CHAPTER 13 Arthroscopy in the Throwing Athlete
Excessive valgus and extension forces are generated during the throwing motion in several sports, especially baseball, tennis, football, and certain track and field events.1 The repetition required to excel in these sports can ultimately lead to fatigue and even failure of key stabilizing structures in the elbow. The medial ulnar collateral ligament (MUCL) is the primary restraint to a valgus load during the throwing motion and is most susceptible to injury after repetitive throwing. MUCL insufficiency leads to valgus instability, a condition that is significant only in overhead athletes. Over time, chronic valgus instability can result in a unique constellation of elbow pathologies that are indicative of repetitive overhead throwing.
Several investigators have described the most common injuries seen in the elbow of the throwing athlete, including MUCL injuries, ulnar neuritis, posteromedial impingement with osteophyte formation, flexor-pronator strain, ulnar stress fractures, osteochondritis dissecans of the capitellum, and capsular contracture.2–8 Although not all pathology in the thrower’s elbow is amenable to arthroscopic management, clinicians who care for throwing athletes must be familiar with all pathologic conditions and comfortable with open and arthroscopic treatments.
ANATOMY
The elbow is a hinge joint with the bony ulnohumeral articulation that provides stability at the extremes of motion, from 0 to 20 degrees of flexion and beyond 120 degrees of flexion.3 The intervening 100 degrees, which is the primary arc of motion used in overhead throwing, relies progressively on the static and dynamic soft tissue restraints to provide stability.
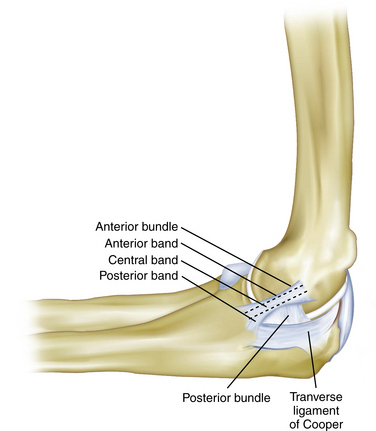
The MUCL is not a single ligament but is rather a complex consisting of an anterior bundle, a posterior bundle, and a transverse component (Fig. 13-1).9 The anterior bundle is the most well-defined structure, and it originates on the medial epicondyle and inserts on the sublime tubercle. The anterior bundle is subdivided into three components: an anterior band, a central band, and a posterior band. The anterior and posterior bands tighten in a reciprocal manner during flexion and extension, respectively. The posterior bundle is a less distinct fan-shaped structure. The transverse ligament is the least distinct anatomic structure and provides very little stability to the elbow because it does not cross the joint. Biomechanical studies have demonstrated that the anterior bundle is the primary constraint to valgus stress about the elbow.10–12 Further studies have shown that the anterior band of the anterior bundle provides most of the stability from 30 to 90 degrees of flexion, whereas the posterior bundle becomes functionally significant between 60 degrees and maximum flexion.13
The mechanics of overhead throwing, particularly pitching, account for the various pathologies seen in overhead athletes. Valgus forces have been estimated to reach 64 N during the late cocking and early acceleration phases of throwing.3,14 After the early and late cocking phases, the elbow goes from rapid flexion to extension, and the tangentially directed forces produce a valgus and extension moment, with resulting tensile forces across the medial side of the elbow, compressive forces across the lateral aspect of the joint, and shear forces in the posterior compartment.3,4,15 The repetitive stress on the MUCL eventually leads to attenuation and ultimately rupture, resulting in an insufficient ligament complex, abnormal valgus rotation of the elbow, and instability. The term valgus extension overload describes this phenomenon.2,16 As the athlete continues to throw with instability, the valgus overload is accentuated, and excessive valgus moments lead to stretch of other medial structures, resulting in ulnar neuritis, flexor-pronator tendinopathy, or medial epicondyle apophysitis in the skeletally immature patient.
Corresponding overload on the lateral side of the elbow may lead radiocapitellar chondromalacia, osteophyte formation, and loose bodies. During extension, posterior shear forces can produce olecranon osteophytes at the posteromedial tip with a corresponding kissing lesion on the posteromedial trochlea.3 The clinician who treats throwing athletes must be familiar with these pathologies and be alert for underlying MUCL insufficiency as the cause of many of these disorders, because treating the pathology without ligament reconstruction often fails to relieve the athletes’ symptoms and allow them to return to sport.
PATIENT EVALUATION
Physical Examination
Inspection of the elbow begins with an assessment of the resting position of the elbow and its carrying angle. A normal carrying angle is approximately 11 degrees of valgus for men and 13 degrees of valgus for women.3 An increase in the carrying angle of valgus may indicate an adaptation to the repetitive stress of valgus instability. Angles of greater than 15 degrees in professional pitchers have been documented in the literature.17 The lateral, posterior, medial, and anterior regions of the involved elbow should be examined for swelling, obvious deformity, scars, or signs of previous trauma.
In the posteromedial region of the elbow, the ulnar nerve is easily palpable in the groove, which is located between the medial epicondyle and the olecranon. The examiner should test for a Tinel sign and for hypermobility. This is done by palpating the nerve as the elbow is brought from extension to terminal flexion to determine whether the nerve subluxates or completely dislocates over the medial epicondyle. Palpation of the posteromedial region of the elbow should also focus on the olecranon, which can reveal osteophytes or swelling that occur in throwing athlete with valgus extension overload syndrome. The medial subcutaneous border of the olecranon should also be palpated for tenderness, which in the throwing athlete, can be caused by a stress fracture.18
Examination of the lateral region of the elbow begins with palpation of the lateral epicondyle. Tenderness directly over the epicondyle is consistent with lateral epicondylitis; tenderness directly over the anconeus soft spot can indicate a symptomatic lateral plica, a condition that is commonly found in throwing athletes. In one study, this was the most reproducible finding in a group of patients who were treated for this condition.19
Range of motion should be assessed for elbow flexion and extension and for forearm supination and pronation, as well as the nature of the extension and flexion end points. Cain and associates describe the “end feel” at the extremes of motion in the physical examination of the throwing athlete.3 Normal extension terminates in the firm sensation of the posterior bony articulation making contact in the olecranon fossa, and normal flexion terminates in the abutment of the soft tissues of the distal humerus and the proximal forearm. Variations in the normal end points, particularly a bony end feel in extension, can indicate pathology such as posterior osteophytes. The examiner should focus on the end feel at extension and not necessarily on motion itself. Elbow flexion contractures have been detected in up to 50% of professional pitchers, and they do not necessarily indicate injury.
To perform the valgus stress test, the patient’s distal forearm is placed under the examiner’s axilla as a valgus load is applied to the elbow in 30 degrees of flexion (Fig. 13-2). The absence of a distinct end point combined with pain or tenderness indicates a positive test result and insufficiency of the anterior band of the anterior bundle of the medial collateral ligament (MCL).
The moving valgus stress test, as described by O’Driscoll,20 is performed with the patient in an upright position and the shoulder abducted 90 degrees (Fig. 13-3). Starting with the elbow in full flexion and the shoulder in maximal external rotation, the elbow is quickly extended while a constant valgus torque is maintained. For an examination result to be positive, the pain generated by the maneuver must reproduce the medial elbow pain that the patient has with activities, and the pain should be maximal between the position of late cocking (120 degrees) and early acceleration (70 degrees) as the elbow is extended.
Other relevant tests of the throwing athlete include the radiocapitellar compression test for osteochondritis dissecans of the radiocapitellar joint, the clunk test for posterior olecranon impingement, and the flexion-pronation test to detect a symptomatic snapping lateral plica. The radiocapitellar compression test is performed by placing the elbow in full extension and loading the joint with supination and pronation to produce mechanical symptoms. The clunk test for posterior olecranon impingement stabilizes the upper arm and brings the elbow into extension to produce posterior elbow pain (Fig. 13-4). The flexion pronation test is performed by placing the arm in maximum pronation and then passively flexing the elbow to approximately 90 degrees, which causes snapping in a positive test.19
Diagnostic Imaging
The routine preoperative radiographic evaluation of the elbow includes anteroposterior, lateral, and oblique views. Stress views may be helpful in assessing ligamentous laxity, and olecranon axial views at 110 degrees of flexion may reveal posteromedial osteophytes in valgus extension overload syndrome. However, it has been our experience that a true lateral view of the elbow in hyperflexion is adequate to diagnose posteromedial osteophytes. Contralateral comparison imaging studies of the elbow are helpful when evaluating elbow joint laxity and when trying to distinguish true growth disturbances from variant ossification centers in the pediatric population. Computed tomography can be helpful when trying to assess suspected bony pathology, including stress fractures and avulsion fractures.
Magnetic resonance imaging (MRI) remains the gold standard for evaluating pathology of the soft tissues about the elbow, including ligamentous injury, tendinopathy, and lesions of the articular cartilage. The accuracy of MRI in the evaluation of subtle MCL injuries and the role of arthrography and contrast remain controversial. At our institution, we use a noncontrast MRI with specially designed sequences (Fig. 13-5). Potter and colleagues demonstrated a high sensitivity and specificity for MRI in detecting ligamentous, soft tissue, and cartilaginous injuries.21–23 This technique maintains the minimally invasive nature of the test and limits cost. A major additional advantage is excellent visualization of the articular cartilage in a highly specific and sensitive manner.24
TREATMENT
Indications and Contraindications
Arthroscopy is an important method used for the diagnosis and treatment of valgus extension overload, with careful consideration given to choosing the appropriate indications. When valgus overload injury results in disabling symptoms for the athlete, surgical reconstruction of the anterior band of the ulnar collateral ligament may be indicated. Further indications for elbow arthroscopy in the throwing athlete include removal of loose bodies, excision of olecranon osteophytes, synovectomy, capsular release, capsular contracture, débridement of impinging osteophytes, articular cartilage lesions addressed, and the assessment and treatment of osteochondritis dissecans of the capitellum.25–28
The primary contraindication to elbow arthroscopy is any change in the normal bony or soft tissue anatomy that precludes safe entry of the arthroscope into the elbow joint.29 We do not recommend performing arthroscopy when there has been a previous ulnar nerve transposition or when adequate distention of the joint cannot occur. Arthroscopy is contraindicated if there is soft tissue infection in the area of the portal sites.
The surgeon should have a comprehensive understanding of the surrounding anatomy and advanced technical experience of arthroscopic technique. Attention to detail is essential to prevent compromise of the surrounding neurovascular structures or damage to the delicate articular cartilage.30
Conservative Management
Athletes who fail conservative management are candidates for surgery. It is not uncommon for throwing athletes to have myriad pathologies that require arthroscopic treatment and open MCL reconstruction. In addition to our aforementioned criteria for arthroscopic management of valgus extension overload, we perform a MCL reconstruction concomitantly based on the following criteria: MRI evidence of MCL injury; a history of medial elbow pain in the region of the MCL that develops during the late cocking and early acceleration phase; and pain that is severe enough to prevent the athlete from an acceptable level of competition.
Arthroscopic Technique
Patient Positioning
The prone position, first described by Poehling and coworkers,31 places the patient prone on chest rolls with the arm stabilized by an arm holder and allowed to hang off the table. The shoulder is abducted to 90 degrees, and the elbow is flexed to 90 degrees. Some surgeons prefer this position because it eliminates the need for traction, places the elbow in a more stable position, and allows easier access to the posterior aspect of the joint.26,31 If necessary, this position allows conversion from arthroscopy to an open surgical procedure, but we have found this to be very difficult.31 Disadvantages of the prone position include general anesthesia and poor access to the airway by the anesthesiologist.
The lateral decubitus position, originally described by O’Driscoll and Morrey,32 has advantages similar to those of the prone position, including improved arm stability and posterior joint access. However, in the lateral decubitus position, the anesthesiologist’s access to the airway is not compromised. The main disadvantage is that access to the anterior compartment may require repositioning by placing the patient in a lateral position with the shoulder flexed forward at 90 degrees over a padded bolster.
The supine-suspended position, originally described by Andrews and Carson,25 positions the shoulder in 90 degrees of abduction, with the elbow flexed 90 degrees and the forearm, wrist, and hand suspended by a mechanical traction device. We prefer a modification of this position with the shoulder flexed 90 degrees such that the forearm and humerus are suspended over the patient’s chest for arthroscopic evaluation of the elbow. This position requires a mechanical arm holder, and it securely positions the arm in space and eliminates the need for an additional assistant. Several options are available, including the McConnell arm holder (McConnell Orthopaedic Manufacturing, Greenville, TX) and the Spider hydraulic arm holder (Spider Limb Positioner, Tenet Medical Engineering, Calgary, Alberta, Canada). We prefer the Spider hydraulic arm holder because it more rigidly suspends the arm in space and can be easily adjusted to allow for any desired changes in position (Fig. 13-6). This allows easy access to the anterior and posterior compartments, which facilitates arthroscopic work. With the forearm and humerus flexed over the chest, the anterior neurovascular structures effectively drop away from the anterior capsule, allowing for easier and safer work to be done on the anterior compartment.
We have found this technique to be very successful and have not experienced the disadvantages reported in the literature, such as arm instability, difficult orientation, and poor access to the posterior compartment.33 A tourniquet should be placed around the proximal aspect of the arm, but it should be inflated only when blood loss impairs arthroscopic visualization.
Portal Placement
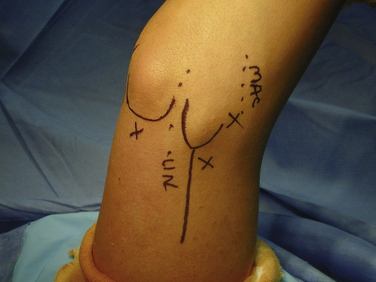
The most common portals used for elbow arthroscopy include the anterolateral, midlateral, anteromedial, proximal medial, proximal lateral, and straight posterior.29,34 We most commonly use the midlateral, proximal lateral, posterolateral, and trans-triceps portals (Figs. 13-7 to 13-9)
The midlateral portal, also known as the soft spot portal or direct lateral portal, is located in the center of the triangle formed by the lateral epicondyle, the tip of the olecranon, and the radial head. The anconeus is penetrated in this portal, and the nearest neurovascular structure is the posterior antebrachial cutaneous nerve.35 This portal is often used to inject fluid to distend the capsule, but it can also be used to remove loose bodies stuck in the lateral gutter.34
The proximal lateral portal, originally described by Field and colleagues36 and by Stothers and coworkers,37 is located 2 cm proximal to the epicondyle and lies directly on the anterior surface of the humerus. The capsular attachments are such that, in flexion, the radial nerve is carried away from the nerve when the joint is distended. This enables clear visualization of the medial and lateral sides of the joint, the anterior and lateral aspects of the radial head and capitellum, and the lateral gutter.38
The posterolateral portal is located 3 cm proximal to the tip of the olecranon and immediately lateral to the triceps tendon. The nearest neurovascular structures are the posterior brachial cutaneous and posterior antebrachial cutaneous nerves.29 This portal provides unobstructed visualization of the entire posterior compartment.34
The trans-triceps portal is a straight posterior portal located in the midline and 3 cm proximal to the tip of the olecranon. It is mostly used to débride the posteromedial olecranon of osteophytes and the olecranon fossa of chondral lesions and for the removal of loose bodies.34
Operative Technique
Anterior Arthroscopy.
The arthroscope is introduced through the proximal lateral portal into the anterior compartment (Fig. 13-10). Diagnostic arthroscopy is then performed anteriorly to evaluate the articular cartilage and synovium and to look for loose bodies. The coronoid process is examined for the presence of bone spurs, and the anterior trochlea and coronoid fossa are examined for cartilage lesions. The anterior radiocapitellar joint is evaluated for osteochondral lesions of the capitellum and any matching pathology of the radial head. The radial nerve lies on or within a few millimeters of the anterolateral joint capsule. Débridement in this area therefore requires considerable caution. The anterior capsule is then evaluated for thickening or contracture in the context of a loss of passive extension.
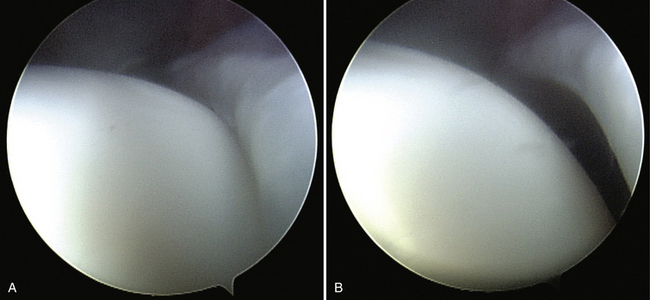
To confirm the diagnosis of MCL insufficiency, the arthroscopic valgus stress test is performed during assessment of the anterior compartment. With the arthroscope in the proximal lateral portal visualizing the medial compartment, valgus stress is applied manually to the elbow. A gap between the ulna and humerus of more than 3 mm is consistent with ulnar collateral ligament insufficiency (Fig. 13-11). A probe of known dimensions can be inserted through the proximal medial portal to aid in the measurement of the ulnohumeral opening. If the portal is not necessary, a valgus opening can be visualized and appropriately estimated. If work needs to be performed in the anterior compartment, such as débridement, synovectomy, capsular release, or removal of loose bodies, a proximal medial portal is established under direct visualization.
Posterior Arthroscopy.
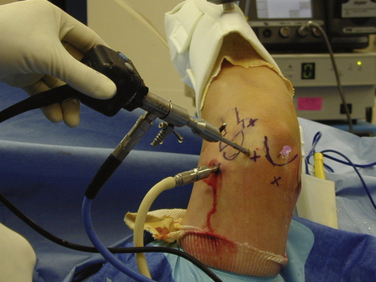
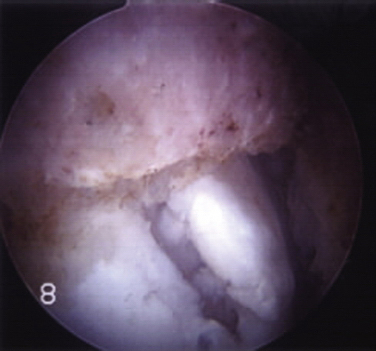
After completion of the anterior arthroscopy, the cannula and its camera are retained, with fluid inflow attached to maintain distention of the joint (Fig. 13-12). A posterolateral portal is then established, and the camera is removed from the anterior cannula and inserted through this portal. We typically maintain the anterior cannula to facilitate reentry into the anterior compartment if necessary and to ultimately drain the elbow of fluid at the conclusion of the procedure.
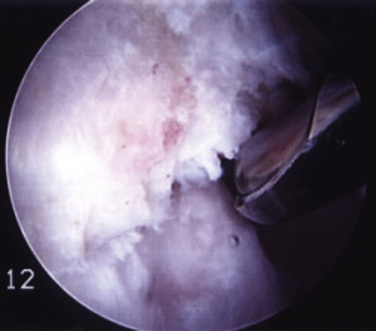
If work needs to be performed posteriorly, a trans-triceps portal is established (Fig. 13-13). The medial, lateral, and central aspects of the olecranon are then evaluated for the presence of osteophytes. The corresponding olecranon fossa and posteromedial aspect of the humeral condyle are evaluated for matching chondral defects. The posterior radiocapitellar joint is evaluated by advancing the arthroscope down the lateral gutter. One of the most common errors made in elbow arthroscopy is to miss a loose body that is caught in the posterior radiocapitellar joint.39 An accessory midlateral portal through the soft spot often is necessary for removal of the loose body.38
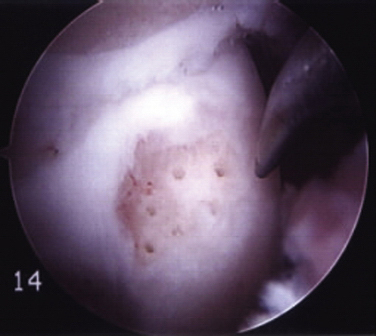
In the throwing athlete, the most common problem encountered is a fragmented spur on the posteromedial olecranon as a result of posterior shear stresses seen in valgus extension overload (Fig. 13-14).38 These spurs should be anticipated because they can be seen on the preoperative radiographs and MRI scans. With the camera in the posterolateral portal and the shaver in the trans-triceps portal, the extent and dimensions of the osteophyte can be evaluated. Excess soft tissues, including synovial reflections, are removed from the olecranon tip by carefully using a radiofrequency device.38 The osteophyte is removed from the posteromedial olecranon using a gentle medial-to-lateral movement (Fig. 13-15).
The optimal amount of olecranon to be débrided has been a matter of debate. Common surgical practice involves débridement of the osteophyte along with some amount of native olecranon bone. Biomechanical studies have demonstrated that excessive olecranon resection can lead to elbow instability and MCL strain in the throwing athlete.40,41 Resections should be limited to approximately 3 mm, because resections greater than this may jeopardize the native or the reconstructed MCL. Practically speaking, our goal of arthroscopic débridement is to remove the osteophyte only and preserve as much native bone as possible.
After the osteophyte is removed, the humeral chondral surface can be visualized more completely and the kissing lesion of chondral abrasion opposite the osteophyte will be in direct view. Loose chondral flaps are débrided, and if necessary, microfracture is performed (Fig. 13-16). On completion of the posterior arthroscopy, the portals are briefly irrigated and closed with interrupted nylon sutures.
Open Medial Ulnar Collateral Ligament Reconstruction.
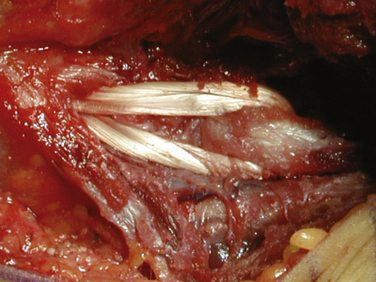
After the arm is exsanguinated to the level of the tourniquet, an 8- to 10-cm incision is made starting 2-cm proximal to the medial epicondyle in line with the intermuscular septum. The incision is carried distally, approximately 2 cm beyond the sublime tubercle. When exposing the flexor-pronator mass, the median antebrachial cutaneous nerve is often observed and should be identified and protected. A muscle-splitting approach is used through the posterior one third of the common flexor-pronator mass within the most anterior fibers of the flexor carpi ulnaris muscle. This is located at the raphe between the flexor carpi ulnaris muscle and the anterior portion of the flexor bundle. The advantage of this particular approach is that it uses a true internervous plane.42 The anterior bundle of the MCL is excised to expose the joint.
Final tensioning is performed by taking the elbow through a complete range of motion while a varus stress is applied. After the surgeon is satisfied, the two suture ends are tied over the medial epicondyle with the elbow in approximately 20 degrees of flexion and full supination (Fig. 13-17). This position is chosen because it reduces excessive tension or laxity in either of the two limbs. After the tourniquet is deflated and hemostasis achieved, an ulnar nerve transposition is performed if indicated. Otherwise, the fascia over the flexor-pronator mass is reapproximated, and the remaining wound is closed in layers. The elbow is placed in a plaster splint at 45 degrees of flexion to reduce excessive laxity or tension on either limb and forearm supination to keep the joint reduced.
PEARLS& PITFALLS
PEARLS
PITFALLS
Postoperative Rehabilitation
Postoperatively, we prefer a compressive dressing for 48 hours, cryotherapy, and routine wound care. Sling immobilization is minimal and used for comfort only. We then proceed in a triphasic rehabilitation program that focuses on the restoration of joint range of motion and flexibility within the healing parameters of the structures involved in the surgery (Box 13-1). Rehabilitation progresses through each phase only after the major goals of the previous phase have been successfully achieved. We recommend the athlete achieve the following criteria to safely return to play: painless and full range of motion, no elbow pain or tenderness, satisfactory isokinetic muscular strength testing, and a satisfactory clinical examination. Rehabilitation after elbow arthroscopy can be somewhat aggressive because the procedure causes minimal postoperative morbidity. For a more comprehensive review of nonoperative and postoperative rehabilitation of the athlete’s elbow, we recommend the chapter by Wilk and Levinson in The Athlete’s Elbow.43 The authors outline the three-phase approach to rehabilitation in detail and explain how such a program allows the surgeon and therapist to tailor the program to the individual patient’s needs.
Box 13-1 Postoperative Rehabilitation Program
PHASE II: 6 TO 10 WEEKS
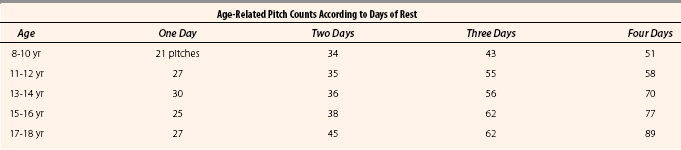
Table 13-1 presents an interval throwing program. Age-related pitch counts according to days rest are listed in Table 13-2.
CONCLUSIONS
Elbow arthroscopy is a powerful tool in the diagnosis and treatment of the various pathologies seen in the throwing athlete’s elbow. Preoperative evaluation should consist of a complete history and physical examination and the use of appropriate imaging modalities to make a prompt diagnosis and facilitate a rapid return to play for the athlete. The arthroscopic recognition and treatment of related pathology correlates with appropriate surgical technique, particularly proper portal placement and adequate surgical instrumentation. The clinician who wishes to use arthroscopy as a tool for treating the thrower’s elbow must be proficient in basic arthroscopic techniques, coupled with a thorough understanding of elbow anatomy and biomechanics.
1. O’Holleran JD, Altchek DW. Elbow arthroscopy: treatment of the thrower’s elbow. Instr Course Lect.. 2006;55:95-107.
2. Chen A, Youm T, Ong B, et al. Imaging of the elbow in the overhead throwing athlete. Am J Sports Med. 2003;31:466-473.
3. Cain E, Dugas J, Wolf R, Andrews J. Elbow injuries in throwing athletes: a current concepts review. Am J Sports Med. 2003;31:621-635.
4. Schickendantz M. Diagnosis and treatment of elbow disorders in the overhead athlete. Hand Clin. 2002;18:65-75.
5. Ball C, Galatz L, Yamaguchi K. Elbow instability: treatment strategies and emerging concepts. Instr Course Lect. 2002;51:53-61.
6. Rizio L, Uribe J. Overuse injuries of the upper extremity in baseball. Clin Sports Med. 2001;20:453-468.
7. Miller C, Savoie FIII. Valgus extension injuries of the elbow in the throwing athlete. J Am Acad Orthop Surg. 1994;2:261-269.
8. Chen F, Rokito A, Jobe F. Medial elbow problems in the overhead throwing athlete. J Am Acad Orthop Surg. 2001;9:99-113.
9. Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315-319.
10. Callaway GH, Field LD, Deng XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223-1231.
11. Hotchkiss RN, Weiland AJ. Valgus stability of the elbow. J Orthop Res. 1987;5:372-377.
12. Hechtman KS, Tjin-A-Tsoi EW, Zvijac JE, et al. Biomechanics of a less invasive procedure for reconstruction of the ulnar collateral ligament of the elbow. Am J Sports Med. 1998;26:620-624.
13. Regan WD, Korinek SL, Morrey BF, et al. Biomechanical study of ligaments around the elbow joint. Clin Orthop. 1991;271:170-179.
14. Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury of mechanisms. Am J Sports Med. 1995;23:233-239.
15. Pappas A, Zawacki R, Sullivan T. Biomechanics of baseball pitching: a preliminary report. Am J Sports Med. 1985;13:216-222.
16. Wilson FD, Andrews JR, Blackburn TA, et al. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11:83-88.
17. King JW, Brelsford HJ, Tullos HS. Analysis of the pitching arm of the professional baseball pitcher. Clin Orthop. 1969;67:116-123.
18. Schickendantz MS, Ho CP, Koh J. Stress injury of the proximal ulna in professional baseball players. Am J Sports Med. 2002;30:737-741.
19. Antuna SA, O’Driscol SW. Snapping plicae associated with radiocapitellar chondromalacia. Arthroscopy. 2001;17:491-495.
20. O’Driscoll SW, Lawton RL, Smith AM. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med. 2005;33:231-239.
21. Potter HG. Imaging of posttraumatic and soft tissue dysfunction of the elbow. Clin Orthop. 2000;370:9-18.
22. Gaary EA, Potter HG, Altchek DW. Medial elbow pain in the throwing athlete: MR imaging evaluation. AJR Am J Roentgenol. 1997;168:795-800.
23. Potter HG, Ho ST, Altchek DW. Magnetic resonance imaging of the elbow. Semin Musculoskelet Radiol. 2004;8:5-16.
24. Potter HG, Linklater JM, Allen AA, et al. Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276-1284.
25. Andrews JR, Carson WG. Arthroscopy of the elbow. Arthroscopy. 1985;1:97-107.
26. Baker CL. The elbow. In: Whipple TL, ed. Arthroscopic Surgery: The Shoulder and Elbow. Philadelphia, PA: JB Lippincott; 1993:239-300.
27. Yadao MA, Field LD, Savoie FHIII. Osteochondritis dissecans of the elbow. Instr Course Lect. 2004;53:599-606.
28. Takahara M, Shundo M, Kondo M, et al. Early detection of osteochondritis dissecans of the capitellum in young baseball players: report of three cases. J Bone Joint Surg Am. 1998;80:892-897.
29. Walcott GD, Savoie FH, Field LD. Arthroscopy of the elbow: setup, portals and diagnostic technique. In: Altchek DW, Andrews JR, eds. The Athlete’s Elbow. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:209-217-249-273.
30. Andrews JR, St Pierre RK, Carson WGJr. Arthroscopy of the elbow. Clin Sports Med. 1986;5:653-662.
31. Poehling GG, Whipple TL, Sisco L, Goldman B. Elbow arthroscopy: a new technique. Arthroscopy. 1989;5:222-224.
32. O’Driscoll SW, Morrey, BF. Arthroscopy of the elbow: diagnostic and therapeutic benefits and hazards. J Bone Joint Surg Am. 1992;74:84-94.
33. Abboud JA, Ricchetti ET, Tjoumakaris F, Ramsey ML. Elbow arthroscopy: basic setup and portal placement. J Am Acad Orthop Surg. 2006;14:312-318.
34. Dodson CC, Nho SJ, Williams RJIII, Altchek DW. Elbow arthroscopy. J Am Acad Orthop Surg. 2008;16:574-585.
35. Adolfsson L. Arthroscopy of the elbow joint: a cadaveric study of portal placement. J Shoulder Elbow Surg. 1994;3:53-61.
36. Field LD, Altchek DW, Warren RF. Arthroscopic anatomy of the lateral elbow: a comparison of three portals. Arthroscopy. 1994;10:602-607.
37. Stothers K, Day BD, Regan WR. Arthroscopy of the elbow: anatomy, portal sites and a description of the proximal lateral portal. Arthroscopy. 1995;11:449-457.
38. O’Holleran JD, Altchek DW. Throwers elbow: arthroscopic treatment of valgus extension overload syndrome. HSS J. 2006;2:83-93.
39. Altchek DW, Hyman J, Williams R, et al. Management of MCL injuries of the elbow in throwers. Tech Shoulder Elbow Surg. 2000;1:73-81.
40. Kamineni S, Hirahara H, Pomianowski S, et al. Partial posteromedial olecranon resection: a kinematic study. J Bone Joint Surg Am. 2005;85A:1005-1011.
41. Kamineni S, ElAttrache NS, O’Driscoll SW, et al. Medial collateral ligament strain with partial posteromedial olecranon resection: a biomechanical study. J Bone Joint Surg Am. 2004;86A:2424-2430.
42. Smith GR, Altchek DW, Pagnani MJ, et al. A muscle-splitting approach to the ulnar collateral ligament of the elbow: neuroanatomy and operative technique. Am J Sports Med. 1996;24:575-580.
43. Wilk KE, Levinson M. Rehabilitation of the athlete’s elbow. In: Altchek DW, Andrews JR, editors. The Athlete’s Elbow. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:249-273.