CHAPTER 10 Arthroscopic Thermal Shrinkage for Scapholunate Ligament Injuries
Introduction
The use of arthroscopic thermal shrinkage with radiofrequency (RF) for the treatment of scapholunate (SL) ligament injuries is a recent technique, but the real effectiveness is undetermined.1–3 The ability of RF probes to both debride and shrink tissues makes them an attractive alternative to the use of a mechanized resector for debridement of SL ligament tears, and provides a means of stabilizing the SL joint.
What Is Shrinkage?
Shrinkage is a physical phenomenon that occurs with heat modification of type I collagen in ligamentous tissue. When the collagen is heated to a critical temperature, the heat-labile intramolecular hydrogen bonds break.4 The protein undergoes a phase transition from a highly ordered crystalline structure to a random-coil state (similar to a melted state) and the tissue tensile properties change.5 Typically, this thermal denaturation of collagen type I occurs at approximately 60 to 65° C.
Molecular Effects of Thermal Shrinkage
Transmission electron microscopy shows significant alterations in the collagen architecture. These changes are characterized by the loss of the classic 67-nm periodicity of the type I collagen fibril that is evidenced by the loss of the periodical cross-striations in the collagen fibril. There is also an increase in the cross-sectional area of the collagen fibril. The margins of the fibrils begin to lose their distinct edge, while maintaining their circular shape. These ultrastructural effects are caused by unwinding of the collagen triple-helix as a result of the temperature rise in the tissue.6,7
Biologic Response to Thermal Shrinkage
At time 0, after thermal shrinkage there is evidence under light microscopy of diffuse hyalinization and fusion of the collagen fiber. By day 7, there is fibroblast proliferation around and within the hyalinized regions. By day 30, large fibroblasts have migrated into the region and have produced a new matrix. These newly arrived fibroblasts use the acellular “hyalinized” collagen as a scaffold for migration and matrix synthesis. At three months, active reparative changes are evident (with an increase in vascularity). The fibroblasts have now regained a more normal appearance under transmission electron microscopy. At seven months, cell morphology and vascularity have returned to normal—without evidence of permanent tissue injury or severe inflammation.8,9
Biomechanical Effects of Thermal Shrinkage
Experimental studies have shown that (1) ligaments and joint capsular tissue can be modified significantly (shortened) by thermal energy at the temperature range of 70 to 80° C, (2) thermal energy causes immediate deleterious effects such as loss of the mechanical properties, collagen denaturation, and cell necrosis, (3) thermally treated tissue is repaired actively by a residual population of fibroblasts and vascular cells, with concomitant improvement of mechanical properties, (4) the shrunken tissue stretches with time if the tissue is subjected to physiologic loading immediately after surgery, and (5) leaving viable tissue between treated regions significantly improves the healing process.10,11
Rationale for Shrinkage of Scapholunate Ligament Injuries
Our concept for the use of thermal shrinkage for the treatment of instability of the carpus with scapholunate ligament injuries arose from previous published work on the use of thermal shrinkage on other articulations, as well as the favorable results that were achieved following mechanical debridement of partial SL ligament tears.12,13 We were also influenced by the biomechanical importance of the SL ligament for stability of the carpus and the paucity of treatment methods for carpal instability, as well as the relative ease of performing an arthroscopic shrinkage of the SL ligament.
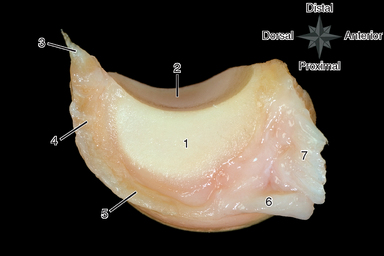
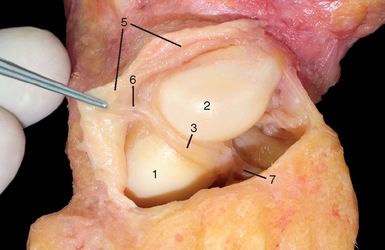
The SL ligament is not a homogeneous structure. It is divided into three parts: dorsal, proximal, and palmar (Figure 10.1). The dorsal part is the strongest subregion of the SL ligament. It meets all criteria for the definition of an articular ligament in that it is composed of collagen fascicles surrounded by connective tissue with intertwined neurovascular bundles.14–16 It has a thickness of 2 to 3 mm and a length of 4 to 5 mm (Figure 10.2), and it merges with the dorsal capsule (Figure 10.3).
The proximal portion is grossly anisotropic. It is composed mainly of fibrocartilaginous tissue, which is relatively weak due to its avascularity. The transition zone between the proximal and palmar portions is marked by the radioscapholunate ligament, which inserts on the palmar aspect of the scapholunate ligament. The palmar portion is composed of thin collagen fascicles (1 mm thick) of length 4 to 5 mm. This portion is not visible through the standard dorsal arthroscopic portals in the face of an intact radioscapholunate ligament.
The three parts do not have the same tensile strength. The dorsal part is most resistant to shear forces, with an ultimate yield strength of 300 N. The palmar part fails at a load of 150 N, whereas the proximal portion can withstand only 25 to 50 N of stress. The triquetrolunate ligament, which is also divided into three parts, has the exact reverse characteristics in regard to loading failure as those of the SL ligament. Biomechanical studies have also demonstrated that the dorsal subregion of the SL ligament is responsible for controlling scaphoid flexion and the extension motion, whereas the palmar subregion controls rotational motion.17–20
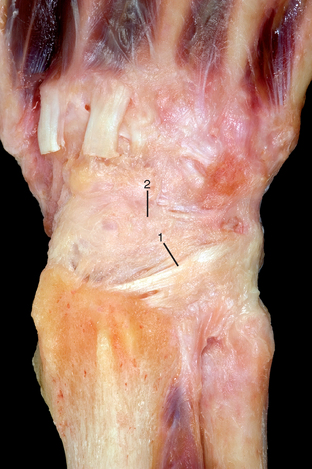
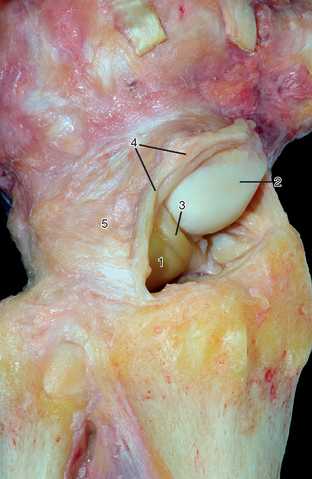
Based on this evidence, it was apparent to us that the use of thermal shrinkage of the SL ligament was feasible and most appropriate for the dorsal part of the ligament. When considering the kinematics and the instability of the carpus in SL ligament injuries, it is important to remember the role of the dorsal radiocarpal ligaments (Figure 10.4) and the dorsal capsule (Figure 10.5). They are initimately connected with the SL ligament and must be included in the thermal shrinkage (Figure 10.6).
The aim of thermal shrinkage of the SL ligaments along with the dorsal ligaments and the dorsal capsule is to maintain the ligament and capsular shortening achieved during shrinkage, while awaiting the secondary fibroplasia and resultant thickening of the joint capsule and ligament. Another theoretical goal is the interruption of any painful afferent sensory pathways through the destruction of sensory receptors.21–23
Technique
The wrist is examined from radial to ulnar, and the stability of the SL interval is assessed by probing the transition zone between the dorsal portion of the SL ligament (which is thick and taut). The weaker proximal portion is identified by palpation. All undergo stress testing of the scapholunate ligament under direct visualization. Any ligamentous injury is classified according to the arthroscopic classification scheme described by Geissler.24 The shrinkage of the SL ligament is performed with a 2.3-mm monopolar RF probe dedicated for shrinkage (Micro-Tacs), includiing an angled tip and a controlled temperature system.
The shrinkage is performed on the entire dorsal section of the ligament (Figures 10.7 through 10.9), extending up to its confluence with the dorsal capsule (Figure 10.10). The palmar subregion of the SL ligament is not included in the shrinkage. The SL ligament and capsular tissue are treated with multiple single linear passes (grid pattern) to leave more viable tissue adjacent to the treated areas, which may result in faster cellular invasion and matrix formation. There is no objective way of measuring the effect of RF probes, and therefore the surgeon relies on visual assessment of the morphologic ligament tissue changes and capsular volume reduction to quantify the degree of tissue shrinkage.
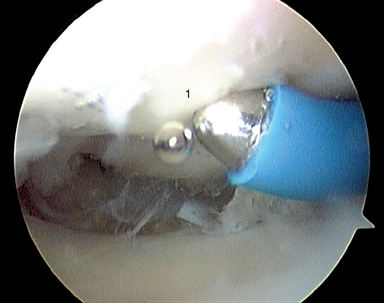
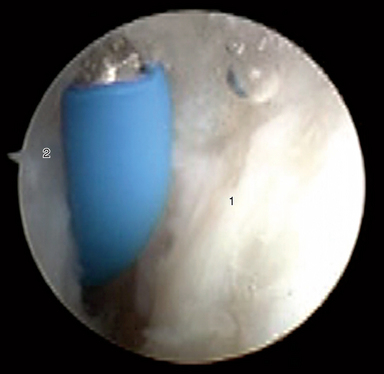
FIGURE 10.7 Arthroscopic photo. (1) SL ligament: shrinkage is performed on the entire dorsal section of the ligament.

FIGURE 10.8 Arthroscopic photo. (1) SL ligament: shrinkage is performed on the entire dorsal section of the ligament.

FIGURE 10.9 Arthroscopic photo. (1) SL ligament: shrinkage is performed on the entire dorsal section of the ligament.

FIGURE 10.10 Arthroscopic photo. The shrinkage is extended up to confluence with the dorsal capsule.
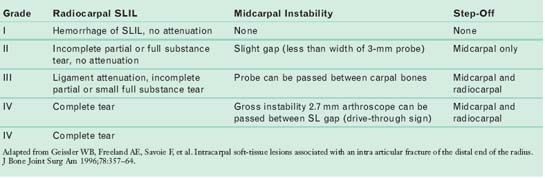
Using the Geissler classification of SL ligament injuries (Table 10.1), symptomatic grade I lesions are treated with the standard technique for shrinkage. Grade II lesions that demonstrate dynamic instability (i.e., an increased scapholunate gap with loading) are treated with shrinkage in addition to Kirschner wire fixation of the scaphoid and lunate.25,26 In grade III lesions (where there is a complete SL ligament perforation), the shrinkage is mainly performed on the dorsal capsule and radiocarpal ligaments—with only marginal shrinkage of the torn dorsal ligament combined with Kirschner wire fixation of the scaphoid and lunate.
Scientific Study
A prospective randomized clinical study was performed to determine the effectiveness of arthroscopic thermal shrinkage with radiofrequency for the treatment of symptomatic SL ligament injuries. From 2001 to 2004, 120 patients with SL ligament injuries were treated. Inclusion criteria consisted of patients with a Geissler grade I, II, or III SL ligament injury associated with dorsoradial wrist pain unresponsive to six to eight weeks of conservative treatment. Patients with DISI deformities on plain X-rays were excluded. The patients were randomized into four treatment groups, as follows.
1 Hirsh L, Sodha S, Bozentka D, Monaghan B, Steinberg D, Beredjiklian PK. Arthroscopic electrothermal collagen shrinkage for symptomatic laxity of the scapholunate interosseous ligament. J Hand Surg. 2005;30B(6):643-647.
2 Darlis NA, Weiser RW, Sotereanos DG. Partial scapholunate ligament injuries treated with arthroscopic debridement and thermal shrinkage. J Hand Surg. 2005;30A:908-914.
3 Shih JT, Lee HM. Monopolar radiofrequency electrothermal shrinkage of the scapholunate ligament arthroscopy. 2006;22(5):553-557.
4 Arnoczky SP, Aksan A. Thermal modification of connective tissues: Basic science considerations and clinical implications. Journal of the American Academy of Orthopaedic Surgery. 2000;5:305-313.
5 Owens BD, Stickles BJ, Busconi BD. Radiofrequency energy: Applications and basic science. Am J Orthop. 2003;32:117-120.
6 Wallace AL, Hollinshead RM, Frank CB. The scientific basis of thermal capsular shrinkage. J Shoulder Elbow Surg. 2000;9:354-360.
7 Medvecky MJ, Ong BC, Rokito AS, Sherman OH. Thermal capsular shrinkage: Basic science and clinical applications. Arthroscopy. 2001;17:624-635.
8 Vangsness CT, Mitchell WIII, Nimni M, Erlich, Saadat V, Schmotzer H. Collagen shortening: An experimental approach with heat. Clin Orthop. 1997;337:267-271.
9 Berger RA, Garcia-Elias M. General anatomy of the wrist. In: Berger RA, Cooney WPIII, editors. Biomechanics of the Wrist Joint. New York: Springer-Verlag; 1991:1-22.
10 DeWal H, Ahn A, Raskin KB. Thermal energy in arthroscopic surgery of the wrist. Clinics in Sports Medicine. 2002;21:727-735.
11 Vangsness CTJr., Mitchell WIII, Nimni M, Erlich M, Saadat V, Schmotzer H. Collagen shortening: An experimental approach with heat. Clinical Orthopaedics and Related Research. 1997;337:267-271.
12 Lopez MJ, Hayashi K, Fanton GS, Thabit GIII, Markel MD. The effect of radiofrequency energy on the ultrastructure of joint capsular collagen. Arthroscopy. 1998;14:495-501.
13 Lu Y, Hayashi K, Edwards RB, Fanton GS, Thabit G, Markel MD. The effect of monopolar radiofrequency treatment pattern on joint capsular healing: In vitro and in vivo studies using an ovine model. Am J Sports Med. 2000;28:711-719.
14 Wall MS, Deng XH, Torzilli PA, Doty SB, O’Brien SJ, Warren RF. Thermal modification of collagen. J Shoulder Elbow Surg. 1998;8:339-344.
15 Fanton GS. Arthroscopic electrothermal surgery of the shoulder. Oper Tech Sports Med. 1998;6:139-146.
16 Obrzut LS, Hecht P, Hayashi K, Fanton GS, Thabit GIII, Markel MD. The effect of radiofrequency energy on the length and temperature properties of the glenohumeral joint capsule. Arthroscopy. 1998;14:395-400.
17 Ruch DS, Poehling GG. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg. 1996;21A:412-417.
18 Hayashi K, Markel MD. Thermal capsulorrhaphy treatment of shoulder instability: Basic science. Clin Orthop. 2001;390:59-72.
19 Hecht P, Hayashi K, Cooley AJ, Lu Y, Fanton GS, Thabit GIII, Markel MD. The thermal effect of monopolar radiofrequency energy on the properties of joint capsule: An in vivo histologic study using a sheep model. Am J Sports Med. 1998;26:808-814.
20 Berger RA. The gross and histologic anatomy of the scapholunate interosseous ligament. The Journal of Hand Surgery. 1996;21A:170-178.
21 Sokolow C, Saffar P. Anatomy and histology of the scapholunate ligament. Hand Clin. 2001;17:77-81.
22 Geissler WB, Haley T. Arthroscopic management of scapholunate instability. Atlas of Hand Clinics. 2001;6:253-274.
23 Goldberg SH, Strauch RE, Rosenwasser MP. Scapholunate and lunotriquetral instability in the athlete. Diagnosis and management operative techniques in sports medicine. 2006;14(2):108-121.
24 Geissler WB, Freeland AE, Savoie F, et al. Intracarpal soft-tissue lesions associated with an intra articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-364.
25 Weiss APC, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. The Journal of Hand Surgery. 1997;22A:344-349.
26 Whipple TL, Schengel D, Caffrey WD. Arthroscopic reduction and internal fixation of scapholunate dissociation. Arthroscopy. 1992;8(3):410.