CHAPTER 3 Arthroscopically Assisted Ulnar Shortening
Basic Science and Anatomy
Ulnocarpal Joint Anatomy
The base of the triangular fibrocartilage attaches to the distal radius at the distal edge of the sigmoid notch. Its distal surface blends imperceptibly with the hyalin cartilage of the lunate fossa of the distal radius. The triangular fibrocartilage narrows as it passes from radial to ulnar to insert in the fovea at the base of the ulnar styloid. Dorsally and palmarly, the TFCC thickens to form the distal radioulnar ligaments. The integrity of these two ligaments is critical to the stability of the distal radioulnar joint. The triangular fibrocartilage meniscal homologue passes distally to attach at the ulnar aspect of the triquetrum. The interval between the ulnotriquetral ligament and the meniscal homologue and ulnar collateral ligament is known as the pre-styloid recess (or the pisotriquetral recess).1
Biomechanics
Palmer and others have demonstrated an inverse relationship between the thickness of the triangular fibrocartilage and ulnar variance.2 That is, the more positive the ulnar variance the thinner the triangular fibrocartilage. This relationship explains the observed coincidence of ulnar plus variance and TFCC tears (ulnar abutment syndrome). The ulnar abutment syndrome is characterized by an ulnar plus variance, central tears of the triangular fibrocartilage, and chondromalacia of the adjacent articular surfaces of the lunate, triquetrum, and ulnar head.
Werner et al.3 have studied the effect of ulnar length on load transmission across the triangular fibrocartilage. They demonstrated a direct relationship between the length of the ulna and the amount of force transmitted across the TFCC. As the ulna gets longer, the force transmitted across the TFCC increases. The opposite occurs with ulnar shortening.
The vascular supply of the triangular fibrocartilage is characterized by a peripheral vascular zone and a central avascular zone.4 The lack of central blood supply precludes any healing of central TFCC tears and dictates the choice of debridement as the treatment for such tears.
Contraindications
Arthroscopic ulnar shortening is unlikely to help those patients who present with an ulnar abutment syndrome combined with additional ulnocarpal and/or lunatotriquetral pathology. A lunatotriquetral ligament instability or ulnocarpal ligament laxity in the presence of an ulnar abutment syndrome will not respond to an arthroscopic ulnar shortening because the arthroscopic ulnar shortening does not address the LT or ulnocarpal instability. An ulnar shortening osteotomy combined with an arthroscopic TFCC debridement would be a reasonable approach in this case. The LT and ulnocarpal instability cannot be treated with ulnocarpal capsular shrinkage because the capsular shrinkage demands immobilization for six to eight weeks. The postoperative regimen for an arthroscopically assisted ulnar shortening consists of early range of motion of the wrist and distal radioulnar joint.
Technique
The initial approach to the TFCC and distal ulna is through the 3-4 and 4-5 portals or through the 6-R portal. The arthroscope is placed in the 3-4 portal, whereas the 4-5 or 6-R portals are used as instrument portals. The arthroscopic treatment of the ulnar abutment syndrome is facilitated by using the Holmium:YAG laser.5 Hyaline cartilage is very efficiently removed with the laser at higher energy settings (2.0 joules at 20 pulses per second). Not only is the ulnar head hyalin cartilage and subchondral bone rapidly removed but in contrast to burring is removed without producing much debris.
An effort is made to leave a smooth surface on the remaining distal ulna. The trabeculae of the distal ulna always produce a somewhat rough distal ulnar surface at the completion of the procedure. However, these irregularities disappear during the months following the surgery (Figures 3.1 and 3.2). Large irregularities must be avoided because they can catch on the proximal surface of the residual TFCC during supination and pronation. Once the ulnar shortening is complete, the traction should be removed from the wrist and the wrist should be ulnarly deviated, axially loaded, and taken through a full range of supination and pronation. If this maneuver produces no popping and clicking or catching, the ulnar head surface is probably smooth.
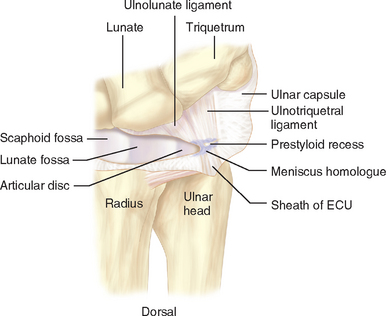
FIGURE 3.1 Anatomy of the triangular fibrocartilage.
(Redrawn from Ishii S, Palmer AK, Werner FW, Short WH, Fortino MD. An anatomic study of the ligamentous structure of the triangular fibrocartilage complex. J Hand Surg [Am] 1998; 23:977–85.)
The postoperative regimen after ulnar shortening includes providing the patient with a wrist splint to be worn as needed, as well as a home therapy program consisting of active and passive range-of-motion exercises. Early range-of-motion exercises are essential. Immobilization of the wrist leads to a loss of motion due to postoperative scar contracture. The sutures (wounds are closed using subcuticular sutures of 4–0 Prolene) are removed at two weeks. Strengthening exercises can be started at six weeks if needed. Premature resumption of heavy lifting or repetitive activities will lead to radiocarpal synovitis. The recovery after an ulnar shortening can be as long as six months (as suggested by Feldon).6 However, the majority of patients will be improved long before six months.
Results
Arthroscopically assisted ulnar shortening has proven to be an effective method of treating patients with an ulnar abutment syndrome.7,8 Eighty-one percent of our patients had an excellent or good outcome. Eight of Tomaino’s 12 patients were pain free, and 4 had minimal symptoms.
This technique has been shown to be as effective as formal ulnar shortening osteotomy for the treatment of ulnar abutment syndrome.9 Arthroscopically assisted ulnar shortening has the advantage of being less invasive and is not associated with complications associated with plate fixation of an osteotomy, such as nonunion and the need for subsequent plate removal (56%).
1 Ishii S, Palmer AK, Werner FW, Short WH, Fortino MD. An anatomic study of the ligamentous structure of the triangular fibrocartilage complex. J Hand Surg [Am]. 1998;23:977-985.
2 Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and triangular fibrocartilage complex thickness. J Hand Surg [Am]. 1984;9:681-682.
3 Werner FW, Glisson RR, Murphy DJ, Palmer AK. Force transmission through the distal radioulnar carpal joint: Effect of ulnar lengthening and shortening. Handchir Mikrochir Plast Chir. 1986;18:304-308.
4 Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: Its clinical significance. J Hand Surg [Am]. 1991;16(6):1101-1105.
5 Nagle DJ, Bernstein MA. Laser-assisted arthroscopic ulnar shortening. Arthroscopy. 2002;18(9):1046-1051.
6 Feldon P, Terrono AL, Belsky MR. The “wafer” procedure: Partial distal ulnar resection. Clin Orthop. 1992;275:124-129.
7 Nagle DJ, Bernstein MA. Laser assisted arthroscopic ulnar shortening. Arthroscopy. 2002;18(9):1046-1051.
8 Tomaino MM, Weiser RW. Combined arthroscopic TFCC debridement and wafer resection of the distal ulna in wrists with triangular fibrocartilage complex tears and positive ulnar variance. J Hand Surg [Am]. 2001;26(6):1047-1052.
9 Bernstein MA, Nagle DJ, Martinez A, Stogin JMJr., Wiedrich TA. A comparison of combined arthroscopic triangular fibrocartilage complex debridement and arthroscopic wafer distal ulna resection versus arthroscopic triangular fibrocartilage complex debridement and ulnar shortening osteotomy for ulnocarpal abutment syndrome. Arthroscopy. 2004;20(4):392-401.