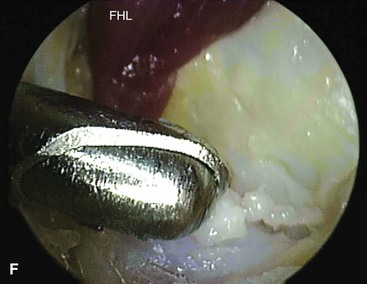
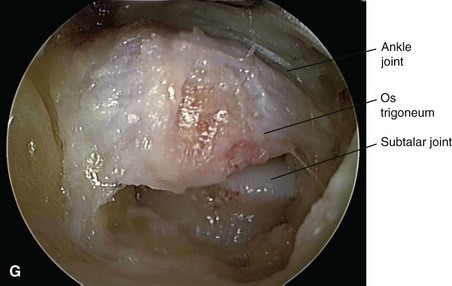
FIGURE 50-10 Posterior débridement for ankle impingement. A, Patient positioning. B, Posterolateral portal. C, Insertion of hemostat aimed along line directed to first web space. D, Insertion of arthroscope through posteromedial portal. E, Insertion of arthroscopic shaver. F, Identification of flexor hallucis longus. G, Exposure of os trigonum. SEE TECHNIQUE 50-2.
Osteochondral Lesions of the Talus
Osteochondral lesions of the talus can be treated arthroscopically and the current grade of recommendation is grade B (fair evidence), according to the literature that is currently available. Ankle arthroscopy is performed as described earlier; noninvasive distraction often is necessary to allow room for the instruments for subchondral penetration. A more thorough discussion of osteochondral lesions of the talus is given in Chapter 89.
Ankle Arthrodesis
Arthrodesis of the ankle can be done arthroscopically, avoiding large incisions in patients with a poor soft tissue envelope and minimal deformity. Once standard anterolateral and anteromedial portals have been established and noninvasive distraction applied, curets and shavers are used to remove articular cartilage. An arthroscopic burr is then used to abrade the subchondral bone (Fig. 50-11). Complete joint preparation can be time consuming and tedious, but care should be taken to be thorough and complete. Percutaneous 6.5-mm or 7.0-mm screws can be placed across the joint with the help of fluoroscopy (Fig. 50-12).
Other Indications
Arthrofibrosis
Subtalar Arthroscopy
 The setup for subtalar arthroscopy is similar to that for ankle arthroscopy, with the operative extremity placed in a leg holder, the hip and knee flexed, and the foot hanging free. Alternatively, the patient can be placed in the lateral decubitus position with the foot hanging off a bump.
The setup for subtalar arthroscopy is similar to that for ankle arthroscopy, with the operative extremity placed in a leg holder, the hip and knee flexed, and the foot hanging free. Alternatively, the patient can be placed in the lateral decubitus position with the foot hanging off a bump.
 After insufflation of the joint, establish the central portal and then the anterolateral portal by direct visualization using a spinal needle (Fig. 50-13).
After insufflation of the joint, establish the central portal and then the anterolateral portal by direct visualization using a spinal needle (Fig. 50-13).
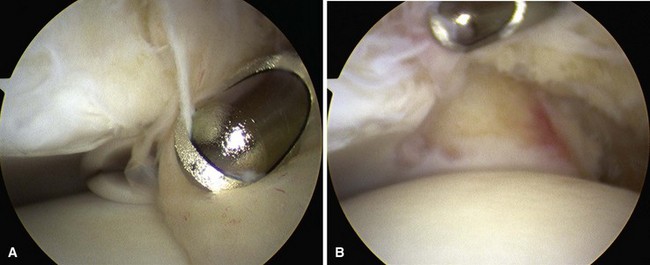
 Often, visualization of the joint is difficult when the arthroscope first enters the joint because of the synovitis that fills the sinus tarsi (Fig. 50-14A). After triangulation to place portals, continue débridement until the joint can be visualized.
Often, visualization of the joint is difficult when the arthroscope first enters the joint because of the synovitis that fills the sinus tarsi (Fig. 50-14A). After triangulation to place portals, continue débridement until the joint can be visualized.
 Débride the anterior aspect of the posterior facet, including the often attenuated interosseous talocalcaneal ligament (Fig. 50-14B).
Débride the anterior aspect of the posterior facet, including the often attenuated interosseous talocalcaneal ligament (Fig. 50-14B).
 Rotate the instruments to the lateral aspect of the posterior facet where débridement of synovitis often is necessary (Fig. 50-15). Switch portals as needed for better access. Occasionally, a posterolateral portal is necessary for posterior access.
Rotate the instruments to the lateral aspect of the posterior facet where débridement of synovitis often is necessary (Fig. 50-15). Switch portals as needed for better access. Occasionally, a posterolateral portal is necessary for posterior access.
 The subtalar joint can also be approached through posterior portals, similar to that described for posterior ankle arthroscopy.
The subtalar joint can also be approached through posterior portals, similar to that described for posterior ankle arthroscopy.
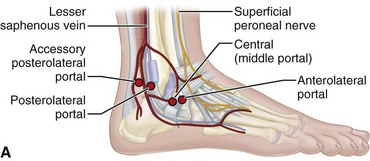
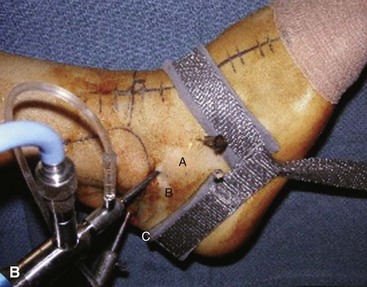
FIGURE 50-13 Subtalar portals must be made carefully to avoid neurovascular injury. A, Anterolateral portal. B, Central portal. C, Posterolateral portal. SEE TECHNIQUE 50-3.
First Metatarsophalangeal Joint Arthroscopy
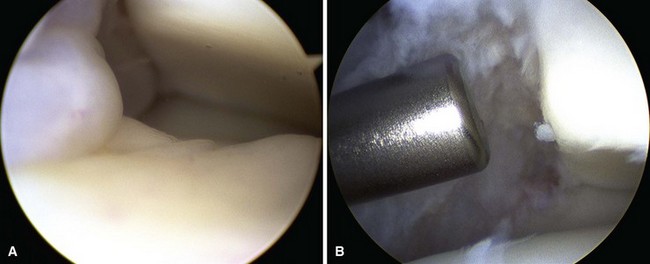
First metatarsophalangeal joint arthroscopy can be used to treat osteochondral lesions of the first metatarsal head (Fig. 50-16), early osteophytosis, chondromalacia, loose bodies, arthrofibrosis, synovitis, and gouty arthritis. Arthroscopic or arthroscopic-assisted techniques have been described for first metatarsophalangeal joint arthrodesis, with a soft tissue release for hallux valgus before a distal first metatarsal osteotomy.

FIGURE 50-16 A, First metatarsophalangeal joint osteochondral lesion. B, After débridement and microfracture.
First Metatarsophalangeal Joint Arthroscopy
Tendoscopy
Tendoscopy of the peroneal tendons (Fig. 50-18) and posterior tibial tendons (Fig. 50-19) has been described and can be used for tenosynovectomy for tendinitis and groove deepening for peroneal dislocation. Endoscopic procedures also can be helpful for conditions around the Achilles tendon (Fig. 50-20). Endoscopic calcaneoplasty and débridement of the retrocalcaneal space has good to excellent results in 80% to 100% of patients.
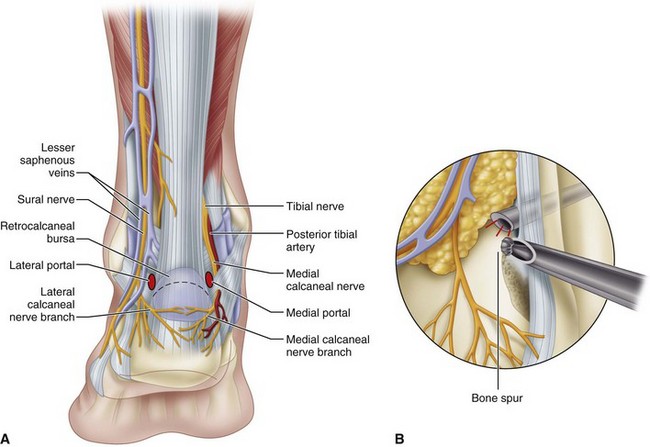
FIGURE 50-20 A, Achilles tendoscopy portals. B, Excision of Haglund deformity with scope through medial portal and burr laterally.
(From Ferkel RD, Hommen JP: Arthroscopy of the ankle and foot. In Coughlin MJ, Mann RA, Saltzman CL, editors: Surgery of the foot and ankle, ed 8, Philadelphia, 2007, Elsevier.)
Allegra F, Maffulli N. Double posteromedial portals for posterior ankle arthroscopy. Clin Orthop Relat Res. 2010;468:996.
Aurich M, Bedi HS, Smith PJ, et al. Arthroscopic treatment of osteochondral lesions of the ankle with matrix-associated chondrocyte implantation: early clinical and magnetic resonance imaging results. Am J Sports Med. 2011;39:311.
Baums MH, Kahl E, Schultz W, Klinger HM. Clinical outcome of the arthroscopic management of sports-related “anterior ankle pain”: a prospective study. Knee Surg Sports Traumatol Arthrosc. 2006;14:482.
Beals TC, Junko JT, Amendola A, et al. Minimally invasive distraction technique for prone posterior ankle and subtalar arthroscopy. Foot Ankle Int. 2010;31:316.
Berlet GC, Saar WE, Ryan A, Lee TH. Thermal-assisted capsular modification for functional ankle instability. Foot Ankle Clin. 2002;7:567.
Boack DH, Manegold S. Peripheral talar fractures. Injury. 2004;35(Suppl 2):SB23.
Calder JD, Sexton SA, Pearce CJ. Return to training and playing after posterior ankle arthroscopy for posterior impingement in elite professional soccer. Am J Sports Med. 2010;38:120.
Cameron SE, Ullrich P. Arthroscopic arthrodesis of the ankle joint. Arthroscopy. 2000;16:21.
Choi WJ, Lee JW, Han SH, et al. Chronic lateral ankle instability: the effect of intra-articular lesions on clinical outcome. Am Sports Med. 2008;36:2167.
Collman DR, Kaas MH, Schuberth JM. Arthroscopic ankle arthrodesis: factors influencing union in 39 consecutive patients. Foot Ankle Int. 2006;27:1079.
Corte-Real NM, Moriera RM. Arthoscopic repair of chronic lateral ankle instability. Foot Ankle Int. 2009;30:213.
Cui Q, Milbrandt T, Millington S, et al. Treatment of posttraumatic adhesive capsulitis of the ankle: a case series. Foot Ankle Int. 2005;26:602.
Dannawi Z, Nawabi DH, Patel A, et al. Arthroscopic ankle arthrodesis: are results reproducible irrespective of pre-operative deformity? Foot Ankle Surg. 2011;17:294.
Deng DE, Hamilton GA, Lee M, et al. Complications associated with foot and ankle arthroscopy. J Foot Ankle Surg. 2012;51:281.
Dodd A, Simon D, Wilkinson R. Arthroscopically assisted transfibular talar dome fixation with a headless screw. Arthroscopy. 2009;25:806.
Ferkel RD, Chams RN. Chronic lateral instability: arthroscopic findings and long-term results. Foot Ankle Int. 2007;28:24.
Ferkel RD, Hewitt M. Long-term results of arthroscopic ankle arthrodesis. Foot Ankle Int. 2005;26:275.
Galla M, Lobenhoffer P. Technique and results of arthroscopic treatment of posterior ankle impingement. Foot Ankle Surg. 2011;17:79.
Glazebrook MA, Ganapathy V, Bridge MA, et al. Evidence-based indications for ankle arthroscopy. Arthroscopy. 2009;25:1478.
Gougoulias NE, Agathangelidis FG, Parsons SW. Arthroscopic ankle arthrodesis. Foot Ankle Int. 2007;28:695.
Grishko V, Xu M, Wilson G, Pearsall AW. 4th: Apoptosis and mitochondrial dysfunction in human chondrocytes following exposure to lidocaine, bupivacaine, and ropivacaine. J Bone Joint Surg. 2010;92A:609.
Guo QW, Hu YL, Jiao C, et al. Open versus endoscopic excision of a symptomatic os trigonum: a comparative study of 41 cases. Arthroscopy. 2010;26:384.
Han SH, Lee JW, Kim S, et al. Chronic tibiofibular syndesmosis injury: the diagnostic efficiency of magnetic resonance imaging and comparative analysis of operative treatment. Foot Ankle Int. 2007;28:336.
Hua Y, Chen S, Li Y, et al. Combination of modified Brostrom procedure with ankle arthroscopy for chronic ankle instability accompanied by intra-articular symptoms. Arthroscopy. 2010;26:524.
Imade S, Takao M, Miyamoto W, et al. Leg anterior compartment syndrome following ankle arthroscopy after Maisonneuve fracture. Arthroscopy. 2009;25:215.
Imade S, Takao M, Nishi H, Uchio Y. Arthroscopy-assisted reduction and percutaneous fixation for triplane fracture of the distal tibia. Arthroscopy. 2004;20:e123.
Jacobs TF, Vansintjan PS, Roels N, et al. The effect of lidocaine on the viability of cultivated mature human cartilage cells: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2011;19:1206.
Jang EC, Kwak BK, Song KS, et al. Pseudoaneurysm of the anterior tibial artery after ankle arthroscopy treated with ultrasound-guided compression therapy. J Bone Joint Surg. 2008;90A:2235.
Kashir A, Kiely P, Dar W, D’Souza L. Pseudoaneurysm of the dorsalis pedis artery after ankle arthroscopy. Foot Ankle Surg. 2010;16:151.
Kralinger F, Lutz M, Wambacher M, et al. Arthroscopically assisted reconstruction and percutaneous screw fixation of a pilon tibial fracture. Arthroscopy. 2003;19:E45.
Lee JW, Suh JS, Huh YM, et al. Soft tissue impingement syndrome of the ankle: diagnostic efficacy of MRI and clinical results after arthroscopic treatment. Foot Ankle Int. 2004;25:896.
Leetun DT, Ireland ML. Arthroscopically assisted reduction and fixation of a juvenile Tillaux fracture. Arthroscopy. 2002;18:427.
Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg. 2009;91A:333.
Loren GJ, Ferkel RD. Arthroscopic assessment of occult intra-articular injury in acute ankle fractures. Arthroscopy. 2002;18:412.
Lui TH. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23:554.e1.
Lui TH. Ankle arthroscopy with patient in prone position. Arch Orthop Trauma Surg. 2008;128:1283.
Lui TH, Chan WK, Chan KB. the arthroscopic management of frozen ankle. Arthroscopy. 2006;22:283.
Lui TH, Ip K, Chow HT. Comparison of radiologic and arthroscopic diagnoses of distal tibiofibular syndesmosis disruption in acute ankle fracture. Arthroscopy. 2005;21:1370.
Maiotti M, Massoni C, Tarantino U. The use of arthroscopic thermal shrinkage to treat chronic lateral ankle instability in young athletes. Arthroscopy. 2005;21:751.
McGillion S, Jackson M, Lahoti O. Arthroscopically assisted percutaneous fixation of triplane fractures of the distal tibia. J Pediatr Orthop B. 2007;16:313.
Murawski CD, Kennedy JG. Anteromedial impingement in the ankle joint: outcomes following arthroscopy. Am J Sports Med. 2010;38:2017.
Nery C, Raduan F, Del Buono A, et al. Arthroscopic-assisted Broström-Gould for chronic ankle instability: a long-term follow-up. Am J Sports Med. 2011;39:2381.
Nickisch F, Barg A, Saltzman CL, et al. Postoperative complications of posterior ankle and hindfoot arthroscopy. J Bone Joint Surg. 2012;94A:439.
Nielsen KK, Linde F, Jensen NC. The outcome of arthroscopic and open surgery ankle athrodesis: a comparative retrospective study on 107 patients. Foot Ankle Surg. 2008;14:153.
Okuda R, Kinoshita M, Morikawa J, et al. Arthroscopic findings in chronic lateral ankle instability: do focal chondral lesions influence the results of ligament reconstruction? Am J Sports Med. 2005;33:35.
Ono A, Nishikawa S, Nagao A, et al. Arthroscopically assisted treatment of ankle fractures: arthroscopic findings and surgical outcomes. Arthroscopy. 2004;20:627.
Panagopoulos A, van Niekerk L. Arthroscopic assisted reduction and fixation of a juvenile Tillaux fracture. Knee Surg Sports Traumatol Arthrosc. 2007;15:415.
Piper SL, Kramer JD, Kim HT, Feeley BT. Effects of local anesthetics on articular cartilage. Am J Sports Med. 2011;39:2245.
Robinson P, White LM, Salonen DC, et al. Anterolateral ankle impingement: MR arthrographic assessment of the anterolateral recess. Radiology. 2001;221:186.
Schuberth JM, Jenning MM, Lau AC. Arthroscopy-assisted repair of latent syndesmotic instability of the ankle. Arthroscopy. 2008;24:868.
Stutz G, Kuster MS, Kleinstuck F, Gachter A. Arthroscopic management of septic arthritis: stages of infection and results. Knee Surg Sports Traumatol Arthrosc. 2000;8:270.
Subairy A, Subramanian K, Geary NP. Arthroscopically assisted internal fixation of a talus body fracture. Injury. 2004;35:86.
Takao M, Ochi M, Oae K, et al. Diagnosis of a tear of the tibiofibular syndesmosis: the role of arthroscopy of the ankle. J Bone Joint Surg. 2003;85B:324.
Takao M, Uchio Y, Naito K, et al. Diagnosis and treatment of combined intra-articular disorders in acute distal fibular fractures. J Trauma. 2004;57:1202.
Tey M, Monllau JC, Centenera JM, Pelfort X. Benefits of arthroscopic tuberculoplasty in posterior ankle impingement syndrome. Knee Surg Sports Traumatol Arthrosc. 2007;15:1235.
Thaunat M, Billot N, Bauer T, Hardy P. Arthroscopic treatment of a juvenile Tillaux fracture. Knee Surg Sports Traumatol Arthosc. 2007;15:286.
Thordarson DB, Bains R, Shepherd LE. The role of ankle arthroscopy on the surgical management of ankle fractures. Foot Ankle Int. 2001;22:123.
Tol JL, van Dijk CN. Etiology of the anterior ankle impingement syndrome: a descriptive anatomical study. Foot Ankle Int. 2004;25:382.
Jl Tol, Verhagen RAW, Krips R, et al. The anterior ankle impingement syndrome: diagnostic value of oblique radiographs. Foot Ankle Int. 2004;25:63.
Tol JL, Verheyen CP, Van Dijk CN. Arthroscopic treatment of anterior impingement in the ankle: a prospective study with a five-to eight-year followup. J Bone Joint Surg. 2001;83B:9.
Urguden M, Cevikol C, Dabak K, et al. Effect of joint motion on safety of portals in posterior ankle arthroscopy. Arthroscopy. 2009;25:1442.
Utsugi K, Sakai H, Hiraoka H, et al. Intra-articular fibrous tissue formation following ankle fracture: the significance of arthroscopic debridement of fibrous tissue. Arthroscopy. 2007;23:89.
van Dijk CN, Scholten PE, Krips R. A 2-portal endoscopic approach for the diagnosis and treatment of posterior ankle pathology. Arthroscopy. 2000;16:871.
Ventura A, Terzaghi C, Legnani C, Borgo E. Arthroscopic four-step treatment for chronic ankle instability. Foot Ankle Int. 2012;33:29.
Vispo Seara JL, Barthel T, Schmitz H, Eulert J. Arthroscopic treatment of septic joints: prognostic factors. Arch Orthop Trauma Surg. 2002;122:204.
Willits K, Sonneveld H, Amendola A, et al. Outcome of posterior ankle arthroscopy for hindfoot impingement. Arthroscopy. 2008;24:196.
Young BH, Flanigan RM, DiGiovanni BF. Complications of ankle arthroscopy utilizing a contemporary noninvasive distraction technique. J Bone Joint Surg. 2011;93A:963.
Zvijac JE, Lemak L, Schurhoff MR, et al. Analysis of arthroscopically assisted ankle arthrodesis. Arthroscopy. 2002;18:70.
Ahn JH, Lee SK, Kim KJ, et al. Subtalar arthroscopic procedures for the treatment of subtalar pathologic conditions: 115 consecutive cases. Orthopedics. 2009;32:891.
Amendola A, Lee KB, Saltzman CL, Suh JS. Technique and early experience with posterior arthroscopic subtalar arthrodesis. Foot Ankle Int. 2007;28:298.
Lee KB, Bai LB, Song EK, et al. Subtalar arthroscopy for sinus tarsi syndrome: arthroscopic findings and clinical outcomes of 33 consecutive cases. Arthroscopy. 2008;24:1130.
Lee KB, Chung JY, Song EK, et al. Arthroscopic release for painful subtalar stiffness after intra-articular fractures of the calcaneum. J Bone Joint Surg. 2008;90B:1457.
Lee KB, Park CH, Seon JK, Kim MS. Arthroscopic subtalar arthrodesis using a posterior 2-portal approach in the prone position. Arthroscopy. 2010;26:230.
Rammelt S, Gavlik JM, Barthel S, Zwipp H. The value of subtalar arthroscopy in the management of intra-articular calcaneus fractures. Foot Ankle Int. 2002;23:906.
Shazly OE, Nassar W, Badrawy AE. Arthroscopic subtalar fusion for post-traumatic subtalar arthritis. Arthroscopy. 2009;25:783.
Woon CY, Chong KW, Yeo W, et al. Subtalar arthroscopy and fluoroscopy in percutaneous fixation of intra-articular calcaneal fractures: the best of both worlds. J Trauma. 2011;71:917.
First Metatarsophalangeal Joint Arthroscopy
Ahn JH, Choy WS, Lee KW. Arthroscopy of the first metatarsophalangeal joint in 59 consecutive cases. J Foot Ankle Surg. 2012;51:161.
Debnath UK, Hemmady MV, Hariharan K. Indications for and technique of first metatarsophalangeal joint arthroscopy. Foot Ankle Int. 2006;27:1049.
Lui TH. First metatarsophalangeal joint arthroscopy in patients with hallux valgus. Arthroscopy. 2008;24:1122.
Michels F, Guillo S, de Lavigne C, Van Der Bauwhede J. The arthroscopic Lapidus procedure. Foot Ankle Surg. 2011;17:25.
Siclari A, Decantis V. Arthroscopic lateral release and percutaneous distal osteotomy for hallux valgus: a preliminary report. Foot Ankle Int. 2009;30:675.
Vaseeon T, Phisitkul P. Arthroscopic debridement for first metatarsophalangeal joint arthrodesis with a 2- versus 3-portal technique: a cadaveric study. Arthroscopy. 2010;26:1363.
Bulstra GH, Olsthoorn PGM, van Dijk N. Tendoscopy of the posterior tibial tendon. Foot Ankle Clin. 2006;11:421.
Jerosch J, Nasef NM. Endoscopic calcaneoplasty—rationale, surgical technique, and early results: a preliminary report. Knee Surg Sports Traumatol Arthrosc. 2003;11:190.
Komatsu F, Takao M, Innami K, et al. Endoscopic surgery for plantar fasciitis: application of a deep-fascial approach. Arthroscopy. 2011;27:1105.
Leitze Z, Sella EJ, Aversa JM. Endoscopic decompression of the retrocalcaneal space. J Bone Joint Surg. 2003;85A:1488.
Lui TH, Chan KB, Chan LK. Endoscopic distal soft-tissue release in the treatment of hallux valgus: a cadaveric study. Arthroscopy. 2010;26:1111.
Maquirriain J, Ayerza M, Costa-Paz M, Muscolo DL. Endoscopic surgery in chronic Achilles tendinopathies: a preliminary report. Arthroscopy. 2002;18:298.
Ogut T, Ayhan E. Hindfoot endoscopy for accessory flexor digitorum longus and flexor hallucis longus tenosynovitis. Foot Ankle Surg. 2011;17:e7.
Ortmann FW, McBryde AM. Endoscopic bony and soft-tissue decompression of the retrocalcaneal space for the treatment of Haglund deformity and retrocalcaneal bursitis. Foot Ankle Int. 2007;28:149.
Scholten PE, van Dijk N. Endoscopic calcaneoplasty. Foot Ankle Clin. 2006;11:439–446.
Scholten PE, van Dijk N. Tendoscopy of the peroneal tendons. Foot Ankle Clin. 2006;11:415.
Amendola A, Petrik J, Webster-Bogaert S. Ankle arthroscopy: outcome in 79 consecutive patients. Arthroscopy. 1996;12:565.
Barber FA, Click J, Britt BT. Complications of ankle arthroscopy. Foot Ankle. 1990;10:263.
Bonnin M, Bouysset M. Arthroscopy of the ankle: analysis of results and indications on a series of 75 cases. Foot Ankle Int. 1999;20:744.
Corso SJ, Zimmer TJ. Technique and clinical evaluation of arthroscopic ankle arthrodesis. Arthroscopy. 1995;11:585.
Crosby LA, Yee TC, Formanek TS, Fitzgibbons TC. Complications following arthroscopic ankle arthrodesis. Foot Ankle Int. 1996;17:340.
Farooki S, Yao L, Seeger LL. Anterolateral impingement of the ankle: effectiveness of MR imaging. Radiology. 1998;207:357.
Ferkel RD, Fischer SP. Progress in ankle arthroscopy. Clin Orthop Relat Res. 1989;240:210.
Ferkel RD, Heath DD, Guhl JF. Neurological complications of ankle arthroscopy. Arthroscopy. 1996;12:200.
Glick JM, Morgan CD, Myerson MS, et al. Ankle arthrodesis using an arthroscopic method: long-term follow-up of 34 cases. Arthroscopy. 1996;12:428.
Holt ES. Arthroscopic visualization of the tibial plafond during posterior malleolar fracture fixation. Foot Ankle. 1994;15:206.
Jerosch J, Steinbeck J, Schroder M, Reer R. Arthroscopically assisted arthrodesis of the ankle joint. Arch Orthop Trauma Surg. 1996;115:182.
Kibler WB. Arthroscopic findings in ankle ligament reconstruction. Clin Sports Med. 1996;15:799.
Komenda GA, Ferkel RD. Arthroscopic findings associated with the unstable ankle. Foot Ankle Int. 1999;20:708.
Liu SH, Nuccion SL, Finerman G. Diagnosis of anterolateral ankle impingement: comparison between magnetic resonance imaging and clinical examination. Am J Sports Med. 1997;25:389.
Myerson MS, Quill G. Ankle arthrodesis: a comparison of an arthroscopic and an open method of treatment. Clin Orthop Relat Res. 1991;268:84.
O’Brien TS, Hart TS, Shereff MJ, et al. Open versus arthroscopic ankle arthrodesis: a comparative study. Foot Ankle Int. 1999;20:368.
Ogilvie-Harris DJ, Reed SC. Disruption of the ankle syndesmosis: diagnosis and treatment by arthroscopic surgery. Arthroscopy. 1994;10:561.
Parisien JS, Vangsness T. Arthroscopy of the subtalar joint: an experimental approach. Arthroscopy. 1985;1:53.
Saltzman CL, Marsh JL, Tearse DS. Treatment of displaced talus fractures: an arthroscopically assisted approach. Foot Ankle Int. 1994;15:630.
Taga I, Shino K, Inoue M, et al. Articular cartilage lesions in ankles with lateral ligament injury: an arthroscopic study. Am J Sports Med. 1993;21:120.
Turan I, Wredmark T, Fellander-Tsai L. Arthroscopic ankle arthrodesis in rheumatoid arthritis. Clin Orthop Relat Res. 1995;320:110.
van Dijk CN, Bossuyt PM, Marti RK. Medial ankle pain after lateral ligament rupture. J Bone Joint Surg. 1996;78B:562.
van Dijk CN, Scholte D. Arthroscopy of the ankle joint. Arthroscopy. 1997;13:90.
van Dijk CN, Tol JL, Verheyen CCPM. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25:737.
van Dijk CN, Verhagn RAW, Tol JL. Arthroscopy for problems after ankle fracture. J Bone Joint Surg. 1997;79B:280.
Whipple TL, Martin, Dr., McIntyre LF, Meyers JF. Arthroscopic treatment of triplane fractures of the ankle. Arthroscopy. 1993;9:456.
Winson IG, Robinson DE, Allen PE. Arthroscopic ankle arthrodesis. J Bone Joint Surg. 1995;87B:343.
Elgafy H, Ebraheim NA. Subtalar arthroscopy for persistent subfibular pain after calcaneal fractures. Foot Ankle Int. 1999;20:422.
Frey C, Feder KS, DiGiovanni C. Arthroscopic evaluation of the subtalar joint: does sinus tarsi syndrome exist? Foot Ankle Int. 1999;20:185.
Scranton PE. Comparison of open isolated subtalar arthrodesis with autogenous bone graft versus outpatient arthroscopic subtalar arthrodesis using injectable bone morphogenic protein-enhanced graft. Foot Ankle Int. 1999;20:162.
Williams MM, Ferkel RD. Subtalar arthroscopy: indications, technique, and results. Arthroscopy. 1998;14:373.
First Metatarsophalangeal Joint Arthroscopy
Bartlett DH. Arthroscopic management of osteochondritis dissecans of the first metatarsal head. Arthroscopy. 1998;4:51.
Davies MS, Saxby TS. Arthroscopy of the first metatarsophalangeal joint. J Bone Joint Surg. 1999;81B:20.
Iqbal MJ, Chana GS. Arthroscopic cheilectomy for hallux rigidus. Arthroscopy. 1998;14:307.
Jaivin JS, Ferkel RD. Arthroscopy of the foot and ankle. Clin Sports Med. 1994;13:761.
van Dijk CN, Veenstra KM, Nuesch BC. Arthroscopic surgery of the metatarsophalangeal first joint. Arthroscopy. 1998;14:851.