CHAPTER 2 Arthroscopic Treatment of Tibial Eminence Fractures
Tibial eminence fractures are intra-articular fractures that can be a challenging injury for orthopedic surgeons to manage. These represent an avulsion injury of the insertion of the anterior cruciate ligament (ACL) at the tibia and are considered the equivalent of an ACL tear.1,2 Poncet first described the tibial eminence fracture in 1875 and, since then, the treatment algorithm has changed significantly, from nonoperative management to what is now considered contemporary arthroscopic management.3 This chapter will discuss in detail a current review of the anatomy, mechanism of injury, diagnosis, treatment, rehabilitation, and potential complications that can occur with tibial eminence fractures.
ANATOMY
The tibia is the primary weight-bearing bone of the knee joint. The most proximal aspect of the tibia is comprised of the medial and lateral tibial condyles. The articular surfaces of the condyles are the medial and lateral tibial plateaus, which articulate with the corresponding medial and lateral femoral condyles. The plateaus are separated by the intercondylar eminence, which serves as the site of attachment for the anterior and posterior cruciate ligaments and the fibrocartilaginous menisci.4 Specifically, the midpoint of the intercondylar eminence serves as the distal attachment of the ACL.
Tibial eminence fractures are seen in children usually between the ages of 8 and 15 years.3,5,6 Although this fracture pattern is commonly associated with a childhood injury, it is also seen in adults.2,7,8 It is theorized that this occurs more commonly in children because of the relative weakness of the incompletely ossified tibial eminence as compared with the fibers of the ACL. It has also been proposed that the injury occurs secondary to greater elasticity of the ligaments in younger people.9
PATIENT EVALUATION
Diagnostic Imaging
Plain radiographs are usually diagnostic and involve anteroposterior, lateral, and oblique views. Computed tomography (CT) scanning may be used to define bony architecture better and magnetic resonance imaging (MRI) is useful for determining additional injuries to chondral surfaces, menisci, and ligaments. Arteriography and vascular surgery consultation must be considered in the presence of diminished pulses or abnormal vascular examination. We prefer to obtain an MRI in all pattients in whom tibial avulsion is suspected to confirm the diagnosis and determine the amount of displacement and presence of associated pathology.
Classification
Meyers and McKeever first described the classification scheme for tibial eminence fractures in 1959.2 Their classification divides these fractures into three types based on displacement of the avulsed fracture fragment (Fig. 2-1). Type I represents a nondisplaced or minimally displaced fracture at the anterior margin. Type II fractures involve the anterior third or half of the avulsed bone displaced proximally, with an intact posterior hinge resembling a bird’s beak. Type III fractures have a completely displaced fracture. These have been further subdivided into IIIA and IIIB fracture classifications.10 Type IIIA fractures involve the ACL insertion only, whereas the IIIB type includes the entire intercondylar eminence. Some have labeled comminuted fractures as type IV.10
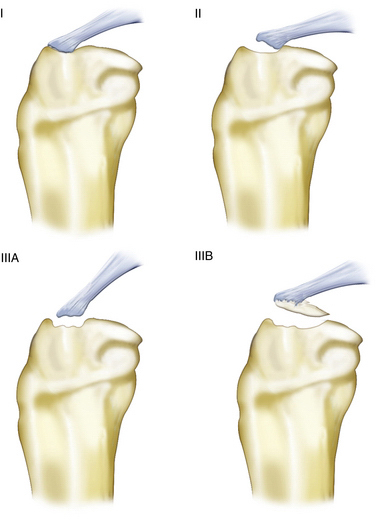
FIGURE 2-1 Meyers and McKeever classification of tibial intercondylar eminence fractures.
(Adapted from Lubowitz JH, Elson WS, Guttman D. Part II: Arthroscopic treatment of tibial plateau fractures: intercondylar eminence avulsion fractures. Arthroscopy. 2005;21:86-92.)
Associated injuries with fractures of the tibial eminence are common. Meniscus injuries are the most common injuries seen; however, these fractures may be associated with chondral and ligamentous injuries as well.11,12 In an unpublished study, we found an interposed intermeniscal ligament in 80% of types II and III injuries. This has profound implications for treatment strategies. In addition, tibial eminence fractures are also seen with tibial plateau fractures, specifically Schatzker types V and VI fractures.13
TREATMENT
The goal for management of tibial eminence fractures should be no different than for any other intra-articular fracture. Anatomic reduction and rigid fixation that allow for early range of motion should be the treatment for these fractures. Debate has ensued over anatomic reduction versus overreduction. It has been proposed that overreduction may result in excessive tension of the ACL, which results in limited knee range of motion.14 Others have countered this by stating that plastic deformation of the ACL occurs prior to the avulsion fracture and thus overreduction would result in a better outcome.9 Numerous studies have documented residual laxity in well-reduced tibial eminence fractures, and most have concluded that the laxity is not symptomatic.15–17 More studies are needed to answer the question of anatomic versus overreduction, but there is consensus that any displacement requires at least an anatomic reduction.
Management has been based on the Meyers and McKeever classification, with recommendations for immobilization in extension for type I fractures. Some controversy exists in regard to what degree the knee is to be extended for nonoperative management. Meyers and McKeever have recommended immobilization in 20 degrees of flexion.2,8 Similarly, Beaty and Kumar have recommended immobilization in 10 to 15 degrees of flexion.18 Fyfe and Jackson based their recommendations of flexing the knee to 30 to 40 degrees because the ACL is taut in extension and, with some flexion, the tension on the avulsion fragment would be less.19 These authors favor immobilization in full extension to avoid a flexion contracture, which can occur if the knee is kept in a flexed position. We encourage straight leg raises and quadriceps isometrics and allow full weight bearing, as tolerated, in a brace locked in full extension. The knee should not be immobilized in hyperextension because extensive stretch on the popliteal artery may result in a compartment syndrome.13 Regardless of the position of immobilization, close follow-up with radiographs weekly for 4 weeks should help confirm maintenance of reduction.
Treatment of type II fractures has been controversial. Closed reduction may be attempted by aspiration of the hemarthrosis and knee extension performed to allow the femoral condyles to help reduce the fracture.20 Anteroposterior and lateral radiographs should be taken to verify reduction and, with difficult visualization, CT or MRI should be performed. Often, anatomic reduction is not achieved secondary to interposition of the medial meniscus, lateral meniscus, or intermeniscal ligament. Persistent displacement, despite attempted reduction maneuvers, warrants arthroscopic evaluation and treatment. Many reports have identifed associated soft tissue injuries, including chondral, meniscal, and ligamentous structures. The need for anatomic reduction of these fractures to allow for postoperative stability and motion, combined with the need to identify and treat these associated injuries, make arthroscopic evaluation necessary for successful treatment of most type II and all type III fractures.16,21–24 These authors also think that most, if not all, type II fractures were likely a type III level of displacement at the time of disruption. Based on that, we take an aggressive operative approach to most type II injuries.
Closed reduction may be attempted for type III injuries, but anatomic reduction and maintenance of reduction are difficult. Most experts agree that type III fractures require reduction and fixation.13,25,26 Arthroscopic reduction and fixation of these injuries have become the standard of care and has made open reduction and internal fixation a treatment that is infrequently necessary or used.
Arthroscopic Technique
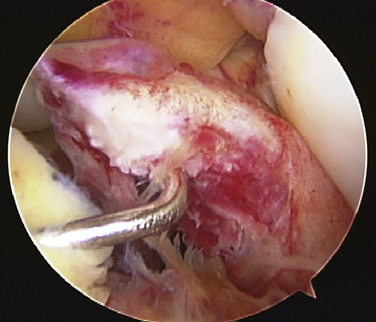
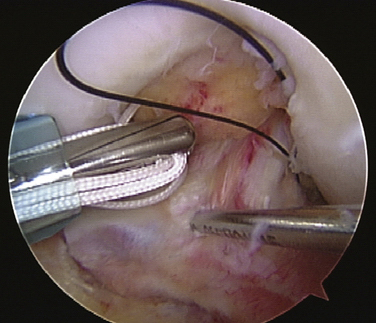
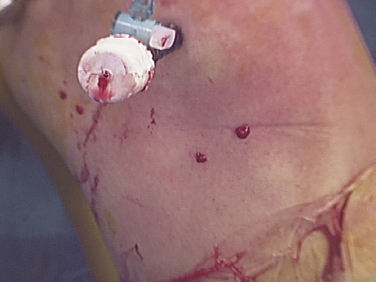
General or epidural anesthesia may be used. The leg is secured in an arthroscopic leg holder and the foot of the bed is flexed. The contralateral leg is supported with a foam pad and abducted to the side to allow fluoroscopy of the involved extremity in both anteroposterior and lateral projections. A tourniquet is placed around the thigh, but is not routinely used. After prepping and draping, an superomedial portal is established. A fluid pump is used to promote hemostasis and adequate visualization. Care is taken to keep pressure relatively low to avoid fluid extravasation. This has not been found to be a problem nor have elevated compartment pressures. An anterolateral portal is established for the arthroscope. The hematoma is evacuated until reasonable visualization is possible. Once pathology can be visualized, an anteromedial portal is established after localization with a spinal needle. An arthroscopic probe is then used to dislodge any clotted blood or debris at the site of fracture (Fig. 2-2).
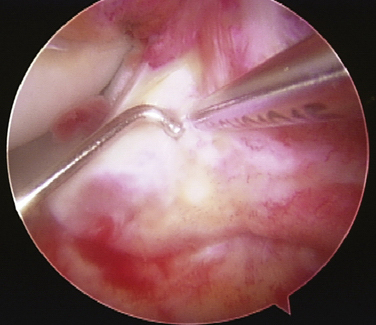
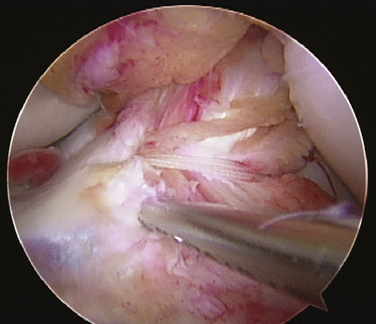
A synovial resector (4.5 mm) is used to débride the region further and to remove any debris from the fracture bed. Once the fracture site has been débrided, the probe is used to attempt a reduction. Interposition of the intermeniscal ligament or the menisci requires use of the probe to hold the soft tissue structures out of the way while attempting to reduce the fragment with an ACL guide or probe. An accessory medial portal is created 1.5 to 2.0 cm medial to the anteromedial portal for the probe. In patients in whom the intermeniscal ligament prevents reduction and also cannot be mobilized, resection is performed. Once the fracture has been reduced, a 0.062-inch Steinmann pin is placed percutaneously from a medial parapatellar position to hold the fracture reduced (Fig. 2-3).
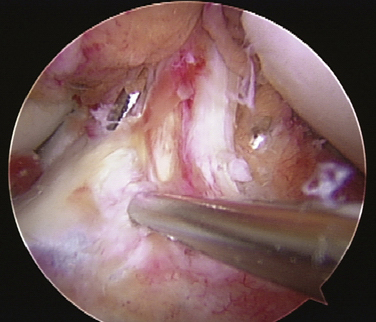
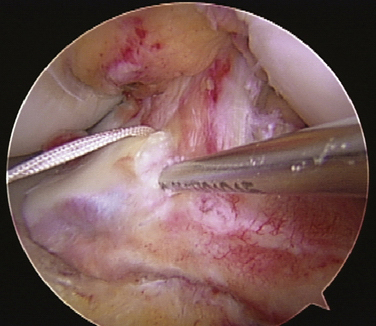
Suture fixation should be used when the fracture is small or comminuted, or in the presence of open growth plates. Some have advocated using the suture methods for all patients because these result in less risk (neurovascular bundle) and less secondary procedures (hardware removal) 25,26 These authors favor the suture technique in all cases. After the fracture is reduced and held in position with the Steinmann pin, the ACL tibial tunnel guide is used to pass a 2.4-mm guide pin through the anteromedial tibial metaphysis, entering the joint on the medial side of the fragment (Fig. 2-4). A second wire is passed starting 1 to 2 cm lateral to the first hole on the tibial cortex, entering the knee at the lateral side of the fragments (Fig. 2-5). The first wire is removed and, immediately after removal, a Hewson suture passer (Smith & Nephew Endoscopy, Andover, Mass) is passed up the hole and two Ultrabraid sutures (Smith & Nephew Endoscopy) are delivered into its loop through the anteromedial portal and pulled out the anteromedial tibia (Fig. 2-6). The second wire is taken out and the Hewson suture passer is immediately placed into the joint (Fig. 2-7). The opposite end of the ULTRABRAID suture(s) are delivered into its loop and pulled out the tibia (Fig. 2-8). A crochet hook or blunt probe is passed into the subcutaneous tissue through one of the suture holes, hooking the opposite sutures, and pulling them out the same hole. A knot is tied and passed through the skin puncture hole and subcutaneous tissue and is secured tightly to the tibial cortex. Each suture is tied and secured individually (Fig. 2-9). This provides firm fixation of the fracture fragment and can be visualized directly.
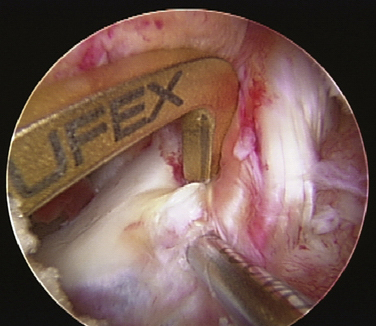
FIGURE 2-4 The ACL tibial tunnel guide is used to pass a 2.4-mm wire on the medial side of the fragment.
PEARLS& PITFALLS
PEARLS
COMPLICATIONS
Although a good outcome is usually expected for fractures of the tibial eminence, complications do occur. Residual laxity after fixation is commonly found after arthroscopic reduction and fixation. Although multiple studies have reported results verifying positive Lachman tests and a difference in laxity from the contralateral uninjured extremity, most patients have functional stability and are not adversely affected.7,15-17,27 Evidence of clinical instability warrants revision with ACL reconstruction.
Painful or symptomatic hardware is common with the use of cannulated screws. Loss of full knee extension can occur secondary to scar tissue or a prominent screw in the intercondylar notch. It has been demonstrated that at the time of hardware removal, soft tissue interposition is the rule, and that excision combined with implantation removal results in excellent outcomes.28
1. Kendall NS, Hsu SYC, Chan K. Fracture of the tibial spine in adults and children. J Bone Joint Surg Br. 1992;74:848-852.
2. Meyers, MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1959;41:209-222.
3. Gronkvist H, Hirsch G, Johansson L, et al. Fracture of the anterior tibial spine in children. J Pediatr Orthop. 1984;4:465-468.
4. Wiss DA, Watson JT. Fractures of the tibial plateau. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD, editors. Rockwood and Green’s Fractures in Adults. Philadelphia: Lippincott-Raven; 1996:1920-1953.
5. Chandler JT, Miller TM. Tibial eminence fracture with meniscal entrapment. Arthroscopy. 1995;11:499-502.
6. Owens BD, Crane GK, Plante T, et al. Treatment of type III tibial intercondylar eminence fractures in skeletally immature atrhletes. Am J Orthop. 2003;33:103-105.
7. Wiley JJ, Baxter MP. Tibial spine fractures in children. Clin Orthop Relat Res. 1990;(255):54-60.
8. Meyers MH, McKeevor FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am. 1970;52:1677-1683.
9. Noyes FR, DeLucas JL, Torvik PJ. Biomechanics of anterior cruciate ligament failure: an analysis of strain-rate sensitivity and mechanism of failure in primates. J Bone Joint Surg Am. 1974;56:236-253.
10. Zaricznyj B. Avulsion fracture of the tibial eminence treated by open reduction and pinning. J Bone Joint Surg Am. 1997;59:1111-1114.
11. McLennan JG. The role of arthroscopic surgery in the treatment of fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Br. 1982;64:477-480.
12. Falstie-Jensen S, Sondergard Peterson PE. Incarceration of the meniscus in fractures of the intercondylar eminence of the tibia in children. Injury. 1984;15:236-238.
13. Schatzker J. Tibial plateau fractures. In: Browner BD, Jupiter JB, Levine AM, Trafton PG, editors. Skeletal Trauma. Philadelphia: WB Saunders; 1992:1745-1770.
14. Lubowitz JH, Elson WS, Guttmann D. Part I: arthroscopic management of tibial plateau fractures. Arthroscopy. 2004;20:1063-1070.
15. Baxter MP, Wiley JJ. Fractures of the tibial spine in children. J Bone Joint Surg Br. 1988;70:228-230.
16. Willis RB, Blokker C, Stoll TM, et al. Long-term follow-up of anterior tibial eminence fractures. J Pediatr Orthop. 1993;13:361-364.
17. Lee Y, Chin L, Wang N, et al. Anterior tibial spine fracture in children: follow-up evaluation by biomechanical studies. Chin Med J. 1996;58:183-189.
18. Beaty JH, Kumar A. Fractures about the knee in children. J Bone Joint Surg Am. 1994;76:1870-1880.
19. Fyfe IS, Jackson JP. Tibial intercondylar fractures in children: a review of the classification and the treatement of malunion. Injury. 1981;13:165-169.
20. Lubowitz JH, Elson WS, Guttman D. Part II: arthroscopic treatment of tibial plateau fracturesintercondylar eminence avulsion fractures. Arthroscopy. 2005;21:86-92.
21. Mah JY, Otsuka NY, Mclean J. An arthroscopic technique for the reduction and fixation of tibial-eminence fractures. J Pediatr Orthop. 1996;16:119-121.
22. Janarv P, Westblad P, Johansson C, et al. Long-term follow-up of anterior tibial spine fractures in children. J Pediatr Orthop. 1995;15:63-68.
23. Osti L, Merlo F, Bocchi L. Our experience in the arthroscopic treatment of fracture-avulsion of the tibial spine. Chir Organi Mov. 1997;82:295-299.
24. Matthews DE, Geissler WB. Arthroscopic suture fixation of displaced tibial eminence fractures. Arthroscopy. 1994;10:418-423.
25. Hunter RE, Willis JA. Arthroscopic fixation of avulsion fractures of the tibial eminence: technique and outcome. Arthroscopy. 2004;20:113-121.
26. Lubowitz JH, Grauer JD. Arthroscopic treatment of anterior cruciate ligament avulsion. Clin Orthop Relat Res. 1993;294:242-246.
27. Smith JB. Knee instability after fractures of the intercondylar eminence of the tibia. J Pediatr Orthop. 1984;4:462-464.
28. Senekovic V, Veselko M. Anterograde arthroscopic fixation of avulsion fractures of the tibial eminence with a cannulated screw: five-year results. Arthroscopy. 2003;19:54-61.