CHAPTER 11 Arthroscopic Synovectomy for Inflammatory Arthritis
PATIENT EVALUATION
History and Physical Examination
Physical examination often reveals a boggy swelling posterolaterally, which indicates synovitis or effusion (Fig. 11-1). The range of motion of the elbow and forearm should be documented with the use of a goniometer. If there is a loss of motion, a soft end point suggests a soft tissue cause, such as a tense effusion with synovitis or capsular contracture, whereas a firm end point suggests osseous deformity. For instance, the synovial tissue in patients with hemophilic arthropathy is hypertrophic, highly vascular, and prone to impingement between the articular surfaces. Synovectomy alone cannot address the loss of motion due to a bony abnormality. Limitation in rotation may be caused by radial head deformity and may need to be addressed by radial head resection at the time of the synovectomy (see Chapter 10). In the setting of rotational stiffness, examination and imaging of the wrist are important to rule out pathology of the distal radioulnar joint as a cause, especially in patients with rheumatoid arthritis, in which involvement of this joint is common.
Diagnostic Imaging
Plain radiographs of the elbow reveal the degree of joint destruction, which aids in estimating the expected efficacy of synovectomy in the rheumatoid elbow (Fig. 11-2A and B). The Mayo Clinic classification of rheumatoid elbows,11 which grades the severity of disease based on the radiographic appearance, can be useful in guiding treatment. Grade I is primarily synovitis with no radiographic changes other than periarticular osteopenia or soft tissue swelling. In grade II, there is narrowing of the joint, but the architecture of the joint is intact. In grade III, there is alteration of the subchondral architecture of the joint, such as thinning of the olecranon or resorption of the trochlea or capitellum. In grade IV, there is gross destruction of the joint. Grade V is ankylosis.
Computed tomography (CT) can better define the osseous anatomy, including osteophytes and deformity of the radial head. Radial head deformities identified on imaging may need to be addressed by radial head resection at the time of the synovectomy (see Chapter 10). Magnetic resonance imaging (MRI) is useful for determining the extent of synovitis and nonossified loose bodies (see Fig. 11-2C and D).
Indications and Contraindications
Rheumatoid arthritis of the elbow is the most common indication for arthroscopic synovectomy in inflammatory arthritis.1–4 Synovectomy for rheumatoid arthritis of the elbow is indicated in the setting of persistent, painful synovitis with associated loss of function despite an adequate trial of medical management. Although the best results are seen in patients with some preserved articular cartilage and only mild bony deformity, arthroscopic synovectomy also should be considered in patients with more advanced disease who are younger or have pauciarticular disease. Arthroscopic débridement and synovectomy is a reasonable option in this group given the concerns about the longevity of total elbow arthroplasty.
Arthroscopic synovectomy is used to treat patients with hemophilia who have recurrent elbow hemarthroses and synovitis.5–7 Patients should have failed treatment with factor replacement for 3 to 6 months before being considered for synovectomy.8 With improved factor replacement, the incidence hemophilic patients with persistent synovitis requiring surgery seems to be decreasing over time. Arthroscopic synovectomy is also indicated for psoriatic arthritis and acute septic arthritis.9
Inadequate expertise of the treating surgeon is a contraindication to arthroscopic synovectomy. Arthroscopy of the rheumatoid elbow is technically demanding and has been associated with an increased risk of nerve injury.12 Patients with greater stiffness and deformity have diminished capsular volume, reducing the working room in the elbow.13 Initial visualization is often poor, and the capsule is often very thin and friable, increasing the risk of inadvertent capsulectomy and nerve injury. Surgeons with less arthroscopic experience should manage these patients with open surgery or refer them to someone more skilled at advanced arthroscopic techniques of the elbow.
Advanced articular destruction and bony deformity is a relative contraindication. The results of synovectomy are less favorable in this setting. Gross instability, often a result of severe joint destruction, is considered a contraindication, because synovectomy cannot address symptoms related to instability and may instead aggravate these symptoms.14
Treatment Alternatives
Alternative surgical treatment options include open synovectomy, combined synovectomy and radial head excision, interposition or excisional arthroplasty, and total elbow arthroplasty. Open synovectomy is a safer option in the hands of surgeons with less arthroscopic experience and is well supported by the literature for the treatment of rheumatoid synovitis in early stages of the disease.15–30
Conversion to an open procedure should be performed if there is an inadequate view to proceed safely or a slow progression of the arthroscopy due to technical challenges. Historically, most reports of open synovectomy for rheumatoid arthritis have included a radial head resection.15–30 Currently, the decision to resect the radial head at the time of synovectomy is based on the degree of radial head deformity and how much it is thought to be contributing to the symptoms. The surgeon should retain the radial head if possible. An unstable elbow can be made worse by removing the stabilizing effect of the radial head (see Chapter 10). Even in a stable elbow, radial head excision increases loading on the ulnohumeral joint and may lead to more rapid progression of arthritis.
Interposition arthroplasty has fallen out of favor in treating inflammatory arthritis, because it tends to be unpredictable compared with total elbow arthroplasty.31,32 Its use is currently limited to younger patients with polyarticular disease too advanced to benefit from synovectomy and débridement. Total elbow arthroplasty is the procedure of choice for most patients with advanced rheumatoid arthritis, particularly older patients with polyarticular disease.
Arthroscopic Technique
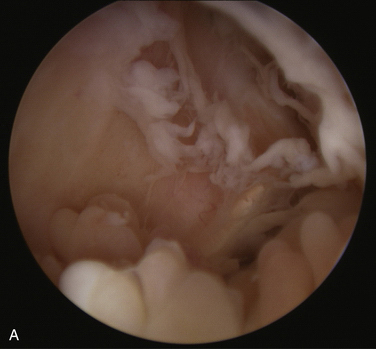
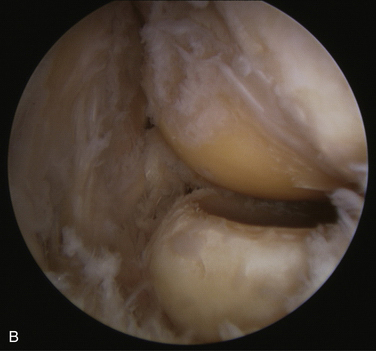
The extensive synovitis often makes the initial view very poor (Fig. 11-3). The full-radius resector should not be turned on until it is confirmed that the instruments are within the joint. The joint synovium is removed with the resector while preserving joint capsule. Visualization improves with the removal of synovium, and the surgeon should proceed cautiously until a good view is obtained. The capsule is typically very thin in rheumatoid elbows, making it easy to inadvertently penetrate or resect. Keeping the tip of the resector in view at all times and pointed away from the capsule can help to protect the capsule. Extra caution should be used when removing synovium anterior to the radial head in the region of the posterior interosseous nerve and in the posteromedial gutter near the ulnar nerve.
We prefer to start the synovectomy in the anterior compartment (Fig. 11-4A to D). The proximal anterolateral portal is the viewing portal, the proximal anteromedial portal is the working portal, and a direct posterior portal is used as an outflow portal with a drainage cannula. The viewing and working portals are exchanged using a switching stick to complete the anterior synovectomy. If the view is insufficient, a middle anterolateral or middle anteromedial portal can be established, and a retractor (e.g., Howarth elevator) is inserted to retract the capsule. The posterior synovectomy is performed next, starting with a direct posterior viewing portal and a middle posterolateral working portal. Care is taken in the area of the medial recess because of the risk of injury to the ulnar nerve. The lateral compartment can be addressed by viewing from the middle posterolateral portal and working through a distal posterolateral (i.e., soft spot) portal, and vice versa (see Fig. 11-4E and F).
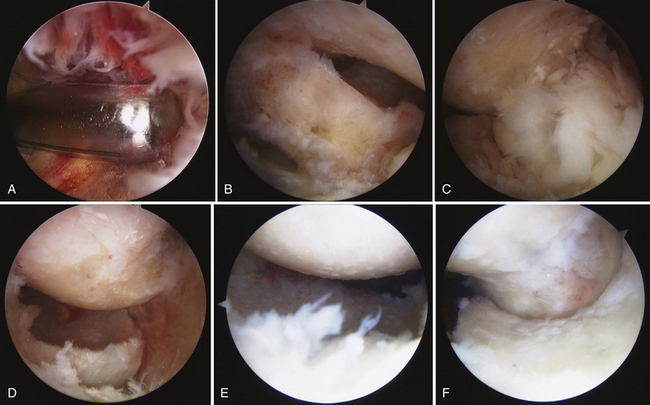
FIGURE 11-4 A 57-year-old woman had with Mayo Grade III rheumatoid arthritis of the left elbow with associated intractable synovitis. A, The initial view of the anterior joint from the proximal anterolateral portal reveals extensive synovitis. B, The arthroscopic view shows the coronoid after anterior synovectomy. C, Synovitis of the radiocapitellar joint is seen from the proximal anteromedial portal. D, The arthroscopic view shows the radiocapitellar joint after anterior synovectomy. E and F, The radiocapitellar and ulnohumeral joints are seen from the distal posterolateral portal after synovectomy.
Radial head excision should be reserved for patients with a stable elbow and a radial head deformity impeding rotation (see Chapter 10). Osteophyte débridement and capsulectomy may be indicated in some cases, and they can be performed arthroscopically with the synovectomy. Osteophytes that are impeding joint motion are removed with a burr if needed. An anterior or posterior capsulectomy is performed if there is significant restriction of elbow flexion or extension and the patient desires improved motion. Caution should be exercised when removing the anterolateral capsule because of the proximity of the posterior interosseous nerve.
PEARLS& PITFALLS
PEARLS
PITFALLS
OUTCOMES
Open elbow synovectomy, with or without radial head excision, is an effective treatment for the rheumatoid elbow.15–30 The best results are obtained in patients with some preserved articular cartilage and mild bony deformity (corresponding to grade I, II, and early III involvement).14 Results vary, but studies indicate that 70% to 90% have satisfactory outcomes within the first 3 to 5 years, although these improvements deteriorate with time.14 There is no evidence that open synovectomy arrests the progress of the disease process. Further studies are needed that employ more potent disease-modifying agents.
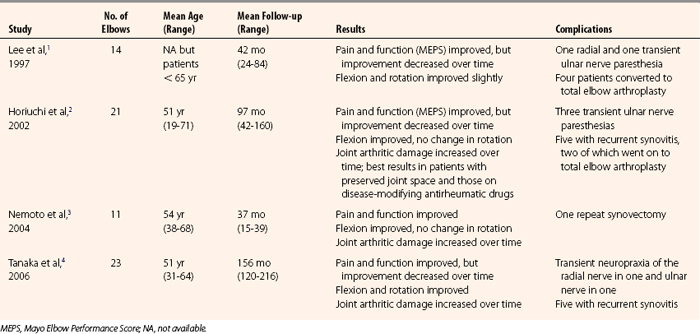
The literature provides limited information about the results of arthroscopic synovectomy for rheumatoid arthritis and even less information for other conditions (Table 11-1). Compared with open procedures, arthroscopic synovectomy offers theoretical advantages of being less invasive, which speeds recovery and limits postoperative pain, and allowing the surgeon to better visualize all areas of the elbow and address intra-articular pathology. Although there are no published randomized clinical trials comparing the relative efficacy and risks of open versus arthroscopic synovectomy, reports in the literature suggest that the outcomes of arthroscopic synovectomy are comparable to those of open synovectomy. As with open synovectomy, results deteriorate with time1,2,4 and depend on the severity of arthritis, with better results expected for elbows without significant osseous destruction and with some preserved articular cartilage.1,2
In 1997, Lee and Morrey1 initially reported good or excellent results for 93% of patients, but these results deteriorated to 57% by 42 months postoperatively. In 2001, Horiuchi and colleagues2 reported good to excellent results for 71% of patients at 2 years, but the rate deteriorated to 43% by 8 years. However, if elbows with advanced cartilage loss and bony deformity were excluded, the results were 100% and 71% of patients with good or excellent results at 2 and 8 years, respectively. Patients maintained on disease-modifying agents had a lower incidence of recurrent synovitis and a better long-term outcome.
In 2006, Tanaka and coworkers4 reported a prospective comparative study of arthroscopic versus open synovectomy with 23 elbows in each group. At a mean follow-up of 10 years, 48% of those treated arthroscopically and 70 % of those treated with open procedures had minimal or no pain. There were no significant differences found between the groups with respect to pain, function, or range of motion. Improvements in each of these outcomes deteriorated with time. A subgroup of patients with a preoperative flexion arc of less than 90 degrees had significantly better function when treated arthroscopically instead of with an open procedure.
Less is known about the results of arthroscopic synovectomy for hemophilic arthropathy of the elbow. Although studies are limited to very small numbers and they often combine results of synovectomy of other joints, there is evidence that arthroscopic synovectomy decreases the rate of recurrent hemarthrosis.5–8
Transient nerve paresthesias, recurrent synovitis, and persistent pain requiring repeated synovectomy or total elbow arthroplasty have been reported as complications of arthroscopic synovectomy.1–4,12
CONCLUSIONS
Although arthroscopic synovectomy is one of the most technically demanding arthroscopic elbow operations, early evidence supports its safety and efficacy. The outcomes and complications likely depend on the arthroscopic experience of the surgeon, the underlying disease severity of the patient, and the concomitant use of disease-modifying medications.
1. Lee BPH, Morrey BF. Arthroscopic synovectomy of the elbow for rheumatoid arthritis. J Bone Joint Surg Br. 1997;79B:770-772.
2. Horiuchi K, Momohara S, Tomatsu T, et al. Arthroscopic synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 2002;84A:342-347.
3. Nemoto K, Arino H, Yoshihara Y, Fujikawa K. Arthroscopic synovectomy for the rheumatoid elbow: a short-term outcome. J Shoulder Elbow Surg. 2004;13:652-655.
4. Tanaka N, Sakahashi H, Hirose K, et al. Arthroscopic and open synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 2006;88:521-525.
5. Dunn AL, Busch MT, Wyly JB, et al. Arthroscopic synovectomy for hemophilic joint disease in a pediatric population. J Pediatr Orthop. 2004;24:414-426.
6. Tamurian RM, Spencer EE, Wojtys EM. The role of arthroscopic synovectomy in the management of hemarthrosis in hemophilia patients: financial perspectives. Arthroscopy. 2002;18:789-794.
7. Journeycake JM, Miller KL, Anderson AM, et al. Arthroscopic synovectomy in children and adolescents with hemophilia. J Pediatr Hematol Oncol. 2003;9:726-731.
8. Verma N, Valentino LA, Chawla A. Arthroscopic synovectomy in haemophilia: indications, technique and results. Haemophilia. 2007;13(suppl 3):38-44.
9. Jerosch J, Hoffstetter I, Schroder M, Castro W. Septic arthritis: arthroscopic management with local antibiotic treatment. Acta Orthop Belg. 1995;61:126-134.
10. Kamineni S, O’Driscoll S W, Morrey BF. Synovial osteochondromatosis of the elbow. J Bone Joint Surg Br. 2002;84B:961-966.
11. Morrey BF, Adams RA. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J Bone Joint Surg Am. 1992;74:479-490.
12. Kelly EW, Morrey BF, O’Driscoll SW. Complications of elbow arthroscopy. J Bone Joint Surg Am. 2001;83A:25-34.
13. Gallay SH, Richards RR, O’Driscoll SW. Intra-articular capacity and compliance of stiff and normal elbows. Arthroscopy. 1993;9:9-13.
14. Lee BPH, Morrey BF. Synovectomy of the elbow. In: Morrey BF, editor. The Elbow and Its Disorders. 3rd ed. Philadelphia, PA: WB Saunders; 2000:708-717.
15. Woods DA, Williams JR, Gendi NS, et al. Surgery for rheumatoid arthritis of the elbow: a comparison of radial-head excision and synovectomy with total elbow replacement. J Shoulder Elbow Surg. 1999;8:291-295.
16. Gendi NST, Azon JMC, Carr AJ, et al. Synovectomy of the elbow and radial head excision in rheumatoid arthritis. J Bone Joint Surg Br. 1997;79B:918-923.
17. Lonner JH, Stuchin SA. Synovectomy, radial head excision, and anterior capsular release in stage III inflammatory arthritis of the elbow. J Hand Surg Am. 1997;22A:279-285.
18. Ferlic DC, Patchett CE, Clayton ML, Freemand AC. Elbow synovectomy in rheumatoid arthritis. Long-term results. Clin Orthop Relat Res. 1987;220:119-225.
19. Maenpaa HM, Kuusela PP, Kaarela K, et al. Reoperation rate after elbow synovectomy in rheumatoid arthritis. J Shoulder Elbow Surg. 2003;12:480-483.
20. Makai F, Chudacek J. Long-term results of synovectomy of the elbow with excision of the radial head in rheumatoid arthritis. In: Hamalainen M, Hagena FW, eds. Rheumatoid Surgery of the Elbow. Hamalainen M, Hagena FW, editors. Long-term results of synovectomy of the elbow with excision of the radial head in rheumatoid arthritis. Vol. 15, Basel, Switzerland: Karger; 1991:22-26.
21. Tulp NJ, Winia WP. Synovectomy of the elbow in rheumatoid arthritis: long-term results. J Bone Joint Surg Br. 1989;71:664-666.
22. Taylor AR, Mukerjea SK, Rana NA. Excision of the head of the radius in rheumatoid arthritis. J Bone Joint Surg Br. 1986;58:485-487.
23. Rymaszewski LA, Mackay I, Amis AA, Miller JH. Long-term effects of excision of the radial head in rheumatoid arthritis. J Bone Joint Surg Br. 1984;66:109-113.
24. Wilson HDW, Arden GP, Ansell BM. Synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Br. 1973;55:106-111.
25. Eichenblat HM, Hass A, Kessler I. Synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 1982;64:1074-1078.
26. Brumfield HRH, Resnick CT. Synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 1985;67:16-20.
27. Herold N, Schrøder HA. Synovectomy and radial head excision in rheumatoid arthritis: 11 patients followed for 14 years. Acta Orthop Scand. 1995;66:252-254.
28. Rodríguez-Merchán EC, Magallón M, Galindo E, López-Cabarcos C. Hemophilic synovitis of the knee and the elbow. Clin Orthop Relat Res. 1997;343:47-53.
29. Linclau LA, Winia WPCA, Korst JK. Synovectomy of the elbow in rheumatoid arthritis. Acta Orthop Scand. 1983;54:935-937.
30. Saito T, Koshino T, Okamoto R, Horiuchi S. Radical synovectomy with muscle release for the rheumatoid elbow. Acta Orthop Scand. 1986;57:71-73.
31. Kauffman JI, Chen AL, Stuchin S, Di Cesare PE. Surgical management of the rheumatoid elbow. J Am Acad Orthop Surg. 2003;11:100-108.
32. Ljung P, Jonsson K, Larsson K, Rydholm U. Interposition arthroplasty of the elbow with rheumatoid arthritis. J Shoulder Elbow Surg. 1996;5(pt 1):81-85.