CHAPTER 4 Arthroscopic Treatment of Radial-Sided TFCC Lesions
Functional Anatomy of TFCC
The triangular fibrocartilage complex (TFCC) is a ligamentous structure composed of fibrocartilage located between the distal ulna and the ulnar carpus.1,2 The TFCC has several functions, the most important of which is to stabilize the ulnar carpus.3 The TFCC also provides a continuous gliding surface across the distal face of the radius and ulna for flexion-extension and translational movements. It provides a flexible mechanism for stable rotational movements of the radiocarpal unit around the ulnar axis, and cushions the forces transmitted through the ulnocarpal axis.4 The TFCC improves functional stability of the wrist while allowing 6 degrees of motion: flexion, extension, supination, pronation, and radial and ulnar deviation. The TFCC functionally enhances the surface area of joint contact between the radius and ulna to the carpus.
The TFCC consists of several discrete anatomical structures that when combined form a functional unit.2 The dorsal and volar radioulnar ligaments encase the articular disc and create the distal radioulnar joint. The ulnar collateral ligament, the meniscal homologue, the tendon sheath of the extensor carpi ulnaris, and the ulnocarpal ligaments intimately attach to the articular disc. This broadly based disc adheres to the radial sigmoid notch and extends to the ulnar styloid.
The TFCC transmits axial load from the wrist to the forearm in a longitudinal direction across the ulnar column of the wrist.3 Force is transmitted across the ulnar aspect of the lunate, the triquetrum, and the TFCC on the distal radioulnar joint. The bony morphology of these structures reflects an adaptation to the unique demands on this part of the wrist. Densitometric studies have demonstrated patterns of enhanced subcortical mineralization in the bones of the ulnar wrist. The patterns of increased mineralization correspond to the distribution of force in a longitudinal direction across the ulnar column of the wrist.5
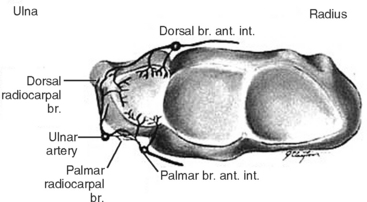
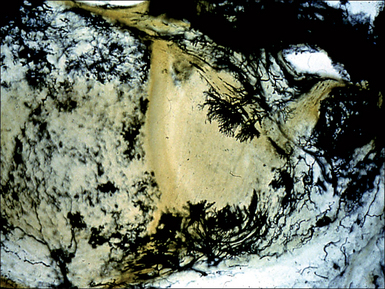
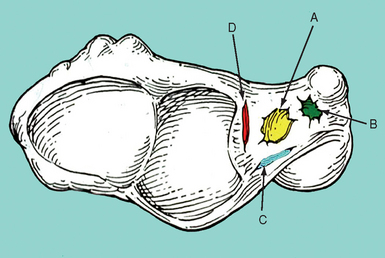
The vascular anatomy of the TFCC is variable, and is in part responsible for the differences in outcomes resulting from different patterns of injuries. Perfusion to the TFCC arises from dorsal and palmar branches of the anterior interosseus artery. Dorsal and palmar branches of the ulnar artery supply the ulnar styloid and the ulnar aspect of the volar periphery (Figure 4.1).6,7 Studies of the vascular anatomy of the TFCC have demonstrated that vessels supply the TFCC from the palmar, ulnar, and dorsal attachments of the joint capsule in a radial fashion—and that the blood flow penetrates less than 20% of the periphery (Figure 4.2).6,8,9 The central portion of the TFCC is therefore relatively avascular. Although the radial aspect of the disc is hypovascular compared to the ulnar side, some radial-sided vascularity has been documented in cadaveric studies—suggesting that healing is possible in this region.9
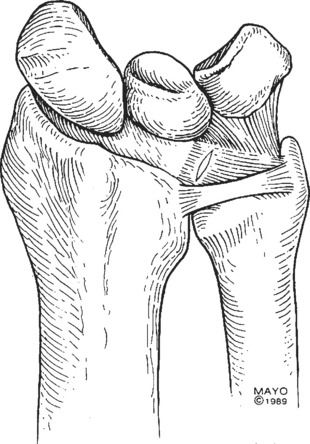
The radial insertion of the TFCC is vulnerable to injury when axial load is combined with pronation and ulnar deviation or extension of the wrist. This motion exposes the TFCC to shear stress, which if substantial enough causes distortion of the TFCC. Extreme stress loads can result in a TFCC tear and subsequent degeneration of the TFCC from its radial insertion (Figures 4.3 and 4.4).10
Patterns of TFCC Injury
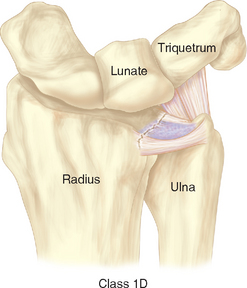
The TFCC transmits force from the wrist to the forearm, and injuries to the TFCC are a common cause of ulnar-sided wrist pain. When evaluating TFCC injuries, it is important to distinguish between age-related (degenerative) and traumatic etiologies. A useful classification system for TFCC injuries was established by Palmer (Figure 4.5 and Table 4.1).11
Table 4.1 Palmer’s Classification of TFCC Lesions (Acute and Degenerative)
| Class 1: Traumatic |
Classification from Palmer AK. Triangular fibrocartilage complex lesions: A classification. J Hand Surg [Am] 1989;14:594–606.
Age-related nontraumatic lesions to the TFCC are typically characterized by central perforations.8,12 In a study of 180 wrist joints in 100 cadavers ranging in age from fetuses to 94 years, Mikic demonstrated that degeneration of the TFCC begins in the third decade of life. He showed that this degeneration increases in frequency and severity as people age. After the fifth decade of life, he noted 100% of TFCCs to be abnormal appearing. It is important to note, however, that these age-related TFCC lesions are often asymptomatic.13
Evaluation of Radial-Sided TFCC Injuries
Patients with radial-sided TFCC injuries typically present with ulnar-sided wrist pain and clicking.14–16 Frequently, a history of a fall onto a pronated and hyperextended wrist can be elicited. Class 1D injuries are frequently associated with distal radius fractures.17 Upon clinical examination, the examiner may note crepitus of the DRUJ during active supination and ulnar deviation. The patient may experience pain in the region of the DRUJ, with dorsopalmar translation of the distal ulna. As a provocative test, the examiner can fix the patient’s wrist in ulnar deviation while rotating the forearm between pronation and supination. A click may indicate a tear of the TFCC, which is interposed between the carpus and the ulnar head. If the injury is advanced, and osteoarthritis has caused deterioration of the sigmoid notch, the patient may experience pain when lateral force is applied to the ulna (compressing it into the radius). The stability of the DRUJ should also be assessed.
Numerous modalities are useful in evaluating the location of injury within the TFCC. Triple-injection wrist arthrography is particularly valuable in detecting Palmer class 1D lesions.18,19 With this procedure, 5 to 10 ml of contrast agent is injected into the ulnar aspect of the wrist, tangent to the triquetrum, under continuous radiographic visualization. This allows examination of the distribution and flow of contrast through the wrist (Figure 4.6).
MRI has become the most widely utilized imaging modality for the evaluation of TFCC injuries.20,21 Using dedicated small-joint wrist coils, MRI predicts lesions of the TFCC with approximately 80% sensitivity and 70% specificity.22 Fat suppression T2-weighted images in the coronal plane can best elucidate the precise anatomical details of the TFCC. MRI has the capacity to localize lesions to the central part of the disc, the periphery, and the radial insertion (Figure 4.7). This specificity can aid in the surgical planning for the treatment of such lesions.
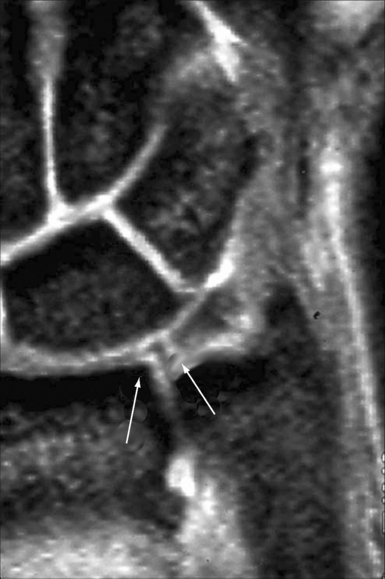
FIGURE 4.7 MRI of the wrist. A T2-weighted coronal image shows a tear at the radial attachment of the TFCC.
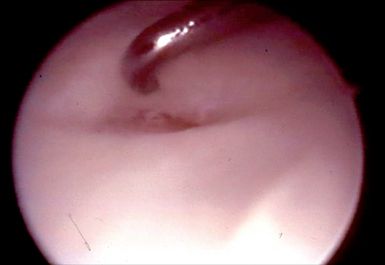
Wrist arthroscopy has recently become the criterion standard for both diagnosing and treating lesions of the TFCC. When compared to MRI and arthrography, arthroscopy most accurately determines the location of lesions and the size of tears. It also allows determination of whether a flap is unstable.23,24 Scar and vascular invasion along the periphery of the TFCC, as well as tears within the lunotriquetral interosseous ligament or ECU subsheath, indicates injury. Specifically, a trampoline test is positive when the surgeon’s probe fails to bounce off the TFCC, indicating laxity of the disc and the presence of a tear (Figure 4.8).25 It is important to note, however, that laxity of the TFCC does not necessarily translate into instability of the DRUJ.26
Surgical Treatment of Radial-Sided TFCC Lesions
The anatomy and patterns of injury to the TFCC are well elucidated. Efforts now focus on the optimal treatment of different types of lesions. With recent advances in small-joint arthroscopy, arthroscopic debridement and repair of TFCC lesions are now possible. Historically, treatment of most tears of the TFCC (particularly those involving the avascular horizontal disc) emphasized debridement or excision.14,27,28 This practice stemmed from two important principles. First, the variable vascular perfusion to the different regions of the TFCC was thought to create a suboptimal biologic environment for the healing of repairs. This is known to be especially true in the central portion of the disc, where vascular penetration is negligible.6,8,9
Several investigators also questioned whether there was significant penetration of vessels in the radial aspect of the TFCC, and proposed that class 1D lesions be treated in a similar fashion to central lesions (with debridement).6 Second, biomechanical studies of the stability of the horizontal disc showed that no significant kinematic or structural changes result if debridement involves less than two-thirds of the disc and spares the peripheral 2 mm of the disc.5
Currently, the optimal treatment for radial-sided avulsions of the TFCC is a subject of considerable controversy. When compared to arthroscopic repair, the advantages of arthroscopic debridement include decreased operative time, decreased recovery time (with a shorter period of immobilization), fewer complications, and better range of motion.14
We have previously shown that in 52 patients arthroscopic debridement of TFCC tears provided complete relief of pain in 73%. Of these lesions, 34% were radial-sided tears. Our technique consisted of using small pituitary rongeurs or punches, as well motorized shavers to debride the defect edges. We noted no clinical ulnar wrist instability in follow-up. Similar outcomes were recently reported by Husby and Haugstvedt, who demonstrated excellent clinical outcomes after arthroscopic debridement of central and radial TFCC tears (with high patient satisfaction and no complications).29
Despite convincing data regarding the functional outcomes in patients undergoing debridement of radial-sided TFCC lesions, further research has emphasized the importance of the peripheral attachments of the TFCC in stabilizing the distal radioulnar joint. These attachments also provide support for the ulnocarpal joint.4,11 This observation has led several investigators to advocate repair of certain peripheral TFCC tears in order to increase stability.25,30,31 A number of techniques for reattachment of class 1B and 1C TFCC tears have been described with positive clinical results, confirming the ability of lesions in these regions to heal. The optimal treatment of radial-sided class 1D lesions remains controversial.
It is uncommon for a class 1D tear to cause instability of the DRUJ in the absence of a distal radius fracture, which is the most common cause of DRUJ instability.26 The examiner should examine the volar and dorsal aspects of the wrist and forearm for swelling and symmetry with the other wrist. Increased anteroposterior translation of the ulna on the radius during passive movement of the DRUJ when compared to the contralateral side provides evidence for instability.32 A provocative maneuver for DRUJ instability can be performed by depressing the patient’s distal ulna from dorsal to volar with the wrist in pronation. A positive piano-key sign is characterized by volar laxity of the ulnar head in the affected wrist when compared with the contralateral wrist.
In the setting of a distal radius fracture with concomitant DRUJ instability, accurate fracture reduction and maintenance of the reduction are imperative for healing of the disrupted joint.33 After reduction of a distal radius fracture, it is important to test the stability of the DRUJ. The secondary stabilizers of the DRUJ (namely, the ulnocarpal ligaments, ECU subsheath, interosseous membrane, and lunotriquetral interosseous ligament) typically maintain sufficient stability of the joint to allow healing after fracture reduction.34 If, however, a radial TFCC tear is identified during the arthroscopic treatment of a distal radius fracture securing the radial side of the disc to the sigmoid notch using a 0.035-inch Kirschner wire will typically promote healing of the radial attachment. Severe or bidirectional DRUJ instability that persists after fracture reduction and fixation indicates that the secondary stabilizers of the DRUJ, including the TFCC, have been progressively injured and may be contributing to joint instability. In this situation, open repair of the TFCC may be indicated.
Repairing the torn TFCC to the sigmoid notch of the radius has been described using both open and arthroscopic approaches. Cooney described a technique for an open suture repair of peripheral lesions through a dorsal approach (Figure 4.9).35 Thirty-three patients with peripheral rim tears not associated with instability of DRUJ joint underwent open repair, combined with debridement of the ulnar border of the radius to promote vascular ingrowth. He reported good to excellent results in 80% of the patients. At two-year follow-up, MRI showed continuity of the repair in a small subgroup of patients within the series.
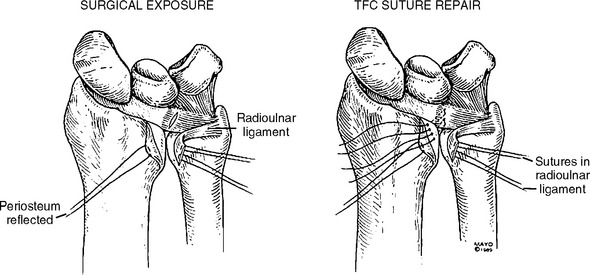
FIGURE 4.9 Repair of a class 1D injury using an open, dorsal approach and placement of transosseus sutures.
(Reproduced with permission by Cooney WP, Linscheid RL, et al. Triangular fibrocartilage tears. J Hand Surg [Am] 1994;19:143–54.)
Miniami coupled open reattachment of peripheral TFCC tears with hemiresection-interposition arthroplasty of the DRUJ to avoid impingement of the ulnar head against the reconstructed disc. He reported complete relief of pain in 63% of patients.31
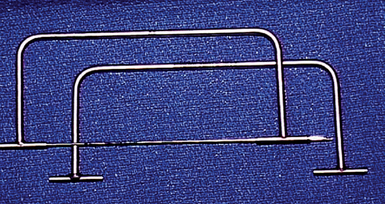
Numerous arthroscopic techniques have subsequently been described for radial-sided TFCC lesions. Jantea reported a series of 12 patients with radial-sided TFCC tears who underwent arthroscopic repair by means of transosseus sutures.36 His technique involves using a rectangular guiding device mounted on the dorsal wrist, which allows accurate underpinning of the TFCC tear (Figure 4.10). A 0.045-inch Kirschner wire is first inserted through the ulnar wrist in the interval between the ECU and FCU tendons. The wire exits at the point on the sigmoid notch where the TFCC inserts. A small skin incision is made on the radial side of the wrist between the first and second compartment, carefully avoiding injury to the superficial branch of the radial nerve, the radial artery, and the extensor tendons.
Trumble described an alternative technique that employs a cannula and preloaded meniscal repair needle instead of a wire guide.37 In his series, which emphasized repair of class 1D lesions, postoperative range of motion and grip strength averaged greater than 80% compared to the contralateral side. Follow-up studies showed that repairs were intact in 12 out of 15 patients.
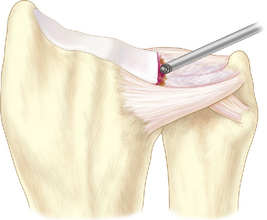
Sagerman and Short treated 14 patients with class 1D TFCC tears with arthroscopic reattachment in a similar fashion using a direct suture technique.38 In accordance with Chidgey’s theory that introducing additional vascularity to the radial attachment of the TFCC improves healing, the authors emphasized the use of a motorized bur to abrade the edge of the sigmoid notch (Figure 4.11) before reconnecting the radial attachment (Figure 4.12).1 Follow-up yielded 67% of patients with good or excellent clinical results.
Fellinger described repair of the torn disc to the radial sigmoid notch using a T-Fix device (Acufex).39 With this procedure, a K-wire is passed from distal to proximal through an ulnar skin incision and into the sigmoid notch under arthroscopic guidance. The wire is advanced until it reaches the opposite radial cortex, which is then overreamed using a cannulated 2.5-mm drill. Through a separate radial-sided skin incision, the T-Fix device is inserted into the canal until the tip reaches the sigmoid notch. Using arthroscopic guidance and assistance, the base of the disc is perforated with the tip of the application device.
Personal Series
Five patients underwent an in-out suture repair similar to that described by Short and Sagerman. Three patients were treated with a repair similar to that described by Jantea, utilizing a jig type of pin-guiding device (Figure 4.10). Three patients underwent repair with the T-Fix bone anchor device, as described by Fellinger. Regardless of the technique employed, all repairs utilized 2–0 PDS suture on meniscal needles. The suture limbs were tied over a bone bridge on the radial aspect of the distal radius (Figure 4.13). In addition, in order to promote vascular in-growth to the radial portion of the disc the sigmoid notch was abraded with a bur before the ligament was reattached in each of the repairs (Figure 4.11).
In both the debridement and the repair group, all ulnar-sided lesions were repaired. The average total operative time was 92 minutes for the repair group, compared to 43 minutes for the debridement group. The postoperative protocol for the debridement group included splinting for one week, followed by free wrist range of motion thereafter. Sixty percent of patients participated in formal hand therapy, and the average time to return to work was seven weeks. In contrast, the patients who underwent repair were kept immobilized for three weeks. One hundred percent of patients in this group participated in formal hand therapy, and the average time to return to work was 16 weeks.
Author’s Preferred Technique
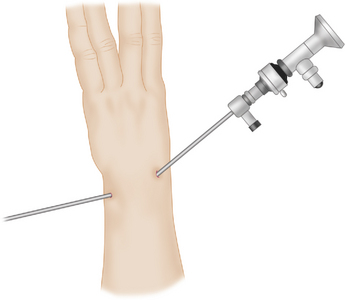
When an isolated radial-sided TFCC tear exists with a stable DRUJ, debridement of the lesion is a simple procedure that removes the reactive tissue and allows early return of wrist motion and function. Under regional anesthesia, the patent’s wrist is reexamined to confirm stability of the DRUJ and to identify abnormal clicking or ECU subluxation. A well-padded pneumatic tourniquet is applied to the upper arm, and the wrist is placed in traction using a standard traction tower set to 12 pounds (Figure 4.14). After gravity exsanguination of the limb, the tourniquet is inflated to 250 mmHg. A standard 3-/,4 portal is made using a #11 scalpel. The subcutaneous tissues are dissected down to the level of the joint capsule using a small curved clamp in order to protect the branches of the radial sensory nerve. A small capsulotomy is performed, and a 30-degree 2.3-mm-diameter arthroscope is inserted into the portal.
Initially, the radial side of the wrist is systematically examined. The arthroscope is then directed ulnarly to evaluate the entire TFCC. Once a class 1D lesion is confirmed, the ulnar portal is placed (typically in the 6-R location)—being mindful to avoid injury to the sensory branch of the ulnar nerve (Figure 4.12). Through this portal a small arthroscopic probe is inserted to assess the stability of the torn flap and the TFCC tension. A 3.5 motorized suction shaver is then inserted and used to debride any synovitis and to smooth the edges of the defect. Unstable flaps are resected using small-joint suction punches. Once the lesion is debrided, the midcarpal joint is inspected.
Once the arthroscopic procedure is complete, the wrist is reexamined under anesthesia. The clicks that were noted previously have typically resolved. The portal sites are then closed with a single suture using 4–0 nylon, and a splint is applied. The splint is worn continuously for the first week to support the wrist, and then worn intermittently for an additional three weeks while the patient avoids repetitive rotatory wrist activity or forceful grasping. The critical points are summarized in Table 4.2.
Table 4.2 Critical Points: Arthroscopic Debridement of Isolated Class 1D TFCC Tears
| Indications |
Controversies
The results of arthroscopic reattachment of isolated radial-sided TFCC lesions have been promising. Despite studies suggesting hypovascularity of the radial aspect of the TFCC, vascular in-growth and/or synovial fluid diffusion presumably provide adequate nutritional support to allow 1D lesions of the TFCC to heal. Clearly, arthroscopic repair of TFCC tears has the potential to offer advantages—including increased stability of the DRUJ. This is especially true for class 1B and 1C lesions. Many techniques have been described for arthroscopic repair of class 1D lesions, with promising short-term results.20,36–38,40 Few long-term results, however, are available from these studies. In addition, further studies are necessary to clarify the optimal suture technique and the size, number, and placement of sutures.
Whether the outcomes after arthroscopic reattachment of class 1D lesions are superior to those following simple debridement has yet to be proven. A retrospective study by Miwa of 62 wrists treated with either arthroscopic debridement or repair of TFCC lesions showed no statistically significant difference in clinical outcomes between the debridement group and the repair group in any class, including class 1D lesions.41 These results are similar to those from our own series, suggesting that debridement remains a simple and effective means of treating radial-sided TFCC tears.
Arthroscopic debridement of class 1D lesions offers the advantages of being technically simple and safe, with a low potential for complications and short operative time. Long-term data suggests that DRUJ stability is not compromised after disc debridement, which calls into question the theoretical advantage of repair.29 Furthermore, if arthroscopic debridement is unsuccessful in relieving pain or providing stability it does not preclude a future repair.
1 Chidgey LK, Dell PC, Bittar ES, Spanier SS. Histologic anatomy of the triangular fibrocartilage. J Hand Surg [Am]. 1991;16(6):1084-1100.
2 Kauer JMG. The articular disc of the hand. Acta Anat. 1975;93:590-605.
3 Palmer AK, Glisson RR, Werner FW. Relationship between ulnar variance and TFCC thickness. J Hand Surg [Am]. 1984;9:681-683.
4 Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist: Anatomy and function. J Hand Surg [Am]. 1981;6:153-162.
5 Adams BD. Partial excision of the triangular fibrocartilage complex articular disk: A biomechanical study. J Hand Surg [Am]. 1993;18:334-340.
6 Bednar MS, Arnoczky SP, Weiland AJ. The microvasculature of the triangular fibrocartilage complex: Its clinical significance. J Hand Surg [Am]. 1991;16(6):1101-1105.
7 Osterman AL, Hunt TR, Bednar JM, Bozentka DJ. Vascularity of the triangular fibrocartilage as measured in vivo. Presented at the 49th annual meeting of the American Society for Surgery of the Hand, Cincinnati, OH, 1994.
8 Mikic ZD. Age changes in the triangular fibrocartilage of the wrist joint. J Anat. 1978;126(2):367-384.
9 Thiru-Pathi RG, Ferlic DC, Clayton ML, McClure DC. Arterial anatomy of the triangular fibrocartilage of the wrist and its surgical significance. J Hand Surgery [Am]. 1986;11:258-263.
10 Melone CP, Nathan R. Traumatic disruption of the triangular fibrocartilage complex. Clin Orthop. 1992;275:65-73.
11 Palmer AK. Triangular fibrocartilage complex lesions: A classification. J Hand Surg [Am]. 1989;14:594-606.
12 Viegas SF, Ballantyne G. Attritional lesions of the wrist joint. J Hand Surg [Am]. 1987;12:1025-1029.
13 Culp R, Osterman L, Kaufmann R. Wrist arthroscopy: Operative procedures. In: Green D, Hotchkis R, Pederson W, Wolfe S, editors. Green’s Operative Hand Surgery. Fifth Edition. Philadelphia: Elsevier; 2005:786.
14 Osterman AL. Arthroscopic debridement of triangular fibrocartilage complex tears. Arthoscopy. 1990;6:120-124.
15 Osterman AL, Terrill RG. Arthroscopic treatment of TFCC lesions. Hand Clinics. 1991;7:277-281.
16 Terrill RQ. Use of arthroscopy in the evaluation and treatment of chronic wrist pain. Hand Clinics. 1994;10:593-604.
17 Lindau T, Arner M, Hagberg L. Intraarticular lesions in distal fractures of the radius in young adults: A descriptive arthroscopic study in 50 patients. J Hand Surg [Br]. 1997;22B:638-643.
18 Levinsohn EM, Rosen ID, Palmer AK. Wrist arthrography: Value of the three compartment injection method. Radiology. 1991;179:231-239.
19 Zinberg EM, Palmer AK, Coren AB, Levinsohn EM. The triple injection wrist arthrogram. J Hand Surg [Am]. 1988;13:803-809.
20 Giovagnoni A, Misericordia M, Terrilli F, et al. Magnetic resonance in the diagnosis of lesions of the carpal triangular fibrocartilage: The experience with 49 patients with chronic pain at the wrist. Radiol Med (Torino). 1993;85:12-16.
21 Oneson SR, Timins ME, Scales LM, et al. MR imaging diagnosis of triangular fibrocartilage pathology with arthroscopic correlation. Am J Roentgenol. 1997;168:1513-1518.
22 Nakamura T, Yabe Y, Horiuchi Y. Fat suppression magnetic resonance imaging of the triangular fibrocartilage complex: Comparison with spin echo, gradient echo pulse sequences and histology. J Hand Surg [Br]. 1999;24(1):22-26.
23 Pederzini L, Luchetti R, Soragni O, et al. Evaluation of the triangular fibrocartilage complex tears by arthroscopy, arthrography, and magnetic resonance imaging. Arthroscopy. 1992;8:191-197.
24 Weiss APC, Akelman E, Lambiase R. Comparison of the findings of triple injection cine-arthrography of the wrist with those of arthroscopy. J Bone Joint Surg Am. 1996;78:348-356.
25 Hermansdorfer JD, Kleinman WB. Management of chronic peripheral tears of the triangular fibrocartilage complex. J Hand Surg [Am]. 1991;16:340-346.
26 Adams BD. Distal radioulnar instability. In: Green D, Hotchkis R, Pederson W, Wolfe S, editors. Green’s Operative Hand Surgery. Fifth Edition. Philadelphia: Elsevier; 2005:612-616.
27 Imbriglia JE, Boland DS. Tears of the articular disc of the triangular fibrocartilage complex: Results of excision of the articular disc. J Hand Surg [Am]. 1984;9:527-530.
28 Menon J, Wood VE, Schoene HR, Frykman GK, Hohl JC, Bestard EA. Isolated tears of the triangular fibrocartilage of the wrist: Results of partial excision. J Hand Surg [Am]. 1984;9(4):527-530.
29 Husby T, Haugstvedt JR. Long-term results after arthroscopic resection of lesions of the triangular fibrocartilage complex. Scand J Plast Reconstr Hand Surg. 2001;35:79-83.
30 Nagle DJ, Benson LS. Wrist arthroscopy: Indications and results. Arthroscopy. 1992;8(2):198-203.
31 Minami A, Kaneda K, Itoga H. Hemiresection-interposition arthroplasty of the distal radioulnar joint associated with repair of triangular fibrocartilage complex lesions. J Hand Surg [Am]. 1991;16(6):1120-1125.
32 Morrissy RT, Nalebuff EA. Dislocation of the distal radioulnar joint: Anatomy and clues to prompt diagnosis. Clin Orthop. 1979;144:154-158.
33 Ekenstam F, Jakobsson OP, et al. Repair of the triangular ligament in Colles’ fracture: No effect in a prospective randomized study. Acta Orthop Scand. 1989;60:393-396.
34 Pardubsky P, Adams BD. The distal radioulnar joint in fracture of the wrist. Tech Orthop. 2000;15:353-358.
35 Cooney WP, Linscheid RL, et al. Triangular fibrocartilage tears. J Hand Surg [Am]. 1994;19:143-154.
36 Jantea CJ, Baltazar A, Ruther W. Arthroscopic repair of radial-sided lesions of the fibrocartilage complex. Hand Clinics. 1995;11(1):31-36.
37 Trumble TE, Gilbert M, Vedder N. Arthroscopic repair of the triangular fibrocartilage complex. Arthroscopy. 1996;12(5):588-597.
38 Sagerman SD, Short W. Arthroscopic repair of radial-sided triangular fibrocartilage complex tears. Arthroscopy. 1996;12(3):339-342.
39 Fellinger M, Peicha G, Seibert FJ, Grechenig W. Radial avulsion of the triangular fibrocartilage complex in acute wrist trauma: A new technique for arthroscopic repair. Arthroscopy. 1997;13(3):370-374.
40 Trumble TE, Gilbert M, et al. Ulnar shortening combined with arthroscopic repairs in the delayed management of triangular fibrocartilage complex tears. J Hand Surg [Am]. 1997;22:807-813.
41 Miwa H, Hashizume H, Fujiwara K, Nishida K, Inoue H. Arthroscopic surgery for traumatic triangular fibrocartilage complex injury. J Orthop Sci. 2004;9(4):354-359.