CHAPTER 17 Arthroscopic Treatment of Elbow Fractures
TREATMENT
Indications and Contraindications
Arthroscopic management of elbow fractures is a rapidly evolving indication for the use of elbow arthroscopy in the identification and treatment of intra-articular pathology. The technique provides for a minimally invasive surgical exposure, minimizing further soft tissue trauma in a region notorious for wound complications. Arthroscopic débridement of fibrinous and osseous debris facilitates postoperative elbow range of motion. Visualization of fracture fragments and chondral injuries is often superior to that achieved with open approaches, and it minimizes the requirements for intraoperative fluoroscopy. Identification of intra-articular pathology not evident on preoperative imaging enables appropriate treatment measures and a more accurate prognosis. Elbow arthroscopy can be used in combination with indirect reduction techniques to maximize articular congruity, or it can be used for direct arthroscopic reduction with fixation devices passed into the joint.
Conservative Management
Most intra-articular fractures of the distal humerus can be effectively treated with open reduction and internal fixation (ORIF), and superior results are achieved with this approach compared with skeletal traction or cast immobilization. Khalfayan and colleagues1 concluded that patients with displaced Mason type II radial head fractures who were treated conservatively had more pain, decreased strength, and decreased elbow motion compared with patients treated with open osteosynthesis. Radial head fracture treatment depends on the fracture pattern and displacement and includes early mobilization, ORIF, and resection or prosthetic replacement. Open treatment options for displaced olecranon fractures include tension band wiring, lag screw placement, neutralization plating, and excision with extensor mechanism reconstruction. Capitellar fractures can likewise be excised or stabilized with standard open techniques. Cadaveric research has drawn attention to the important stabilizing role of the coronoid and has provided compelling evidence for surgical management of these fractures in various circumstances.2,3
Arthroscopic Technique
The patient is placed prone or in the lateral decubitus position. The lateral decubitus position typically requires a supportive device to provide arm suspension. With the patient in the prone position, the arm is elevated on a 4-inch padded block with the elbow flexed to 90 degrees over an arm board located at the patient’s side parallel to the table (Fig. 17-1). This method avoids compression of neurovascular structures in the axilla and facilitates medial or lateral access (in case an open procedure becomes necessary) by internal or external rotation of the forearm onto the arm board. The forearm and hand should be wrapped with compressive wrapping material to restrict swelling and fluid extravasation. Intravenous prophylactic antibiotics are routinely administered preoperatively.
Most procedures can be accomplished with the 4.0-mm, 30-degree arthroscopic camera. A 70-degree camera can provide visualization of the capitellum or radial head from a posterior portal when instrumentation is required from the soft spot portal. Graspers with teeth and smooth outer surfaces are preferred to prevent hang-up on soft tissue. A 3.5-mm, full-radius arthroscopic shaver is useful for removal of organized fracture hematoma and debris (Fig. 17-2). Various implants can be used for fixation, contingent on the fracture configuration (discussed later).
After fracture stabilization has been achieved, the surgeon should thoroughly evaluate elbow stability. This can be accomplished with the assistance of fluoroscopy, but it can also be readily assessed arthroscopically. Diagnosis and management of associated ligamentous injuries of the elbow are discussed in Chapters 13 and 14.
Radial Head Fractures
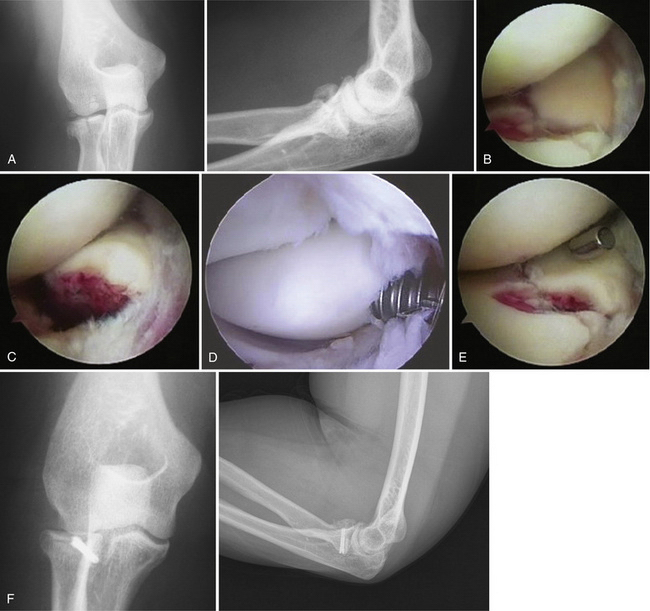
Radial head fractures are the most common type of elbow fracture in adults, and they offer an excellent opportunity for arthroscopic evaluation and management (Fig. 17-3A). In patients with persistent locking and pain despite radiographic evidence of minimally displaced radial head fractures, diagnostic arthroscopy enables accurate assessment of articular cartilage, identification of any osteochondral flaps or loose bodies, and débridement with minimal morbidity. Displaced two-part radial head fractures can be visualized through a proximal anteromedial or posterolateral portal to assess the degree of articular incongruity, fracture fragment stability, and any impingement to forearm rotation. A direct lateral portal can also provide visualization of the posterior aspect of the radial head during confirmation of fracture reduction. If arthroscopic reduction with internal fixation is desired, visualization is best achieved with a 70-degree camera from a posterolateral portal, with instruments and implants introduced through a soft spot portal.
After débridement and lavage, Kirschner wires can be positioned through the anterolateral or soft spot portals in conjunction with arthroscopic probes, graspers, and occasionally, a reduction tenaculum to allow for manipulation, reduction, and provisional fixation of larger fracture fragments. Visualization can often be facilitated by rotating the forearm into maximal supination. Definitive fixation can then be performed using absorbable pins or cannulated screws (see Fig. 17-3D). Herbert-Whipple screws (Zimmer, Inc., Warsaw, IN) and headless variable-pitch screws (Acutrak screws, Acumed, LLC, Hillsboro, OR) are advantageous in providing secure fixation with compression to allow early motion, while being buried beneath the articular surface to avoid impingement. Reduction and stability of the fixation can be directly assessed during full rotation of the elbow (see Fig. 17-3E).
Rolla and colleagues4 reported preliminary results for six patients who underwent arthroscopic reduction and internal fixation for radial head fractures classified as Mason5 type II (3), type III (2), or type IV (1). All patients returned to their preinjury level of function within 6 months. The Mayo Elbow Performance (MEP) scores were excellent for three and good for the other three patients at mean follow-up of 12 months.
Michels and associates6 presented longer-term results of an arthroscopic technique for treatment of Mason type II radial head fractures in 14 patients. The MEP scores were excellent for 11 and good for the other 3 patients at a mean follow-up of 5 years 6 months. The procedure was refined to the use of only a midlateral viewing portal and an anterolateral working portal. A potential advantage of this arthroscopic technique was the observation that a single screw was usually sufficient to obtain stability. The investigators concluded that the capsular dissection required by an open technique might increase fracture fragment instability, resulting in the requirement for additional fixation.
Dawson and Inostroza7 have published a case report in which they described a technique of arthroscopic reduction and percutaneous pinning to treat an angulated radial neck fracture, an entity encountered in the developing elbow and occurring most commonly in patients between 9 and 13 years old. The fracture is reduced through an anterolateral portal with a hemostatic forceps while a Kirschner wire is percutaneously inserted to obtain fixation of the radial head to the diaphysis. A cast is applied for 3 weeks, and the Kirschner wire is then removed.
Arthroscopic excision of acute radial head fractures should not be performed in high-demand patients or when the fracture is associated with instability. Radial head resection in the setting of post-traumatic arthritis of radial head fractures remains controversial. If conservative or primary surgical treatment results in an unsatisfactory clinical outcome, delayed radial head excision is an effective option. Broberg and Morrey8 documented significant relief of pain and recovery of motion with late resection of the radial head after nonoperative treatment of Mason type II and III fractures in a review of 21 patients.
Menth-Chiari and colleagues9,10 demonstrated similar positive benefits for delayed radial head resection by an arthroscopic technique in a mixed series that included 10 patients with post-traumatic arthritis after type II and III fractures. The procedure begins with a partial resection of the anterior three fourths of the radial head and 2 to 3 mm of radial neck using a hooded abrader in the anterolateral portal and the arthroscope in the proximal medial portal. The abrader is then transferred to the mediolateral portal to complete the resection. No subjective or objective evidence of instability was documented in this series. The surgeons advocated that preservation of the annular ligament complex should be an important consideration in maintaining the stability at the proximal radioulnar joint.
Coronoid Fractures
Operative intervention for coronoid process fractures is recommended for Regan and Morrey11 type III fractures and any type of fracture that interferes with joint motion. When comminution precludes fixation, loose debris can be removed arthroscopically. However, larger coronoid fractures can be effectively treated with the use of arthroscopic reduction techniques. The fracture can be manipulated into reduction by a tibial anterior cruciate ligament guide inserted through the anteromedial portal while viewing through a lateral portal (Fig. 17-4).12 A guide pin can then be drilled through the ulnar shaft to engage the fragment, followed by definitive fixation with a small, cannulated screw placed in antegrade fashion. Fragments that are too small for screw fixation can be stabilized with the application of suture anchors placed within the base of the fracture. A hinged brace or external fixator may be necessary to maintain joint stability and offload the repair until adequate healing has occurred.
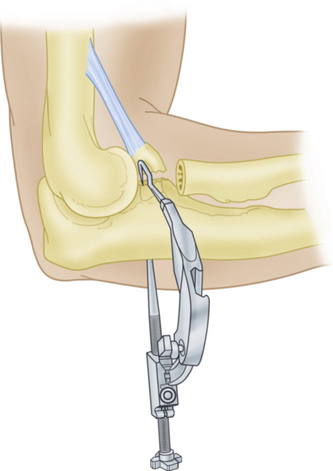
FIGURE 17-4 An anterior cruciate ligament guide is used for coronoid fractures.
(Modified from Adams JE, Merten SM, Steinmann SP. Arthroscopic-assisted treatment of coronoid fractures. Arthroscopy. 2007;23:1060-1065.)
Lui and coworkers13 described successful arthroscopic outcomes in two athletes with type I coronoid fractures after initial conservative management had failed. Treatment consisted of excision of loose bodies in one patient and excision of a fibrous nonunion in the other. Adams and colleagues12 reported their experience with arthroscopically assisted reduction and fixation of four type II and three type III coronoid fractures. Cannulated screw fixation was achieved antegrade over pins placed with the use of an anterior cruciate ligament guide. The surgeons observed that all five of the patients available for follow-up at an average 2 years and 8 months had MEP scores of 100%.
Capitellar and Coronal Shear Fractures
Capitellar fractures account for less than 1% of all elbow fractures. They are divided into type I (i.e., Hahn-Steinthal fragment), type II (i.e., Kocher-Lorenz fragment), and type III (i.e., markedly comminuted) fractures (Fig. 17-5A).14 However, a high incidence of osteochondral capitellar defects has been associated with radial head fractures. Types I and II capitellar and coronal shear fractures can be treated with an antegrade arthroscopically assisted technique similar to that used for coronoid fractures (see Fig. 17-5B). Alternatively, provisional reduction can be carried out in a retrograde fashion with Kirschner wires, followed by cannulated screw fixation (see Fig. 17-5C). The anterolateral portal can provide access for bioabsorbable pin fixation of Kocher-Lorenz fragments and reparable osteochondral flaps considered too fragile for screw fixation. Osteochondral defects that are not reparable should be arthroscopically débrided.15
A 70-degree camera introduced through a posterior portal may provide the optimum view of the capitellum when instrumenting from the soft spot portal. Alternatively, Hardy and colleagues16 found that the proximal lateral portal provided effective visualization in a case report in which a type I fracture was reduced by manipulating the fragment through an anterolateral working portal. Reduction required traction through the axis of the forearm with the elbow flexed at 30 degrees. The surgeon may consider partial release of the lateral collateral ligament to facilitate visualization and reduction of shear-type fractures. Repair can be later achieved arthroscopically with a suture anchor.
Lateral Condylar Fractures
Fractures of the lateral humeral condyle represent approximately 15% of elbow fractures in the pediatric population.17 To ensure articular congruity, these fractures historically have been treated with a closed reduction with arthrography or an open lateral Kocher approach for displaced fractures. Milch type I and II fractures are often amenable to arthroscopic evaluation and arthroscopically assisted percutaneous screw or pin fixation. Arthroscopic reduction has the advantage of avoiding the elevation of the capsulosynovial and periosteal attachments that may occur during a Kocher approach, potentially reducing the risk of compromise to the vasculature of the distal fragment that may lead to avascular necrosis and cubitus valgus deformity.
Hausman and associates18 retrospectively reviewed their results from arthroscopically assisted treatment of six pediatric lateral condyle fractures. Standard anteromedial and anterolateral portals were used. The fracture fragment was reduced under direct visualization with the assistance of percutaneous 0.062-inch Kirschner wire joysticks, including a Kirschner wire placed transversely through the axis of the capitellum to facilitate rotational control of the reduction. The Kirschner wire fixation was maintained for 4 weeks postoperatively in a long arm cast. Although the mean follow-up was only 32 weeks, all patients achieved full active range of motion with no radiographic evidence of nonunion or malunion. Perez Carro and coworkers19 described similar results in their series of four patients.
Intercondylar and Supracondylar Fractures
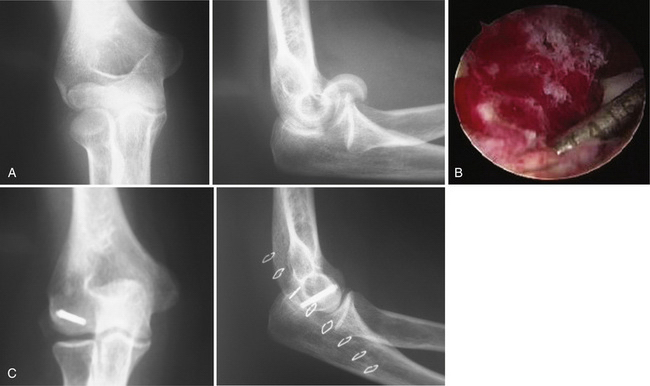
Intercondylar and supracondylar fractures usually require open reduction with plate fixation. Of the three AO North America group C classification subtypes, only the C1 type is amenable to arthroscopically assisted reduction with percutaneous fixation as previously described (Fig. 17-6A and B). Kirschner wires are drilled from a medial to lateral direction to reduce and provisionally secure each condyle. Wires are then drilled proximally into each column to secure this construct to the distal humerus.
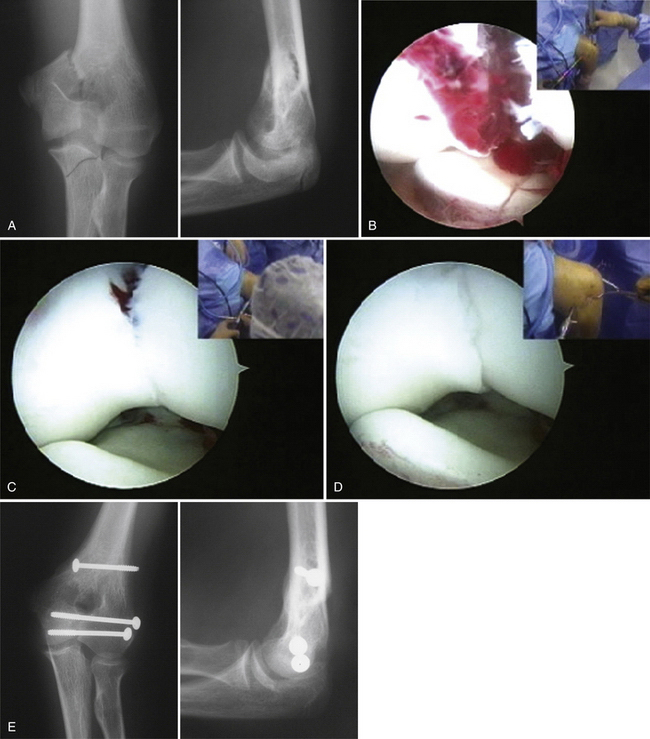
FIGURE 17-6 Unicondylar humerus fractures may represent an indication for elbow arthroscopy. A, The radiographs reveal a supracondylar-intercondylar humerus fracture, which was sustained by a 14-year-old boy. B, Arthroscopic views of the fracture demonstrate the displacement of the fragments and the separation of the humerus from the underlying coronoid and olecranon processes of the ulna. C, The initial reduction was obtained using Kirschner wire joysticks and a fracture clamp placed percutaneously. D, The final reduction is observed after multiple screw placements to stabilize the fracture. E, Final radiographs demonstrate stable internal fixation.
Arthroscopic evaluation must confirm anatomic reduction anteriorly and posteriorly before definitive screw fixation is performed (see Fig. 17-6C through E). Single-column screw fixation limits this technique to individuals with bone quality sufficient to allow for early, protected motion. Visualization can be augmented with an arthroscopic triceps reflection, if necessary. A retractor strategically placed through a superior portal can be used to lift the triceps and facilitate the exposure.
Principles of Arthroscopic Fracture Management of the Elbow
Principal 5: Know the limits. A surgeon must make a realistic appraisal of the technical demands imposed by each case and be especially cognizant of time constraints with regard to fluid extravasation and tourniquet use. A good strategy is to enforce time limits set at the beginning of a case. The use of limited incisions should be considered in preoperative planning, and conversion to conventional open techniques should take precedence over arthroscopic measures whenever the principles of fracture management require.
PEARLS& PITFALLS
PEARLS
PITFALLS
Postoperative Rehabilitation
A light compressive dressing in applied, and gentle, protected range of motion is encouraged on the first postoperative day. The rehabilitation process is coordinated by the surgeon and depends on the fracture pattern. Passive activities are encouraged, and resisted exercises are avoided for a minimum of 6 weeks. A passive motion machine may be of some benefit if the patient is unable to comply with the rehabilitation protocols. A hinged brace may be used within designated motion guidelines when concern for stability and protection of the soft tissues is warranted. Union is assessed radiographically at 6 to 8 weeks or sooner, depending on concern regarding stability of the fixation.
1. Khalfayan EE, Culp RW, Alexander AH. Mason type II radial head fractures: operative versus nonoperative treatment. J Orthop Trauma. 1992;6:283-289.
2. Closkey RF, Goode JR, Kirschenbaum D, Cody RP. The role of the coronoid process in elbow stability: a biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000;82:1749-1753.
3. Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg Am. 2004;86:975-982.
4. Rolla PR, Surace MF, Bini A, Pilato G. Arthroscopic treatment of fractures of the radial head. Arthroscopy. 2006;22:233 e1-233 e6.
5. Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123-132.
6. Michels F, Pouliart N, Handelberg F. Arthroscopic management of Mason type 2 radial head fractures. Knee Surg Sports Traumatol Arthrosc. 2007;15:1244-1250.
7. Dawson FA, Inostroza F. Arthroscopic reduction and percutaneous fixation of a radial neck fracture in a child. Arthroscopy. 2004;20(suppl 2):90-93.
8. Broberg MA, Morrey BF. Results of delayed excision of the radial head after fracture. J Bone Joint Surg Am. 1986;68:669-674.
9. Menth-Chiari WA, Poehling GG, Ruch DS. Arthroscopic resection of the radial head. Arthroscopy. 1999;15:226-230.
10. Menth-Chiari WA, Ruch DS, Poehling GG. Arthroscopic excision of the radial head: clinical outcome in 12 patients with post-traumatic arthritis after fracture of the radial head or rheumatoid arthritis. Arthroscopy. 2001;17:918-923.
11. Regan W, Morrey B. Fractures of the coronoid process of the ulna. J Bone Joint Surg Am. 1989;71:1348-1354.
12. Adams JE, Merten SM, Steinmann SP. Arthroscopic-assisted treatment of coronoid fractures. Arthroscopy. 2007;23:1060-1065.
13. Liu SH, Henry M, Bowen R. Complications of type I coronoid fractures in competitive athletes: report of two cases and review of the literature. J Shoulder Elbow Surg. 1996;5:223-227.
14. Bryan RS, Morrey BF. Fractures of the distal humerus. In: Morrey BF, editor. The Elbow and Its Disorders. Philadelphia, PA: WB Saunders; 1985:302-309.
15. Feldman MD. Arthroscopic excision of type II capitellar fractures. Arthroscopy. 1997;13:743-748.
16. Hardy P, Menguy F, Guillot S. Arthroscopic treatment of capitellum fracture of the humerus. Arthroscopy. 2002;18:422-426.
17. Milch H. Fractures and fracture dislocations of the humeral condyles. J Trauma. 1964;4:592-607.
18. Hausman MR, Qureshi S, Goldstein R, et al. Arthroscopically assisted treatment of pediatric lateral humeral condyle fractures. J Pediatr Orthop. 2007;27:739-742.
19. Perez Carro L, Golano P, Vega J. Arthroscopic-assisted reduction and percutaneous external fixation of lateral condyle fractures of the humerus. Arthroscopy. 2007;23:1131 e1-1131 e4.
Holt MS, Savoie FH3rd, Field LD, Ramsey JR. Arthroscopic management of elbow trauma. Hand Clin. 2004;20:485-495.
Moskal MJ, Savoie FH3rd, Field LD. Elbow arthroscopy in trauma and reconstruction. Orthop Clin North Am. 1999;30:163-177.
Savoie FH, Peden JP, Field LD. Arthroscopic reduction and internal fixation of elbow fractures. In: Yamaguchi K, King GJW, McKee MD, O’Driscoll SW, editors. Advanced Reconstruction: Elbow. Evanston, IL: American Academy of Orthopaedic Surgeons; 2007:85-92.