CHAPTER 11 Arthroscopic Treatment of Lunotriquetral Ligament Injuries
Mechanism of Injury
The wrist is an extremely complex joint.1 Its osseous and ligamentous anatomy as well as the normal carpal kinematics have been well studied.2–5 There are intrinsic ligaments that both insert and originate on the carpal bones, and extrinsic ligaments that insert on the carpal bones but originate on the wrist outside the carpus. The LTIL is the intrinsic interosseous ligament that stabilizes the lunate to the triquetrum (i.e., the LTJ). The LTJ is found along the ulnar portion of the proximal carpal row (PCR), which consists of the scaphoid, lunate, and triquetrum.
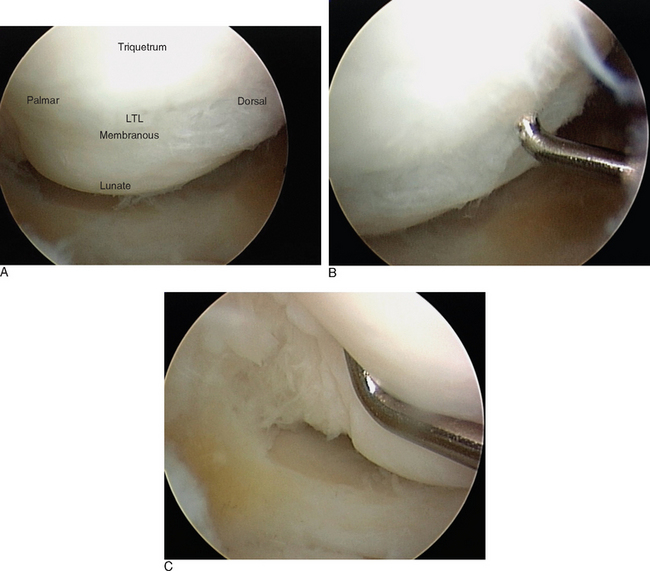
The PCR acts as an intercalated segment (IS), providing a mechanical linkage between the distal carpal row and the distal radius and ulna. There are three distinct regions of the LTIL (Figure 11.1). The dorsal and palmar portions are thickened and provide a strong, stable connection at the LTJ. The palmar portion of the LTIL is the thickest and strongest of the three regions, and is most important in the transmission of load and strain from the triquetrum to the lunate. The central, proximal portion of the LTIL consists of a fibrocartilaginous membrane that provides minimal joint stability.6
Carpal instability (CI) is the end result of a wrist ligamentous injury, which may occur from a variety of mechanisms. The failure of wrist ligaments (and the resultant carpal instability) causes pain (i.e., a symptomatic dysfunction), produces abnormal carpal kinetics (i.e., altered stress with the inability to bear functional loads), and abnormal joint kinematics (i.e., abnormal carpal motion).7 The degree of instability can vary from a subtle micro-movement due to ligament attenuation to gross carpal displacement with a wide intracarpal gap and abnormal carpal alignment.8–16
With an injury to the LTIL, the normal kinetics and kinematics of the wrist are disturbed.17,18 A spectrum of LTJ injuries can develop, ranging from a mild sprain with or without dynamic instability to a complete disruption with a secondary carpal instability dissociative (CID) pattern. This may culminate in a static altered carpal alignment, often referred to as volar intercalated segment instability (VISI). A static CI is characterized by a fixed dissociation between carpals that is clearly evident on imaging studies or during arthroscopy. A dynamic CI is characterized by normal routine radiographs, abnormal kinematics on stress imaging, or altered kinetics and kinematics viewed during arthroscopy.
The mechanism of LTIL tearing resulting in injury to the LTJ is somewhat controversial.19 Perilunate and reverse perilunate injury patterns caused by dorsally and/or palmarly applied forces, fractures of the distal radius or carpals, degenerative wear from ulnar abutment, prolonged repetitive stress, and inflammatory arthritis/synovitis have all been implicated.20,21 Furthermore, the presence of an ulnar positive variant at the DRUJ can facilitate attritional wear and tear of the LTIL.22–24
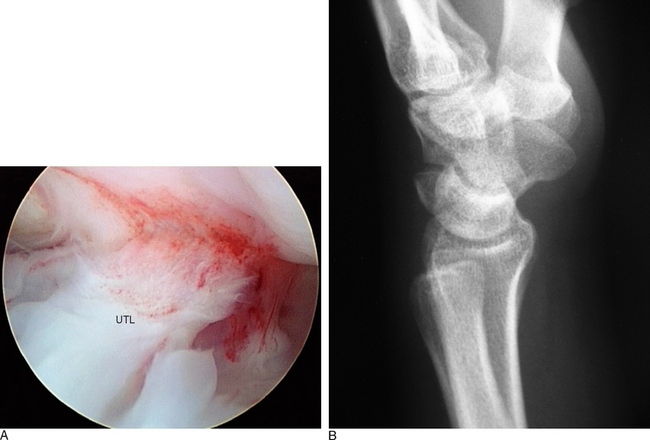
Most investigators believe that when the LTIL is injured subtle micro-motion instability begins, which results in wrist joint synovitis and subsequent chondromalacia.6 Some investigators would consider this early stage as a predynamic instability. Interestingly, damage to the intrinsic interosseous ligament alone is usually not sufficient to cause LTJ dissociation and a grossly unstable VISI. Additional tearing of the secondary constraints to the LTJ is necessary to produce a static CI (Figure 11.2).
Significant injury to either the ulnocarpal ligamentous complex (ULL and UTL) or the dorsal extrinsic ligaments (DRCL and DICL) will then result in a VISI. Secondary attenuation from prolonged cyclic loading may also play an important role.6,15,17 Although these pathomechanics ultimately result in a VISI type of CID pattern, other carpal instabilities of the nondissociative type [i.e., CIND involving the midcarpal joint (MCJ), radiocarpal joint (RCJ), or combined MCJ/RCJ] can produce similar VISI patterns.13,25
Evaluation of LTJ Injuries
The differential diagnosis of ulnar-sided wrist pain is staggering. Extrinsic wrist disorders and internal wrist derangements must be taken into account during the patient history and physical examination. A careful evaluation of the painful wrist will help to differentiate ulnar-sided pain emanating from LTJ injury versus a variety of associated wrist lesions that mimic ulnar-sided wrist pain. These include TFCC injury, DRUJ injury, MCJ injury and instability, cartilage injury producing chondromalacia and degenerative joint disease, UIS, carpal fractures, dorsal extrinsic ligament sprains, pisotriquetral joint injuries, extensor carpi ulnaris (ECU) subluxation, ulnar neurovascular injuries, and inflammatory connective tissue disorders.13,20,21
A typical patient with an LTIL injury usually presents with a history of acute trauma or repetitive stress to the hand and wrist. Symptoms may be recent or chronic. The ulnar-sided wrist pain is usually intermittent to frequent and is worsened with activities, especially those wrist movements that require rotation and ulnar deviation. Wrist motion produces clicking or a clunk. The wrist feels stiff and the grip is weak. The physical examination usually does not reveal a palmar sag of the carpus (which is characteristic of a VISI) but often shows decreased range of motion, clicking, a clunk with movement, or especially painful ulnar deviation or rotation. There is often tenderness to palpation dorsally at the LTJ region or directly ulnarly over the carpus. Provocative tests that stress the LTJ and reveal pain, crepitus, or joint laxity are suggestive of a ligament injury.26–28
Standard plain posteroanterior and lateral radiographs should be obtained on every patient with a suspected LTJ injury. Typically these radiographs are normal, but they might assist with the differential diagnosis of other wrist injuries known to cause ulnar-sided wrist pain. The plain radiographs can be scrutinized for hints of LTJ instability, such as disruptions of Gilula’s lines, a relative malalignment between the lunate and capitate, or possibly a static collapse with a VISI pattern of lunate flexion and triquetral extension (Figure 11.2B). A gap or diastasis between the lunate and triquetrum is virtually never observed. If a VISI is present, the lunate and capitate are no longer colinear and the lunotriquetral axes become negative (mean value of −16 degrees) whereas the mean value is normally positive at 14 degrees.
Some investigators have advocated wrist motion or stress radiographic studies, cineradiography, three-compartment wrist arthrography, nuclear bone scans, computed tomography, and magnetic resonance imaging (MRI).26,29 The author routinely obtains posteroanterior, lateral, and oblique radiographs of the wrist. In those select patients in whom the diagnosis of wrist pain is still indeterminate, a high-resolution 1.5-Tesla MRI is performed and read by an experienced musculoskeletal radiologist. Even though the MRI scan is neither sensitive nor specific for an LTIL tear, it may produce additional information about other associated wrist joint injuries.
Role of Wrist Arthroscopy
The arthroscopic examination of the painful wrist, especially in the evaluation of LTJ injuries, has become the definitive modality of diagnostic investigation. Wrist arthroscopy is an essential component of a thorough examination because it provides the only direct means of inspecting the integrity of the LTIL, the stability of the LTJ, and the presence of associated wrist joint pathology. Subtle LTJ instabilities that were not detected by the other previously described imaging modalities can now be accurately diagnosed with arthroscopy. Wrist arthroscopy of both the RCJ and the MCJ is now the gold standard in the diagnosis of CI based on its superior accuracy in the direct evaluation of ligamentous injuries.19–28,30–40
Treatment of Lunotriquetral Joint Injuries
In an attempt to minimize the surgical trauma of an open wrist operation and to accelerate the rehabilitation process, the treatment of LTJ instability by arthroscopic technique has been recently investigated.19–28,31–50 The technique of arthroscopic ligament debridement and arthroscopic reduction of LTJ injury with internal fixation using K-wires [i.e., arthroscopic reduction and internal fixation (ARIF)] is described in material following.
In the past, treatment of stable acute and chronic LTJ injuries consisted of a period of splint or cast immobilization in conjunction with other supportive conservative measures.10 It is highly unlikely that this approach will work successfully for any serious acute or chronic LTJ instability. Currently it is believed that only minor acute LTIL sprains respond to rest and immobilization. If symptoms do not improve within six weeks, if the clinical examination is consistent with a moderate or severe sprain of the LTIL, if a wrist MRI scan reveals a serious LTJ injury, or if LTJ instability is already present, arthroscopy should be performed. The degree of LTIL damage, degree of LTJ instability (dynamic or static), and level of associated wrist joint pathology determine whether or not to proceed with ARIF or an open surgical technique.
Direct ligament repair, ligament reconstruction with autogenous tendon graft, LTJ arthrodesis, midcarpal arthrodesis, proximal row carpectomy, and total wrist fusion are the open surgical procedures that have been advocated to restore LTJ alignment and thus the integrity of the PCR. Several investigators have recommended direct ligament repair for an acute injury whenever sufficient LTIL remains.10,26,31,43, The LTIL is reattached to the triquetrum, as this is the usual site of avulsion. The repair technique is surgically demanding, and may require both dorsal and palmar approaches. Augmentation of the LTIL repair with a dorsal capsulodesis to improve the extrinsic ligament support has been suggested to be of some benefit.45–47 The results of direct LTIL repair to restore stability of the LTJ have been satisfactory, with the Mayo Clinic reporting an 86% success rate.31
In patients with chronic static LTJ instability with VISI, or in the case of an arthroscopic or open surgical finding of a nonrepairable LTIL, several investigators have recommended LTIL reconstruction with autogenous tendon graft.10,31,44 On the other hand, other investigators have argued that they prefer an LTJ arthrodesis over a tendon graft reconstruction. The technique of LTIL reconstruction utilizing a distally based strip of extensor or flexor carpi ulnaris is an extremely demanding surgical procedure, and may require significant surgical exposure via dorsal and palmar arthrotomies. Advocates of the reconstruction argue that it preserves LTJ motion and near normal carpal kinematics, as opposed to LTJ arthrodesis that entails significant loss of wrist motion. Only a small group of patients have undergone reconstruction, but the Mayo Clinic group has reported good success.10,31
LTJ arthrodesis is a technically less demanding surgical procedure than reconstruction, and has been shown by several investigators to be successful at reducing or eliminating wrist pain and improving function. It has been reported to have a high rate of LTJ nonunion, however, and mild to slight associated stiffness in wrist mobility.51–55 In several comparative studies of LTJ arthrodesis versus reconstruction or repair, the later groups achieved superior results in regard to patient satisfaction, postoperative complications, and necessity for reoperation.26,31
It should be pointed out that in patients with a fixed VISI deformity it is also necessary to consider reconstruction of the palmar ulnocarpal ligaments or the dorsal extrinsic ligaments in order to prevent permanent rotation of the PCR into a VISI.31,56–58 In some wrists, it may even be necessary to proceed to a midcarpal arthrodesis (i.e., lunate-triquetrum-hamate or lunate-triquetrum-hamate-capitate) if restoration of PCR alignment cannot be achieved.20,45–48,53
Ligamentous repair, reconstruction, or joint arthrodesis needs to take into account the presence of degenerative cartilaginous changes or findings of UIS with degeneration of the TFCC and ulnar cartilage.10,20,21,30,31 In these circumstances, an ulnar shortening osteoplasty may also be needed. As an added benefit from an ulnar shortening, it has been shown that the procedure partially stabilizes the ulnar aspect of the wrist through an increased tension in the ulnocarpal ligament complex.59 Furthermore, a debridement of the degenerative TFCC lesion can be performed. In selected cases, an arthroscopic wafer procedure to remove the protuberant dome of the distal ulna might be feasible in place of an ulnar shortening osteotomy.59,60
Arthroscopic Technique
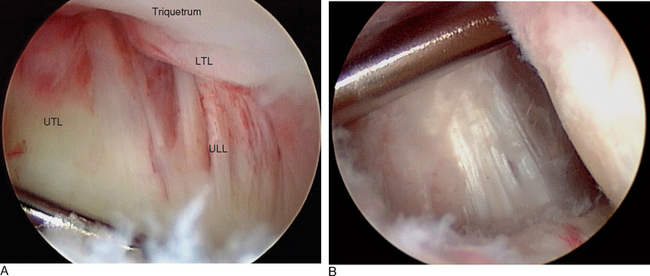
The ulnocarpal ligaments (ULL and UTL) are clearly seen, as is the entire TFCC and the cartilaginous surfaces of the entire PCR (Figure 11.3). The volar portion of the LTIL is best visualized through the ulnar (6-U) portal, where it can be seen in its entirety (Figure 11.1C). As an alternative, a volar wrist portal can be established that also provides excellent viewing of the volar LTIL and dorsal wrist structures such as the DRCL (Figure 11.4B). Associated injuries to the TFCC, extrinsic ligaments, cartilage, and capsule can be assessed with RCJ arthroscopy using a combination of these four portals.
To complete the arthroscopic evaluation of LTJ injury, it is essential to establish midcarpal portals.61 The midcarpal-radial (MCR) portal is the best vantage point to observe the LTJ. Because the LTIL does not extend distally into the MCJ, the interval between the lunate and triquetrum can be seen clearly and instability of the LTJ can be accurately assessed (Figure 11.3). A probe placed into the midcarpal-ulnar (MCU) portal or triquetrohamate (TH) portal can then be used to assess dynamic or static instability. This instability assessment is further enhanced by stress loading the LTJ.
Arthroscopic Classification of Carpal Interosseous Ligament Injury
The degree of LTJ instability can be arthroscopically graded with the Geissler classification scheme.41,62 In the author’s experience, a complete tear of the LTIL with gross dissociation of the LTJ is clearly discernable arthroscopically. The most important subtle arthroscopic observation is whether or not there is attenuation of the LTIL. If attenuation is present, the possibility for instability can range from a predynamic condition with subtle kinetic changes to a more grossly observable dynamic instability with more obvious kinematic carpal alterations of movement. The current Geissler classification does not take into account the important distinction between an attenuated ligament (with or without subtotal tearing) and a ligament injury with no attenuation (with or without subtotal tearing). As such, I have modified the Geissler classification to incorporate these findings (Table 11.1).
| Grade | Arthroscopic Findings |
|---|---|
| 0 | Hemorrhage of interosseous ligament seen in RCJ. No attenuation. No incongruency of carpal alignment in MCJ. |
| I | Incomplete partial or full substance tear of the interosseous ligament as seen in RCJ. No attenuation. No joint incongruency. No instability. |
| II | Attenuation of the interosseous ligament. Most often the central membranous portion is completely torn, and the volar and dorsal portions of the ligament are stretched. Often an incomplete partial or small full substance tear is present. There is possibly a predynamic or mild dynamic instability, as evidenced by excessive joint movement at the MCJ. Usually excessive scar tissue builds up and synovitis is seen in RCJ and possibly MCJ. |
| III | Interosseous ligament is completely torn. Probe can be easily passed through the joint, but a wide diastasis is not present. The joint is dynamically unstable but reducible. No static instability. |
| IV | Gross instability. Marked joint incongruency with static VISI instability. Arthroscope passes through the gap between carpals. |
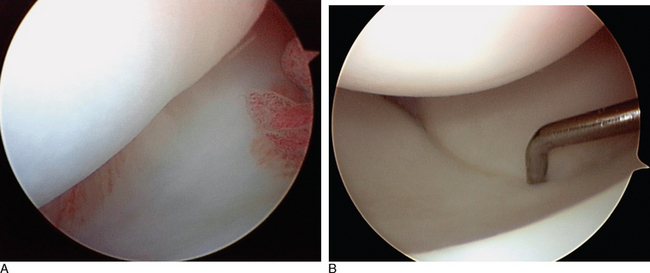
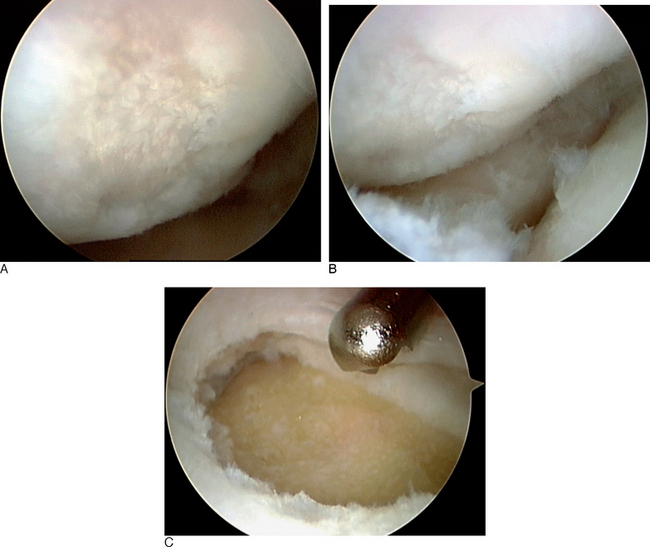
The Geissler grade I interosseous ligament injury class actually comprises several separate and distinct patterns of intrinsic ligament damage. In the first pattern, the LTIL shows evidence of hemorrhage but no attenuation or laxity of its fibers that would be consistent with instability. When a mild sprain of the LTIL occurs, hemorrhage of the ligamentous fibers can be visualized arthroscopically—but as long as the fibers of the ligament have not been stretched beyond their plastic limit of elongation the basic integrity of the LTIL is maintained. Hemorrhage within the LTIL absent any observable attenuation of its fibers leaves the LTJ stable. This pattern of mild sprain will heal in an uneventful fashion. In the modified Geissler classification, this injury pattern would be considered a grade 0 lesion (Figure 11.4A).
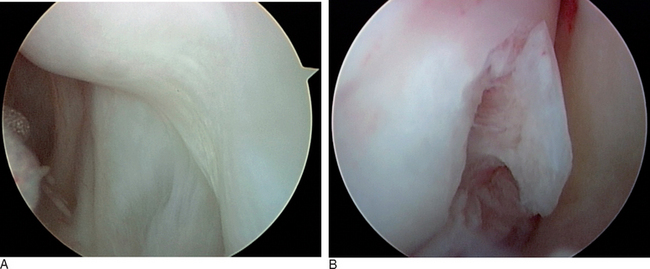
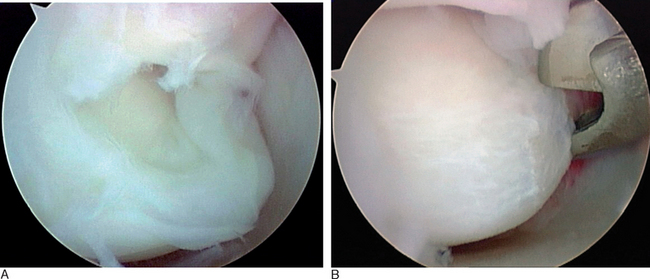
The second pattern within the Geissler grade I classification consists of a partial or full substance, incomplete, subtotal tear of the LTIL. There is no attenuation of the ligamentous fibers, nor any altered carpal kinetics or kinematics. The LTJ remains stable because the integrity of the ligament is maintained (Figure 11.5). This would be a grade I lesion in the modified classication. The mechanical irritation to the wrist joint caused by the tearing of the ligamentous fibers results in pain.
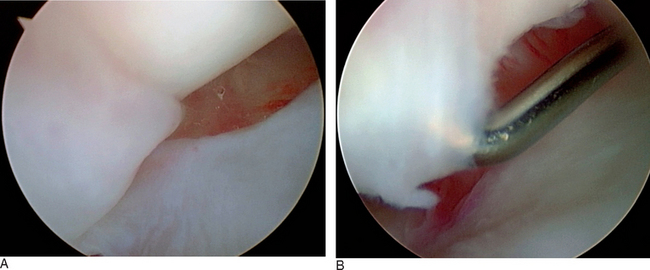
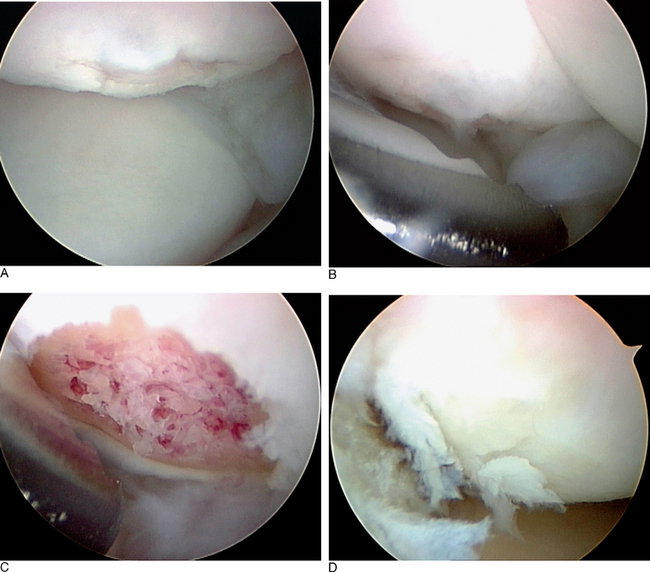
When attenuation of the ligament is arthroscopically observable, this is a much more serious finding and has more serious consequences for both outcome and treatment of these injuries. Attenuation of the LTIL indicates that its fibers have been sprained or stretched beyond their plastic limit, and consequently the basic integrity of the ligament has been compromised. Arthroscopically, the attenuated LTIL appears lax or loose or wavy—but morphologically it remains basically intact and still physically connects the lunate to the triquetrum. Frequently, partial or full substance incomplete tears are present—but it is possible to have ligamentous attenuation without any tearing whatsoever (Figure 11.6).
When palpated by the intra-articular probe, the ligamentous fibers are clearly loose. In the acute stage of injury, an attenuated LTIL has the potential to produce laxity or an early stage of instability that could be considered predynamic in the sense that further instability develops with time and additional joint loading. As the injury becomes chronic, cyclic loading of the attenuated LTIL can lead to dynamic and possibly static LTJ instability. In the modified classification, a grade II interosseous ligament injury is a slight sprain of the LTIL with arthroscopically observable attenuation or laxity of the LTIL, no complete disruption of the volar and dorsal ligamentous fibers, and the potential for predynamic or early dynamic instability of the LTJ as evidenced by excessive LTJ movement (i.e., altered kinematics) or early chondromalacia at the joint line (i.e., altered kinetics). Probing usually reveals a complete central membranous tear with stretching of the volar and dorsal portions of the LTIL; or a partial or full substance incomplete tear of the ligament (Figure 11.7).
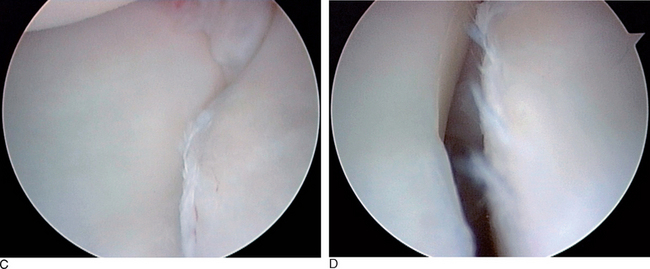
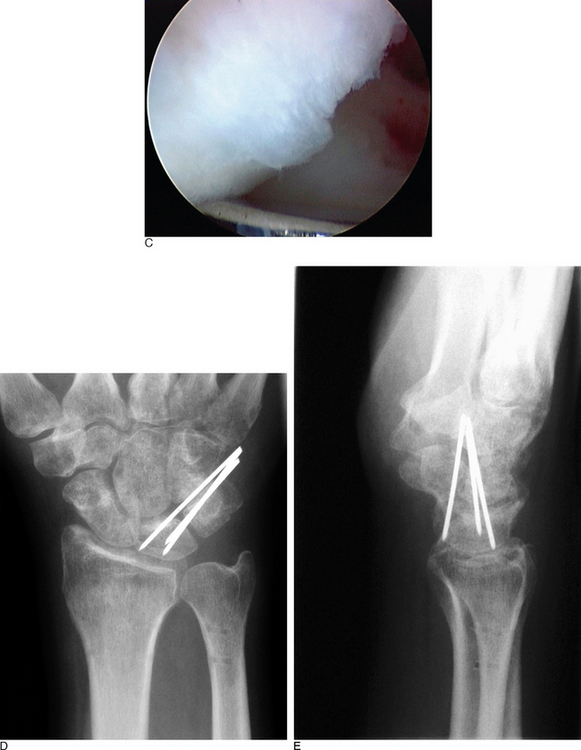
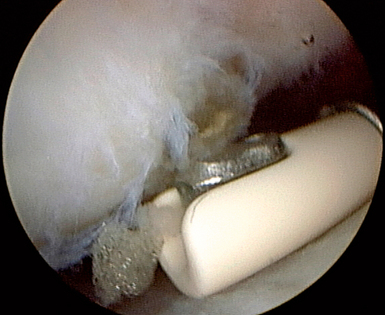
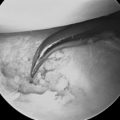
In a Geissler grade III injury of the LTIL, complete disruption of the ligament leads to a dynamically altered relationship between the lunate and the triquetrum. Arthroscopically, an intra-articular probe can be easily passed through the LTJ—revealing an excessive abnormal carpal movement, as seen in the MCJ and often in the RCJ. There is usually much more scar tissue built up in the ulnar aspect of the RCJ adjacent to the LTJ, which is often accompanied by excessive synovitis in the RCJ and MCJ. A diastasis of the LTJ is not seen, and there is no static instability. The LTJ can be reduced with simple manipulation of the lunate and triquetrum. A VISI deformity is not present. The arthroscope cannot be passed through the LTJ because the small gap produced by the instability is not sufficient to allow this to occur (Figure 11.8). This pattern corresponds to a severe ligamentous sprain, and to a grade III interosseous ligament injury.
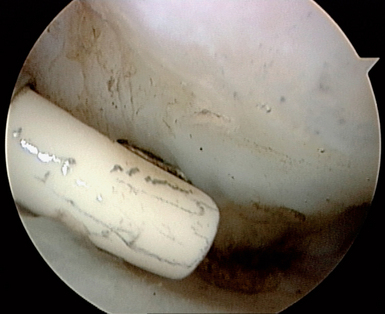
A grade IV injury in both classifications results from a complete disruption of the LTIL, with a static or stress-induced diastasis of the LTJ such that the arthroscope can be passed easily through the wide gap between lunate and triquetrum (Figure 11.9). The secondary ligamentous constraints (i.e., the extrinsic ligaments) are injured, and a CID pattern that usually results in VISI is present (Figure 11.10).
Arthroscopic evaluation of the sprained wrist provides the treating physician with the unique capability to directly examine the full extent of the internal pathologic process. A thorough visual examination of both the RCJ and MCJ will directly define the nature and extent of not only the ligamentous injury but significant associated osseous, cartilaginous, and fibrocartilaginous injuries.35,36,38–40,42,61,62
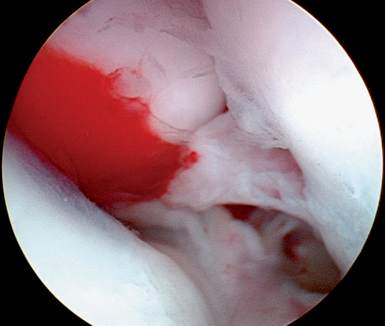
In the ulnar aspect of the RCJ, it is common to find a significant buildup of dorsal capsular scar tissue that forms from the original traumatic injury to the LTIL (Figure 11.11). This scar tissue must be debrided to fully visualize the three regions of the LTIL, the proximal cartilaginous surfaces of the lunate and triquetrum, the TFCC, the ulnocarpal ligaments, and the DRCL. If the LTJ instability is chronic, it is important to assess the ulnar aspect of the carpus for signs of UIS (Figure 11.12). If degeneration of the TFCC or cartilage is present, consideration should be given to formally treating the UIS in addition to treating the LTJ instability.23,24,60
The diagnostic role of arthroscopy in the MCJ is to search out additional cartilaginous and ligamentous pathology.63 Degeneration of the cartilage on the proximal poles of the capitate and hamate, and the distal articular surfaces of the lunate and triquetrum, may be present (Figure 11.13). LTJ instability may occur in conjunction with midcarpal instability.64 MCJ arthroscopy allows for examination of the intrinsic ligaments of the MCJ, especially the THL and TCL. Technically, these two ligaments are difficult to visualize because of the narrow constraints of the triquetrohamate articulation.
If the midcarpal ligaments have been injured, altered joint kinetics and kinematics should be evident (Figure 11.7D). The degree of instability can be assessed and classified as previously described. The arthroscopic findings of MCJ arthritis or instability enable the treating physician to alter the therapeutic intervention. Without the beneficial role of arthroscopy, there would be no reliable nonsurgical diagnostic modality to assist with classification of the CI or to aid in the discovery of ancillary pathology that would alter the treatment plan.
Author’s Preferred Treatment
Acute ulnar-sided wrist pain suspected to have originated from an LTIL injury and that has not responded to conservative care after six weeks of treatment (and certainly by three months) should be evaluated arthroscopically. Likewise, if an MRI has been obtained and is suggestive or diagnostic of an ulnar-sided internal derangement one should proceed to arthroscopy. The wrist arthroscopy will provide valuable information unobtainable via any other diagnostic or imaging source. Arthroscopy of both the RCJ and MCJ will allow for a thorough evaluation of the LTIL, and the extent of LTJ instability. The modified classification scheme provides a helpful guide in choosing an appropriate technique for therapeutic intervention.
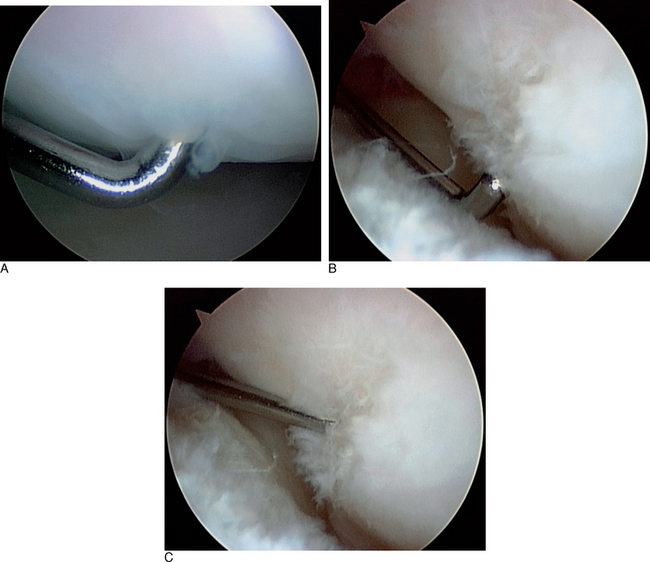
Grade 0 LTJ instability is a stable ligamentous injury that should be expected to heal with wrist immobilization (Figure 11.4A). The prognosis of successful resolution of the wrist pain associated with the mild to slight sprain is excellent. Grade I LTJ instability reveals an intact LTIL with no attenuation of its fibers. There may be an incomplete partial or small full substance tear. There is no increased carpal movement between the lunate and triquetrum. The LTJ is congruent, and no altered carpal kinetics or kinematics is present during the diagnostic arthroscopy (Figure 11.5). If a small ligamentous tear is present, it should be debrided utilizing a full-radius arthroscopic shaver, suction punch, or electrothermal device (Figures 11.8B and 11.14). The wrist is immobilized for four to six weeks in a supportive splint. The prognosis of a successful outcome is excellent.
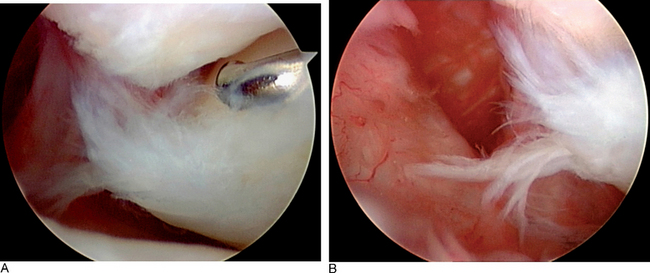
Grade II LTJ instability is characterized by significant attenuation of the LTIL. Often a partial or full substance incomplete tear of the palmar and/or dorsal portions of the LTIL is present. More frequently, there is a complete central membranous tear associated with stretching of the volar and dorsal portions of the LTIL (Figures 11.6 and 11.7). A predynamic instability characterized by cartilage wear and possible increased LTJ motion may be seen in the MCJ. Usually there is excessive scar tissue built up in the dorsoulnar aspect of the carpus, with synovitis (Figure 11.11). This injury pattern has the potential to lead to progression of cartilage degeneration and chronic pain. This specific injury pattern has not been adequately addressed in the literature. Treatment options would include further wrist joint immobilization, debridement of the torn interosseous ligament, ligamentous shrinkage utilizing a radiofrequency probe, LTJ percutaneous K-wire pinning for eight weeks, or a combination of these techniques.
An arthroscopic debridement of the torn LTIL flap should be done to eliminate any mechanical source of joint irritability (Figure 11.8B). Several studies suggest that a debridement of the flap tear alone will produce satisfactory outcomes.35,36,39,40 Only one very small study contradicted this finding.37 Some authors also suggest reduction of the LTJ and percutaneous K-wire pinning for approximately eight weeks20,35,38,48,49 (Figure 11.15 and Figure 11.8D and E). Electrothermal ligamentous shrinkage can be performed with either a radiofrequency probe or a laser64–67 (Figure 11.16). This relatively new technology can be applied to an attenuated LTIL, or even to the ulnocarpal extrinsic ligaments.
Biomechanically, the tensile strength of the heated collagen within the ligament decreases and does not return to normal for approximately 12 weeks. Therefore, it is important to immobilize the wrist for at least 8 weeks, and to avoid any heavy activity for 12 weeks.66 Frequently, an excessive amount of dorsal capsular scar tissue is present in the dorsoulnar section of the RCJ. This scar tissue inhibits full visualization of the ulnar-sided wrist structures and should be arthroscopically debrided (Figure 11.11).
Grade III LTIL injury reveals a complete tear of the LTIL (Figure 11.8). The LTJ is clearly unstable when a force is applied, but the joint is anatomically reducible. A static LTJ diastasis is not present, and injury to the secondary restraint extrinsic ligaments is not seen. A probe can be passed through the small gap present between the lunate and the triquetrum. The author recently reviewed a series of 40 patients with a grade III injury who were treated with arthroscopic debridement of the torn LTIL, arthroscopic reduction of the LTJ, and percutaneous K-wire fixation for 8 to 10 weeks.
An alternative arthroscopic surgical procedure would be a ligament plication of the ulnocarpal ligaments and pinning of the LTJ. Early results with this technique of arthroscopic plication have been promising.57 A tenodesis of the LTJ using a distally based segment of the ECU tendon has been successful in a recent report.58 The author does not have any direct experience with either of these surgical techniques.
Acute grade IV LTIL injuries present with a severe alteration of carpal alignment, incongruency of the LTJ, and gross instability (Figure 11.10). It is possible to manage these with an ARIF before a fixed VISI occurs. If the LTJ is arthroscopically reducible, it may be pinned. The triquetrum should also be pinned to the hamate to maintain its anatomical alignment between the distal radius and ulna, and the distal carpal row to allow for healing of the torn extrinsic ligaments. Cast and pin immobilization should continue for a minimum of eight weeks. The author has had some success with this technique of ARIF, even as long as one year following LTIL injury.
1 Patterson RM, Nicodemus CL, Viegas SF. High-speed, three-dimensional kinematic analysis of the normal wrist. J Hand Surg. 1998;23:446-453.
2 Berger RA. General anatomy. In: Cooney WP, Linsheid RL, Dobyns JH, editors. The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.
3 Garcia-Elias M, Dobyns JH. Bones and joints. In: Cooney WP, Dobyns RL, Dobyns JH, editors. The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.
4 Berger RA. Ligament anatomy. In: Cooney WP, Linsheid RL, Dobyns JH, editors. The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.
5 Mastella DJ, Zelouf DS. Anatomy of the lunotriquetral joint. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
6 Ritt MJ, Bishop AT, Berger RA, et al. Lunotriquetral ligament properties: A comparison of three anatomic subregions. J Hand Surg. 1998;23:425-431.
7 The Anatomy and Biomechanics Committee of the International Federation of Societies for Surgery of the Hand. Position statement: Definition of carpal instability. J Hand Surg. 1999;24:866-867.
8 Linscheid RL, Dobyns JH, Beabout JW, et al. Traumatic instability of the wrist: Diagnosis, classification and pathomechanics. J Bone Joint Surg. 1972;54:1612-1632.
9 Mayfield JK, Johnson RP, Kilcoyne RK. Pathomechanics and progressive perilunar instability. J Hand Surg. 1980;5:226-241.
10 Reagan DA, Linsheid RL, Dobyns JH. Lunotriquetral sprains. J Hand Surg. 1984;9:502-514.
11 Lichtman DM, Schneider JR, Swafford AR, et al. Ulnar midcarpal instability: Clinical and laboratory analysis. J Hand Surg. 1981;6:515-523.
12 Freeland AE, Geissler WB. Kinematics and pathophysiology of carpal instability. In: Geissler WB, editor. Wrist Arthroscopy. New York: Springer, 2005.
13 Weber ER. Wrist mechanics and its association with ligamentous instability. In: Lichtman DM, Alexander AH, editors. The Wrist and Its Disorders. Philadelphia: W.B. Saunders, 1988.
14 Trumble TE, Bour CJ, Smith RJ, et al. Kinematics of the ulnar carpus related to the volar intercalated segment instability pattern. J Hand Surg. 1990;15:384-392.
15 Viegas SF, Patterson RM, Peterson PD, et al. Ulnar-sided perilunate instability: An anatomic and biomechanic study. J Hand Surg. 1990;15:268-278.
16 Horii E, Garcia-Elias M, An KN, et al. A kinematic study of luno-triquetral dissociations. J Hand Surg. 1991;16:355-362.
17 Ritt MJ, Linsheid RL, Cooney WP, et al. The lunotriquetral joint: Kinematic effects of sequential ligament sectioning, ligament repair, and arthrodesis. J Hand Surg. 1998;23:432-445.
18 Garcia-Elias M, Ritt JP. Lunotriquetral dissociation: Pathomechanics. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
19 Bednar JM, Osterman AL. Carpal instability: Evaluation and treatment. J Am Acad Orthop Surg. 1993;1:10-17.
20 Butterfield WL, Joshi AB, Lichtman DM. Lunotriquetral injuries. J Am Soc Hand Surg. 2002;2:195-203.
21 Moran SL, Shin AY. Open treatment options for lunotriquetral instability and dissociation. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
22 Bindra DS, Slade JFIII. Lunotriquetral arthritis and ulnar impaction syndrome. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
23 Hanker GJ. Arthroscopic management of ulnar impaction syndrome. In: Geissler WB, editor. Techniques in Wrist Arthroscopy. New York: Springer-Verlag, 2003.
24 Hanker GJ. Arthroscopic management of ulnar impaction syndrome. In: Geissler WB, editor. Wrist Arthroscopy. New York: Springer, 2005.
25 Dobyns JH, Cooney WP. Classification of carpal instability. In: Cooney WP, Linsheid RL, Dobyns JH, editors. The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.
26 Shin AY, Battaglia MJ, Bishop AT. Lunotriquetral instability: Diagnosis and treatment. J Am Acad Orthop Surg. 2000;8:170-179.
27 Kalainov DM, Hartigan BJ, Cohen MS. Lunotriquetral instability: Clinical findings. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
28 Atzei A, Luchetti R. Clinical approach to the painful wrist. In: Geissler WB, editor. Wrist Arthroscopy. New York: Springer, 2005.
29 Michalko K, Allen S, Akelman E. Evaluation of the painful wrist. In: Geissler WB, editor. Wrist Arthroscopy. New York: Springer, 2005.
30 Cooney WP, Berger RA. Interosseous ligamentous injuries of the wrist. In McGinty JB, editor: Operative Arthroscopy, Third Edition, Philadelphia: Lippincott Williams and Wilkins, 2003.
31 Bishop AT, Reagon DA. Lunotriquetral sprains. In: Cooney WP, Linsheid RL, Dobyns JH, editors. The Wrist: Diagnosis and Operative Treatment. St. Louis: Mosby, 1998.
32 Cassidy C, Ruby LK. Carpal instability. Instr Course Lect. 2003;52:209-220.
33 Pillukat T, Van Schoonhoven J, Lanz U. Ulnar instability of the carpus. Orthopade. 2004;33(6):676-684.
34 Bottcher R, Mutze S, Lautenbach M, et al. Diagnosis of lunotriquetral instability. Handchir Mikrochir Plast Chir. 2005;37(2):131-136.
35 Ritter MR, Chang DS, Ruch DS. The role of arthroscopy in the treatment of lunotriquetral ligament injuries. Hand Clin. 1999;15(3):445-454.
36 Ruch DS, Bowling J. Arthroscopic assessment of carpal instability. Arthroscopy. 1998;14(7):675-681.
37 Westkaemper JG, Mitsionis G, Giannakopoulos PN. Wrist arthroscopy for the treatment of ligament and triangular fibrocartilage complex injuries. Arthroscopy. 1998;14:479-483.
38 Osterman AL, Seidman GD. The role of arthroscopy in the treatment of lunotriquetral ligament injuries. Hand Clin. 1995;11:41-50.
39 Ruch DS, Poehling GG. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg. 1996;21:412-417.
40 Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg. 1997;22:344-349.
41 Geissler WB, Freeland A, Savoie FHIII, et al. Intraarticular soft-tissue lesions associated with an intraarticular fracture of the distal end of the radius. J Bone Joint Surg. 1996;78:357-365.
42 Gupta R, Bozentka DJ, Osterman AL. Wrist arthroscopy: Principles and clinical applications. J Am Acad Orthop Surg. 2001;9:200-209.
43 Palmer AK, Dobyns JH, Linsheid RL. Management of post-traumatic instability of the wrist secondary to ligament rupture. J Hand Surg. 1978;3:507-532.
44 Shin A, Weinstein L, Berger R, et al. Treatment of isolated injuries of the lunotriquetral ligament. J Bone Joint Surg. 2001;83:1023-1028.
45 Watson HK, Black DM. Instabilities of the wrist. Hand Clin. 1987;3:103-111.
46 Kirschenbaum D, Coyle M, Leddy J. Chronic lunotriquetral instability: Diagnosis and treatment. J Hand Surg. 1993;18:1107-1112.
47 Pin P, Young V, Gilula L, et al. Management of chronic lunotriquetral ligament tears. J Hand Surg. 1989;14:77-83.
48 Alexander CE, Lichtman DM. Triquetrolunate instability. In Lichtman DM, Alexander AH, editors: The Wrist and Its Disorders, Second Edition, Philadelphia: W.B. Saunders, 1997.
49 Whipple TL. Intrinsic ligaments and carpal instability. In Arthroscopic Surgery: The Wrist. Philadelphia: J.B. Lippincott; 1992.
50 Schadel-Hopfner M. Therapy of acute triquetrum fractures and LT ligament injuries. Kongressbd Dtsch Ges Chir Kongr. 2001;118:395-398.
51 Nelson D, Manske P, Pruitt D, et al. Lunotriquetral arthrodesis. J Hand Surg. 1993;18:1113-1120.
52 Sennwald GR, Fischer M, Mondi P. Lunotriquetral arthrodesis: A controversial procedure. J Hand Surg [Br]. 1995;20:755-760.
53 Trumble T, Bour C, Smith R, et al. Intercarpal arthrodesis for static and dynamic volar intercalated segment instability. J Hand Surg. 1988;13:384-390.
54 Guidera PM, Watson HK, Dwyer TA, et al. Lunotriquetral arthrodesis using cancellous bone graft. J Hand Surg. 2001;26:422-436.
55 Novak V, Weisler EA. Lunotriquetral arthrodesis. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
56 De Smet L, Janssens I, van de Sande W. Chronic lunotriquetral ligament injuries: Arthrodesis or capsulodesis. Acta Chir Belg. 2005;105(1):79-81.
57 Moskal MJ, Savoie FHIII. Management of lunotriquetral instability. In: Geissler WB, editor. Wrist Arthroscopy. New York: Springer, 2005.
58 Shahane SA, Trail IA, Takwale VJ, et al. Tenodesis of the extensor carpi ulnaris for chronic, post-traumatic lunotriquetral instability. J Bone Joint Surg Br. 2005;87(11):1512-1515.
59 Smith B, Short W, Werner F, et al. The effect of ulnar shortening on lunotriquetral motion and instability: A biomechanical study. Presented at the American Society for Surgery of the Hand, Annual Fellow and Residents Meeting 1994.
60 Geissler WB. Combined lunotriquetral and triangular fibrocartilage complex ligamentous injuries. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
61 Hofmeister EP, Dao KD, Glowacki KA, et al. The role of midcarpal arthroscopy in the diagnosis of disorders of the wrist. J Hand Surg. 2001;26:407-414.
62 Hanker GJ. The role of wrist arthroscopy in the diagnosis and treatment of lunotriquetral joint injuries. In: Ruch DS, editor. Atlas of the Hand Clinics. Philadelphia: W.B. Saunders, 2004.
63 Dautel G, Merle M. Chondral lesions of the midcarpal joint. Arthroscopy. 1997;13:97-102.
64 Sweet A, Weiss L. Applications of electrothermal shrinkage in wrist arthroscopy. Atlas Hand Clin. 2001;6(2):203-210.
65 Frostick SP. Thermal capsulorrhaphy: Basic science. In McGinty J, editor: Operative Arthroscopy, Third Edition, Philadelphia: Lippincott Williams and Wilkins, 2003.
66 Nagle DJ. Lasers and electrothermal devices. In: Geissler WB, editor. Wrist Arthroscopy. New York: Springer, 2005.
67 Darlis NA, Weiser RW, Sotereanos DG. Partial scapholunate ligament injuries treated with arthroscopic debridement and thermal shrinkage. J Hand Surg. 2005;30:908-914.