CHAPTER 6 Arthroscopy of the Distal Radioulnar Joint
Anatomy and Biomechanics
The DRUJ is a trochoid diarthrodial articulation that allows both rotation and translation during normal forearm motion. The overall dimensions of the sigmoid notch average 15 mm in the transverse plane and 10 mm in the coronal plane. Its dorsal bony rim is typically acutely angled, whereas the volar rim is more rounded and is frequently augmented by a cartilaginous lip. The shape of the notch varies considerably in both planes, which plays a role in both joint stability and ease of arthroscopic access.1 Due to its relatively shallow and incongruent articulation, the DRUJ relies strongly on the soft tissues for stability. The structures that contribute to DRUJ stability are the pronator quadratus, extensor carpi ulnaris (ECU), interosseous membrane (IOM), DRUJ capsule, and components of the triangular fibrocartilage complex (TFCC).2
During forearm rotation, DRUJ translation occurs because the sigmoid notch is shallow (with a radius of curvature 50% greater than that of the ulnar head). At the extremes of pronation and supination, the ulnar head slides palmarly and dorsally in the sigmoid notch (respectively)—resulting in only 2 to 3 mm of articular contact area at the rims.3 Although DRUJ motion has a substantial translational component (with a changing axis of rotation), its instant axis generally passes near the center of the ulnar head—moving dorsally with pronation and palmarly with supination. The ulnar head serves as the seat for the sigmoid notch, around which the radius rotates.3 The amount of articular cartilage that covers the head varies from a 50-degree to a 130-degree arc.
Surgical Technique
A regional or general anesthetic is administered. The patient is positioned supine on the operating table. An upper-arm tourniquet is applied over cotton padding. The elbow is flexed to 90 degrees and the upper extremity is mounted in a traction tower using finger traps applied to the long and ring fingers. Placing the wrist in full supination facilitates access to the DRUJ, unless the joint becomes excessively tight in this position. In neutral rotation the opposing surfaces of the sigmoid notch and the ulnar head are congruent, whereas in full supination the opposing surfaces have only a marginal contact area of 2 to 3 mm.4
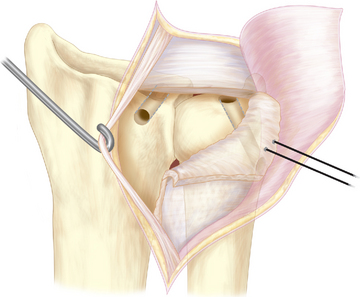
A distal DRUJ portal can be established for instrumentation and improved visualization of the ulnar dome and TFCC. This portal enters between the TFCC central disc and the head of the ulna (Figure 6.1). It should first be localized with a needle while viewing with the arthroscope in the proximal portal.5 The portal is typically used for instruments such as shavers, graspers, and radiofrequency devices.
Arthroscopic Evaluation of the DRUJ
By passing the arthroscope between the TFCC and the dome of the ulnar head, the distal radioulnar ligaments may be visualized from their attachments on the sigmoid notch to their insertion at the fovea of the ulna head. With the arm in neutral rotation, the TFCC is under the least amount of tension—allowing for easier evaluation of the distal articular surface of the ulna. At the fovea, the ulnocapitate ligament may be seen inserting into the ulnar head—just slightly ulnar to the attachments of the radioulnar ligaments.5,6
Pitfalls
Entry into the joint is the most difficult aspect of DRUJ arthroscopy. Keeping the forearm positioned in supination during entry into the DRUJ is important to maximize the dorsal space of the DRUJ. At times, a 1.9-mm scope may be necessary if the joint is tight. Absorption of fluid by the distal radioulnar joint synovium can easily obscure one’s view of the small DRUJ. In the presence of a TFCC tear, fluid inflow from the radiocarpal joint may have already affected the DRUJ.6,7
DRUJ Instability
Arthroscopically assisted TFCC repair, especially for peripheral tears, is common practice (see Chapter 5). In the presence of DRUJ instability, an open TFCC repair directly to the fovea with transosseous sutures is more effective at restoring joint stability. If an arthroscopic or open TFCC repair is not possible due to chronicity and attenuation of the tissues, a secondary reconstruction is indicated. The author’s preferred technique for chronic instability reconstructs both radioulnar ligaments to restore normal joint stability and mechanics.8–11
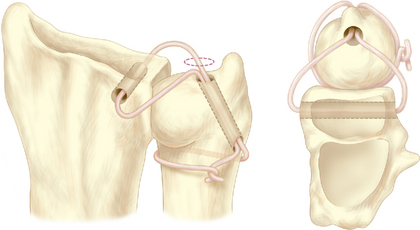
A 5-cm incision is made between the fifth and sixth extensor compartments over the DRUJ. The fifth compartment is opened over the radioulnar joint, and the extensor digiti minimi tendon is retracted. An L-shaped DRUJ capsulotomy is made with one limb along the dorsal rim of the sigmoid notch and the other just proximal to the dorsal radioulnar ligament (Figure 6.2). The ECU sheath is not opened or dissected from the ulnar groove during the procedure. Scar is debrided from the fovea. Functioning remnants of the TFCC are retained.
The other end of the graft is grasped with the hemostat and pulled back along this tract. Both graft limbs are then passed through the ulnar tunnel to exit the ulnar neck. The limbs are passed in opposite directions around the ulnar neck, one passing deep to the ECU sheath. With the forearm in neutral rotation and the DRUJ manually compressed, the limbs are pulled taut, tied together, and secured with sutures (Figure 6.3). The dorsal DRUJ capsule and extensor retinaculum are closed in layers with 3-0 sutures, leaving the EDQ subcutaneous.
1 Tolat AR, Stanley JK, Trail IA. A cadaveric study of the anatomy and stability of the distal radioulnar joint in the coronal and transverse planes. J Hand Surg. 1996;21B(5):587-594.
2 Kihara H, Short WH, Werner FW, Fortino MD, Palmer AK. The stabilizing mechanism of the distal radioulnar joint during pronation and supination. J Hand Surg. 1995;20A:930-936.
3 Ekenstam FA, Hagert CG. Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg. 1985;19:17-25.
4 Ekenstam FA. Anatomy of the distal radioulnar joint. Clin Orthop. 1992;275:14-18.
5 Whipple TL. Arthroscopy of the distal radioulnar joint. Hand Clinics. 1994;10(4):589-592.
6 Leibovic SJ, Bowers WH. Arthroscopy of the distal radioulnar joint. Ortho Clinics of North America. 1995;26(4):755-757.
7 Zelouf DS, Bowers WH. Arthroscopy of the distal radioulnar joint. Hand Clinics. 1999;15(3):475-477.
8 Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg. 2002;27A:243-251.
9 Petersen MS, Adams BD. Biomechanical evaluation of distal radioulnar reconstructions. J Hand Surg. 1993;18A:328-334.
10 Adams BD. Anatomic reconstruction of the distal radioulnar ligaments for DRUJ instability. Techniques in Upper Extremity Surgery. 2000;4:154-160.
11 Adams BD. Distal radioulnar joint instability. In: Green DP, editor. Operative Hand Surgery. Fifth Edition. Philadelphia: Elsevier Churchill Livingstone; 2005:621-624.