CHAPTER 22 Arthroscopic Treatment of Volar Carpal Ganglion Cysts
“Other things may change us, but we start and end with family”
To Nancy, Ryann, and Sawyer, who support and put up with me, constantly.
Arthroscopic Resection of Volar Carpal Ganglia
The concept of using arthroscopy as a means for the management of intra-articular conditions of the wrist has evolved tremendously since Roth first described the technique.1 Arthroscopy of the wrist has become an essential adjunctive tool not only for the diagnosis of multiple conditions but for their definitive treatment. Intra-articular lesions, including capsular lesions, can be assessed and treated arthroscopically.
In 1995, Osterman and Raphael presented a technique for the treatment of the dorsal carpal ganglion.2 This cystic structure has a predictable origin from the dorsal distal third of the scapholunate ligament. The initial skepticism regarding treatment of this lesion (which is at the anatomical boundary for visualization with the arthroscope) has been quelled by experience and refinement of the technique. Arthroscopic treatment of dorsal ganglion cysts is now routine for the experienced arthroscopist.3–5
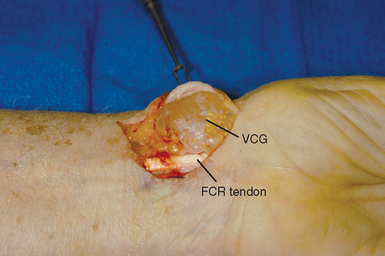
Volar ganglia occur less frequently than the more common dorsal carpal ganglion cyst, accounting for approximately 20% of wrist ganglia. They are sac-like structures (with no true cellular lining) filled with a thick viscous fluid consisting of glucosamine, albumen, globulin, and hyaluronic acid. The ganglion frequently presents externally as a mass in the interval between the flexor carpi radialis (FCR) tendon and radial artery, proximal to the wrist flexion crease (Figure 22.1). Usually, the ganglion presents as a visible and palpable mass—with symptoms that may include pain, numbness secondary to irritation of the palmar cutaneous branch of the median nerve (PcuBrMN), and cosmetic dissatisfaction.
Occult volar ganglia may also contribute to volar wrist pain without a visible or definitely palpable mass. These occult ganglia may be symptomatic due to capsular injury, inflammatory changes, or local pressure. The cause of ganglion cysts has been debated and has been attributed to synovial herniation, mucoid degeneration, degenerative arthritis, and stretch associated with trauma.6,7
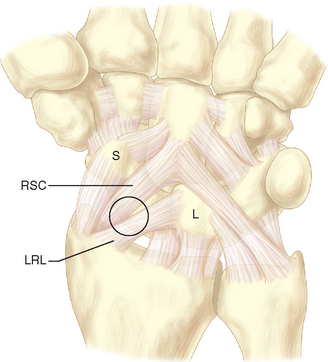
The anatomical origin of the volar carpal ganglion (VCG) has not been as well defined as its dorsal counterpart. Current literature supports a radioscaphoid or scaphotrapezial joint origin.7,8 They may occasionally originate from the FCR tendon or from aberrant locations.6,9 When the ganglion originates from the radioscaphoid joint, it arises from the volar capsule in the relatively deficient area between the volar radioscaphocapitate (RSC) and long radiolunate (LRL) ligaments (Figure 22.2).10
Traditionally, these ganglions are excised through an open volar approach, developing the interval between the radial artery and FCR tendon. The ganglion is then excised along with a segment of volar capsule. Arthroscopic excision of volar ganglion cysts eliminates the need for extensive dissection, limits capsular damage, allows identification of associated intra-articular pathology, and facilitates recovery and return to activity. Arthroscopic treatment of these cysts is technically feasible and facile.10 The volar capsular origin of these lesions is easily visualized, which allows excision of the ganglion stalk utilizing standard arthroscopic portals and instrumentation.
Technique
A standard arthroscopic technique and setup are utilized. Traction is essential, as with all wrist arthroscopy. The portals are marked after the traction is applied. The joint is insufflated with saline via the 3-4 portal. The author has found it very useful, especially in the case of the occult VCG, to watch where the fluid accumulates as the wrist is insufflated. Frequently, an occult ganglion sac will develop an out-pouching that can be seen on the volar aspect of the wrist as the joint is injected.
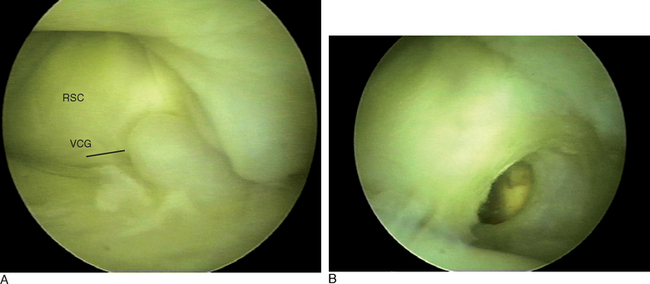
The arthroscopic evaluation of the wrist begins with the arthroscope in the 3-4 portal, with instruments passed via the 4-5 portal. In the case of a VCG, significant redundancy of the capsule or an out-pouching can be visualized in the extrinsic ligament interval between RSC and LRL. This out-pouching and capsular redundancy can be exaggerated, and visualization can be facilitated by placing pressure on the wrist capsule from the volar side. In occult cases, the ganglion will usually become visible (Figure 22.3).
Once the lesion is identified and routine wrist arthroscopy is completed, attention is turned to resection of the mass. A high-speed full-radius resector is used to debride the lesion and resect the volar capsule between the two extrinsic ligaments. Frequently, during the capsular resection thick ganglion fluid will be encountered coincident with clinical resolution of the volar mass. In cases of very large ganglions, a blunt obturator can be passed from dorsal to volar through the capsular defect to facilitate intra-articular aspiration and mobilization of ganglion cyst fluid. Care should be taken to avoid plunging the resector too deeply (to avoid injury to volar neurovascular and tendinous structures). A volar portal11 can be used with a cannula sheath to complete the debridement.
1 Roth JH, Poehling GG, Whipple TL. Hand instrumentation for small joint arthroscopy. Arthroscopy. 1988;4:126-128.
2 Osterman AL, Raphael J. Arthroscopic resection of dorsal ganglia of the wrist. Hand Clinics. 1995;11(1):7-12.
3 Gupta R, Bozentka DJ, Osterman AL. Wrist arthroscopy: Principles and clinical applications. J Am Acad Orth Surg. 2001;9:200-209.
4 Osterman AL. Wrist arthroscopy: Operative procedures. In: Green DP, Hotchkis RN, Pederson WC, editors. Green’s Operative Hand Surgery. Fourth Edition. New York: Churchill Livingstone; 1999:207-222.
5 Rizzo M, Berger RA, Steinmann SP, Bishop AT. Arthroscopic resection in the management of dorsal wrist ganglions: Results with a minimum 2-year follow-up period. J Hand Surg. 2004;29A:59-62.
6 Nahra ME, Bucchieri JA. Ganglion cysts and other tumor related conditions of the hand and wrist. Hand Clinics. 2004;20(3):249-260.
7 Wright TW, Cooney WP, Ilstrup DM. Anterior wrist ganglia. J Hand Surg. 1994;19A:954-958.
8 Greendyke SD, Wilson M, Shepler TR. Anterior wrist ganglia from the scaphotrapezial joint. J Hand Surg. 1992;17A:487-490.
9 Shapiro PS, Seitz WH. Non-neoplastic tumors of the hand and upper extremity. Hand Clinics. 1995;11(2):133-160.
10 Ho PC, Lo WN, Hung LK. Arthroscopic resection of volar ganglion of the wrist: a new technique. J Arthroscopic and Related Surgery. 2003;19(2):218-221.
11 Abe Y, Doi K, Hattori Y, Ikeda K, Dhawan V. Arthroscopic assessment of the volar region of the scapholunate interosseous ligament through a volar portal. J Hand Surg. 2003;28(1):69-73.