CHAPTER 8 Arthroscopic Subacromial Decompression
Arthroscopic subacromial decompression (ASAD) has become one of the most commonly performed surgical procedures of the shoulder. The arthroscopic technique has evolved significantly from the open anterior acromioplasty as described by Neer1,2 and others, and the learning curve should not be underestimated.
ANATOMY AND PATHOANATOMY
Knowledge of the coracoacromial anatomy is crucial for diagnostic accuracy, operative facility, and avoidance of complications. The shape of the acromion and contour of its undersurface is best evaluated with Neer’s supraspinatus outlet view. Bigliani and colleagues3 have described three distinct acromial shapes: type 1, flat (divergent); type 2, curved (congruent); and type 3, hooked (stenotic). They found an increased correlation between the type 3 hooked acromion and underlying full-thickness rotator cuff tears (69.5% for type 3 and 3% for type 1). This radiographic view is also valuable for determining the overall slope and thickness of the acromion and in predetermining where and how much bone should be removed with acromioplasty, when indicated.
It is important to remember that the subacromial bursa is an anterior structure. It extends from the anterior half to one third of the acromion to just medial to the acromioclavicular (AC) joint to 1 to 2 cm anterior to the acromion and 2 to 3 cm laterally. The bursal wall is frequently thickened and troublesome posteriorly, and has been termed the posterior bursal curtain. This curtain frequently closes as one backs the arthroscope posteriorly to get a larger field of view of the subacromial bursa. It is frequently necessary to resect a portion of this structure when performing subacromial surgery.
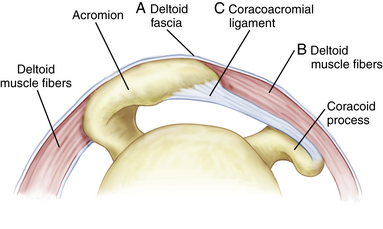
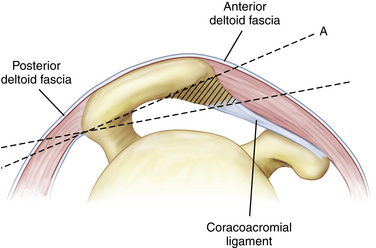
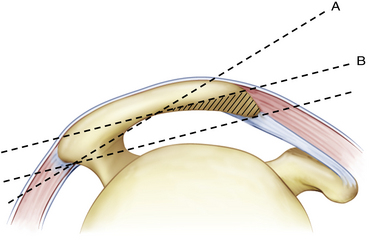
The anatomy of the coracoacromial ligament (CAL) is pertinent to the technique of acromioplasty. It attaches to the front and undersurface of the acromion as a thick band and continues around the anterolateral corner to attach to the lateral ridge for a variable distance.4 Anteriorly, the posterior medial band of the coracoacromial ligament attaches to the anteroinferior edge of the acromion, whereas the deltoid fascia attaches more superiorly (Fig. 8-1).
Anteriorly, the CA ligament attaches on the inferior acromial surface and falls away easily from the overlying anterior deltoid muscle and fascia when detached. Laterally, however, the anterior lateral band of the coracoacromial ligament blends inextricably with the deltoid muscle fascia along the lateral acromion.5 Care must be taken when releasing or ablating the anterolateral band of the CAL not to detach the fascia aggressively or resect too much bone laterally, because this may result in a deltoid detachment.
Edelson and Luchs6 and others have noted variable degrees of transformation of the coracoacromial ligament into bone at its acromial insertion, most commonly in the anterolateral band.4 Gartsman7 has labeled this phenomenon anterior acromial protuberance. Rockwood and Lyons,8 in their open technique, recommend resecting 8 to 10 mm of full-thickness anterior bone and then reattaching the deltoid fascia. This technique of full-thickness anterior bone resection back to the level of the AC joint has been included in a description of arthroscopic subacromial decompression.9
HISTORY AND PHYSICAL EXAMINATION
Causes of Impingement
Secondary Impingement
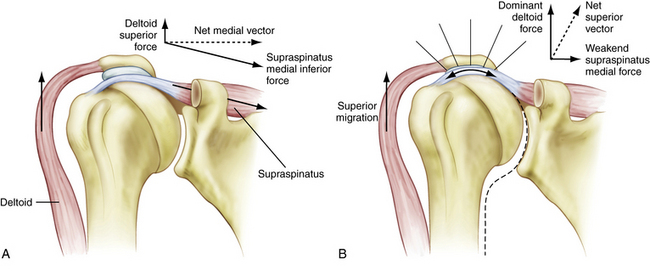
The concept of secondary impingement originated with Codman,10 who proposed an intrinsic tendinous degeneration as the essential lesion in rotator cuff disease. The microvascular studies of Rathbun and McNab11 and Moseley and Goldie12 support this concept. The subsequent pain and weakness of the supraspinatus compromises its function as a humeral head depressor and allows the superior vector forces of the deltoid to dominate, producing a secondary, superiorly directed impingement of the cuff into the acromion (Fig. 8-2 A, B).
Jobe and associates13 expanded this concept to include patients with underlying anterior glenohumeral ligament instability. As the humeral head subluxes anteriorly, the cuff is secondarily compressed against the coracoacromial arch. In addition, Matsen and coworkers14 have noted that posterior inferior capsular contracture produces an obligate anterior superior humeral head translation, with arm elevation and subsequent superior impingement.
Chronic Secondary Impingement with Pathologic Subacromial Changes
If the underlying cause of the secondary impingement is not rectified with a diligent rehabilitation program (e.g., scapular alignment, posterior capsule stretching), the cuff and humeral head elevate. The decreased acromial–humeral head distance results in inflammation and anterior mechanical irritation in the subacromial space, with the development of a traction spur in the acromial attachment of the CAL. This anterior acromial osteophyte formation can lead to awning impingement with arm elevation and subsequent bursal side cuff fraying and roughening. Even if subacromial space changes are present on a secondary basis, débridement, including a possible subacromial decompression, must be considered.
Primary Extrinsic Impingement
Neer1 introduced the concept of extrinsic impingement of the anterior acromion, coracoacromial arch, and AC joint on the underlying rotator cuff and biceps tendon. He also emphasized that forward flexion of the arm is the dominant functional position and that anterior decompression, not lateral acromionectomy, is the appropriate operative approach for significant cuff degeneration.
Neer’s impingement sign is determined with the patient seated in front of the examiner, who stabilizes the scapula as the arm is elevated slightly lateral to the midline to impinge the tuberosity against the acromion (Fig. 8-3).
Pain thus produced is eliminated by injecting 10 mL of 1% lidocaine (Xylocaine) into the subacromial bursa beneath the anterior acromion (impingement injection test) to confirm the diagnosis. Hawkins and Kennedy15 have described a second impingement sign, in which the arm is flexed forward 90 degrees and then forcibly internally rotated, jamming the supraspinatus tendon against the anterior edge of the coracoacromial ligament to produce pain (Fig. 8-4).
Posterior Superior Internal Impingement
Walch and colleagues16 and Jobe and associates17 have described a variety of secondary impingements noted in overhead athletes that occur when the arm is maximally externally rotated while abducted and extended, such as in the cocking phase of throwing. In this position, the posterosuperior articular surface fibers of the supraspinatus are placed under tension and shear but are also compressed between the humeral head and adjacent glenoid rim, resulting in posterior superior synovitis and partial undersurface tears.
Morgan and Rajan18 have described a subset of throwers with glenohumeral internal rotation deficit (GIRD). This posteroinferior capsular contracture produces a posterosuperior humeral head translation, superior labral separation, and internal impingement. Whether any underlying anterior instability is a factor in this type of compression needs to be determined with each individual case. In long-standing cases of internal impingement and superior labral pathology, obligate anterior instability can be encountered and may need to be addressed.
Anterior Subcoracoid Impingement
Gerber and coworkers19 have described this type of anterior impingement between the humeral head and coracoid process. The coracoid tip may be enlarged, fractured, or iatrogenically altered, such as occurs with a laterally positioned Bristow-Latarjet transfer of the coracoid tip onto the anterior glenoid rim. Fractures of the coracoid from the recoil of a rifle in hunters may heal with lateral displacement. These changes are best noted on axillary view x-rays or a computed tomography (CT) scan with the arm flexed 90 degrees and internally rotated.
Whatever the underlying cause, the tip of the coracoid is positioned more laterally than normal and, as the arm is brought into forward flexion, there is a compression of the anterior rotator cuff between the humeral head and tip of the coracoid. This produces pain with Neer’s forward flexion test, but it occurs usually between 80 and 130 degrees of flexion rather than at full flexion. Also, Hawkins flexion and internal rotation test is consistently positive, but the pain is lower and more anterior than with superior impingement. The patient also demonstrates decreased horizontal adduction, with pain similar to that found with AC disease (Fig. 8-5) but again, the pain is more at the tip of the coracoid and not at the AC joint. Selective injections in the region of the coracoid process can help verify the diagnosis.
TREATMENT OPTIONS: INDICATIONS AND CONTRAINDICATIONS
One needs to treat all varieties of impingement with a diligent conservative treatment program, including scapular and rotator cuff retraining, range-of-motion (ROM) exercises to regain full internal and external rotation, nonsteroidal anti-inflammatory drugs (NSAIDs), differential subacromial-AC joint injection, and activity modification for 3 to 6 months in an effort to avoid operative intervention.20
PEARLS& PITFALLS
PITFALLS
The underlying cause of secondary impingement (normally seen in younger individuals with normal bony anatomy) should respond to aggressive scapular-thoracic rehabilitation and stretching or subsequent surgical intervention directed at the primary laxity or contracture of the shoulder. The causes of internal impingement and anterior subcoracoid impingement need to be addressed directly at the capsular or coracoid level and do not respond to anterior superior decompression. Also, isolated AC disease and massive cuff tears with significant underlying glenohumeral arthritis likely to necessitate future arthroplasty should not be decompressed.
The need for arthroscopic subacromial decompression at the time of rotator cuff repair remains controversial. A recent double-blind prospective study by Milano and colleagues21 comparing rotator cuff repair with and without ASAD showed no significant difference in final outcome, although the authors did not evaluate or compare those patients with clinical and radiographic evidence of bursal impingement versus those without. In contrast, MacDonald and associates22 found improved results in the cuff repair plus ASAD group if the acromion was type 2 or 3.
Arthroscopic Subacromial Decompression
The arthroscopic technique for subacromial decompression was first described by Johnson23 in 1986. Ellman24 presented the first series with follow-up and detailed description of the operative technique. Paulos and Franklin25 presented one of the largest early series (80 patients) and introduced the use of the midlateral subacromial portal. Sampson and coworkers26 first described the cutting block technique for acromioplasty wherein the scope is placed laterally and the burring instruments are advanced from the posterior portal, using the posterior half of the acromion as a guide for resection. The authors also emphasized the importance of the supraspinatus outlet x-ray in both preoperative planning and postoperative evaluation and the benefits of evaluating the flatness of the cut from the lateral and the posterior portals.
Preoperative Planning and Decisions
If diligent nonoperative care has been unsuccessful and the correct type of bursal side impingement has been diagnosed, one must then perform the arthroscopic surgical technique correctly to arrive at a successful result. Arthroscopic subacromial decompression is not just an arthroscopic replication of the open procedure as described by Neer1,2 and Rockwood and Lyons.8 Arthroscopically, one avoids taking full-thickness bone off the anterior acromion so as not to detach the deltoid fascial attachment or resecting the CA ligament.27 Fortunately, long-term results for arthroscopic subacromial decompression are found to be superior to open acromioplasty.28
Whether one fashions a type 1 flat divergent surface or a type 2 congruent surface, both of which are physiologic variants, depends on the shape and thickness of the acromion and the preference of the surgeon based on arthroscopic findings. The most commonly cited concern with subacromial decompression is iatrogenic harm to the coracoacromial arch and destabilization of the glenohumeral joint with anterior superior subluxation of the head.29 Although not uncommonly seen in open decompression surgery when the anterior deltoid is detached and fails to heal, it has only rarely been reported as a clinical problem with the arthroscopic technique,30 even though slight elevation has been noted in cadaver studies.31 In fact, this superior migration is not commonly reported, even with large os acromial resections. This may be related to fact that the CAL essentially re-forms after release or partial resection.32 Some decrease in acromion-humeral distance after ASAD has been reported, however, when associated cuff tears are left unrepaired.33 If one cannot repair a large or massive cuff tear or the acromion is very thin, then resection of the impinging osteophyte and smoothing, rather than flattening, the acromion would be the appropriate intervention. Acromioplasty in the younger overhand athlete with secondary impingement-related pain only serves to destabilize any existing instability further.
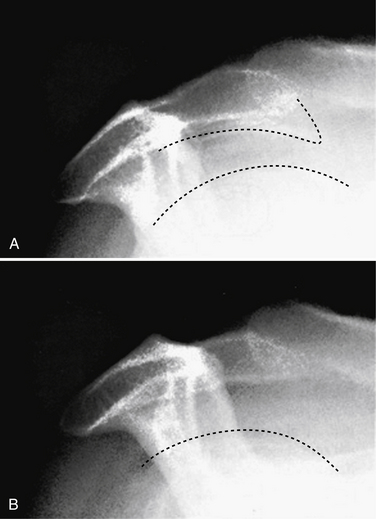
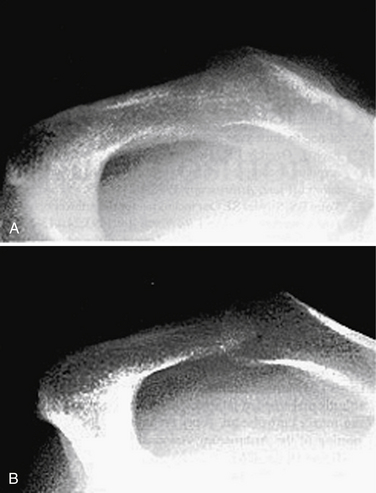
Careful preoperative x-ray evaluation is necessary to determine the appropriate operative approach and to avoid complications. AP, outlet, and axillary views are the key to evaluating the acromion. The AP view demonstrates the orientation and/or disease of the AC joint and the lateral slope of the acromion. The outlet view is used to determine the shape of the acromion (type 2 or 3) and overall thickness. On the outlet view, lines are drawn on the undersurface of the acromion, one from the front tip of the acromion to the posterior edge and a second along the posterior half of the undersurface of the acromion, extending out anteriorly. The distance between these two lines at the anterior margin approximates the amount of undersurface anterior bone that would be resected if one desires to flatten the undersurface of the arch completely (Fig. 8-7).
The axillary view is used to determine the shape of the acromion (cobra versus square-tipped) and whether there is any anterior acromial protuberance or subtle AC arthritis. If, on the outlet view, one notes a very thin or curved acromion, the flat cut line on the undersurface of the posterior half of the acromion may actually exit the superior aspect of the acromion, taking off too much anterior bone (Fig. 8-8).
In these cases, the cutting block technique, as described by Sampson and colleagues,26 would be inappropriate. Instead, the lateral approach would be more applicable, removing less anterior bone and not producing a type I flat acromion but a more feathered type 2 devoid of osteophytes. The procedure may be performed using the beach chair or lateral decubitus position.
TECHNIQUES
Lateral Approach: Limited Anterior Resection Technique
Preoperatively, one will have decided whether to use a lateral approach—a limited anterior resection—or a cutting-block approach for the decompression.24 If the patient has a thin curved acromion and a lateral approach is appropriate, place the lateral portal 3.5 to 4 cm lateral to the acromion and about midway between the midportion of the acromion and anterolateral corner. Use an 18-gauge needle as a guide to determine if the portal permits access for instruments along the anteroinferior edge of the acromion so that the motorized instruments can be directed slightly upward at the acromion for ease in burring and shaving.
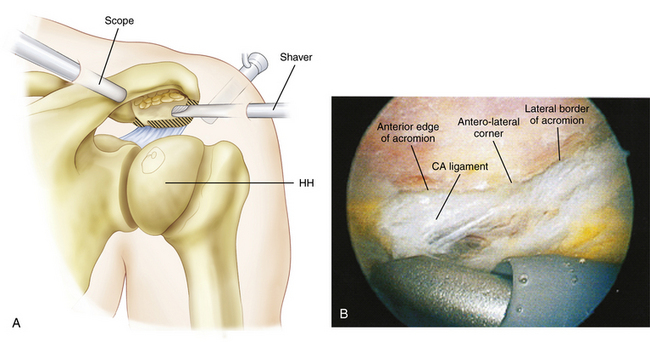
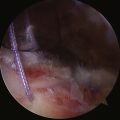
The soft tissue on the undersurface of the anterior half of the acromion is then débrided with an aggressive shaver and/or a cautery ablation system (Fig. 8-9). Care should be taken with either instrument to stay on the undersurface of the bone and not pop off anteriorly or laterally into the deltoid fibers, which are very vascular. The anterolateral corner of the acromion is identified with an 18-gauge needle directed from superiorly; the débridement is started at this point, progresses medially toward the AC joint and then subsequently from this point posteriorly, along the lateral edge of the acromion for about 1 cm.
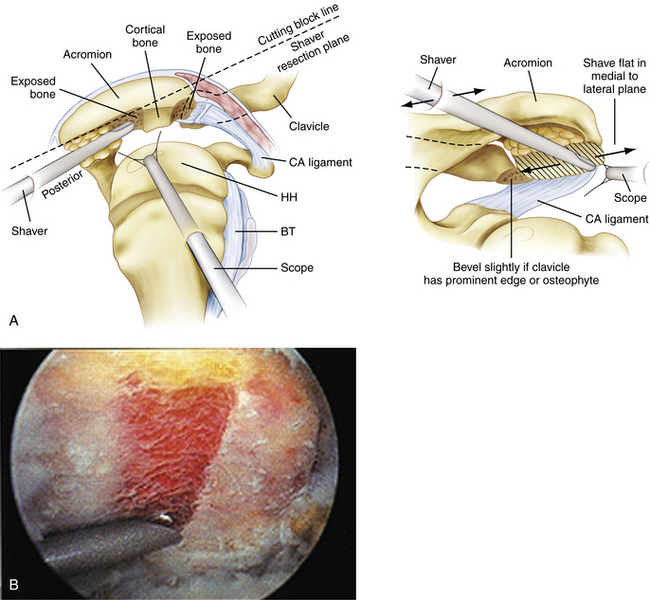
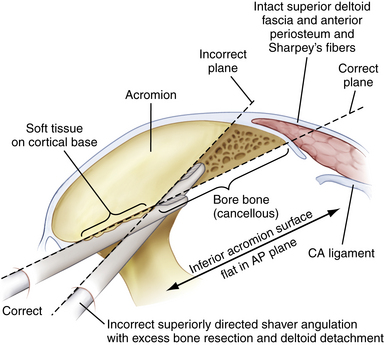
From the preoperative planning, the amount of bone to be resected is known, as is the diameter of the burr. Starting at the anterolateral corner, the appropriate amount of anterior hook or osteophytic bone is then resected from anterior to medial. Care is taken not to remove full-thickness bone anteriorly and thereby detach the anterior deltoid fascia. This cannot be subsequently repaired, as in an open operative procedure. After the anterior bone is resected from lateral to medial, tapering of the remaining bone posteriorly is then accomplished from anterior to posterior to the midportion of the acromion (Fig. 8-10).
Because of the thin and curved nature of the acromion, the goal is not to produce a completely flat undersurface but to perform a smooth and even taper (Fig. 8-11). The arthroscope is always placed laterally to evaluate the decompression in two planes.
Two-Portal Cutting Block Technique
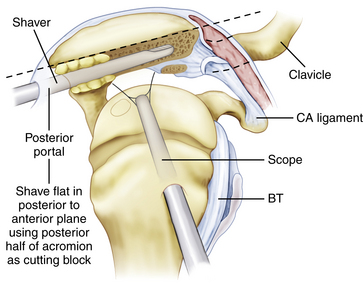
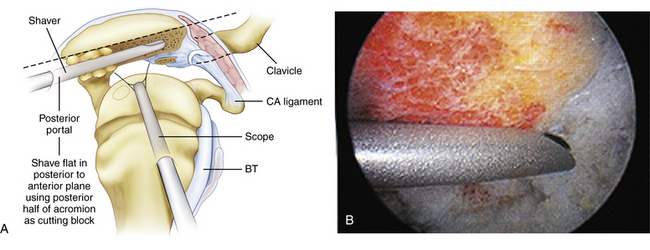
If, on the basis of the preoperative planning, the patient has a thick acromion and a prominent hook anteriorly, one may use the cutting block technique as described by Sampson and associates.26
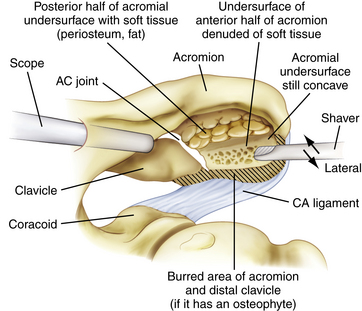
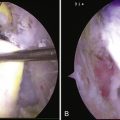
After the anterior half of the acromion is débrided and the anterior lateral bony edges outlined with minimal resection, the arthroscope is placed in the lateral portal to view the arch of the acromion. The burr is introduced though the posterior portal on the undersurface of the posterior half of the acromion. Using this as a cutting block, the burr is advanced anteriorly with a sweeping motion, medially to laterally (Figs. 8-12 and 13). The anterior hook of the acromion is resected and the undersurface flattened in the sagittal plane. Take care not to advance the burr anteriorly into deltoid fibers or fascia.
COMPLICATIONS
The most common complications associated with arthroscopic ASAD are the following:
Inaccurate bone resection is best avoided by thorough preoperative planning. Use of the cutting block technique, when appropriate, leads to more consistent results, with less likelihood of deltoid detachment. Care should be taken to avoid soft tissue interposition between the burr and posterior acromion, which would result in excess superior angulation (Fig. 8-14).
SUMMARY
A successful arthroscopic subacromial decompression is predicated not only on sound arthroscopic technique, but also on proper patient selection. Overuse of acromioplasty can be harmful, and should only be undertaken when the physical findings and diagnostic imaging are corroborated and confirmed again at surgery. Performing an arthroscopic subacromial decompression in a normal subacromial space should be avoided, especially in the younger patient. At surgery, arthroscopic evaluation should confirm extrinsic bursal side fraying and matching coracoacromial arch contact changes. The appropriate technique of ASAD is dictated by the bony anatomy. The approach to the AC joint should be determined preoperatively based on clinical findings and diagnostic imaging. Finally, intraoperative attention to potential complications and the use of meticulous technique will help lead to a positive surgical outcome (Fig. 8-15).
1. Neer C Anterior acromioplasty for chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg, 54A; 1972:41-50.
2. Neer C. Impingement lesions. Clin Orthop. 1983;173:70-77.
3. Bigliani LU, Morrison DS, April EW. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans. 1986;10:216.
4. Fealy S, April E, Khazzam J, et al The coracoacromial ligament: morphology and study of acromial enthesopathy. J Shoulder Elbow Surg, 14; 2005:542-548.
5. Gallino M, Vatiston B, Annaratone G, et al Coracoacromial ligament: a comparative arthroscopic and anatomic study. Arthroscopy, 11; 1995:564-567.
6. Edelson JG, Luchs J. Aspects of coracoacrornial ligament anatomy of interest to the arthroscopic surgeon. Arthroscopy. 1995;11:715-719.
7. Gartsman GM. Arthroscopic acromioplasty for lesions of the rotator cuff. J Bone Joint Surg. 1990;72A:169-180.
8. Rockwood CJr, Lyons F Shoulder impingement syndrome: diagnosis, radiographic evaluation and treatment with a modified Neer acromioplasty. J Bone Joint Surg (Am), 75; 1993:409-424.
9. Esch JC, Baker CL. Rotator cuff disease and impingement. In: Whipple TL, editor. Arthroscopic Surgery—The Shoulder and Elbow. Philadelphia: JB Lippincott; 1993:161-163.
10. Codman E Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. The Shoulder. Boston: Thomas Todd; 1934:73-75.
11. Rathbun J, McNab I. The microvascular pattern of the rotator cuff. J Bone Joint Surg. 1970;52B:540-553.
12. Moseley H, Goldie I. The arterial pattern of the rotator cuff on the shoulder. J Bone Joint Surg. 1963;45B:780-789.
13. Jobe F, Kvitne R, Giangarra C Shoulder pain in the overhand or throwing athlete: the relationship of anterior instability and rotator cuff impingement. Orthop Rev, 18; 1989:963-975.
14. Matsen F, Sidles J, Harryman D Practical Evaluation and Management of the Shoulder. Philadelphia: WB Saunders; 1994:40.
15. Hawkins R, Kennedy J. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151-158.
16. Walch G, Boileau P, Noel E, et al Impingement of the deep surface of the supraspinatus tendon on the posterior superior glenoid rim: an arthroscopic study. J Shoulder Elbow Surg, 1; 1992:238-245.
17. Jobe C Posterior superior glenoid impingement: expanded spectrum. Arthroscopy, 11; 1995:530-536.
18. Morgan C, Rajan S. Posterior inferior capsulotomy for glenohumeral internal rotation deficit in baseball pitchers. •••. 2004;20(suppl 1):9.
19. Gerber C, Terier F, Ganz R. The role of the coracoid process in chronic impingement syndrome. J Bone Joint Surg (Am). 1985;678:703-708.
20. Rubin B, Kibler W Fundamental principles of shoulder rehabilitation: conservative to postoperative management. Arthroscopy, 18(suppl 2); 2002:29-39.
21. Milano G, Grasso A, Deriu L, et al The role of subacromial decompression associated with arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy, 22; 2006:e17.
22. MacDonald P, Lapner P, McRae S, Leiter J. Arthroscopic rotator cuff repair with and without arthroscopic acromioplasty in the treatment of full-thickness rotator cuff tears. Arthroscopy. 2008;24:e19-e20.
23. Johnson L. Shoulder arthroscopy. In: Johnson LL, editor. Arthroscopic Surgery: Principles and Practice. St. Louis: CV Mosby; 1986:1371-1379.
24. Ellman H Arthroscopic subacromial decompression: analysis of one- to three-year results. Arthroscopy, 3; 1987:173-181.
25. Paulos LE, Franklin JL. Arthroscopic shoulder decompression development and application—five-year experience. Am J Sports Med. 1990;18:235-244.
26. Sampson TG, Nisbet JK, Glick JM. Precision acromioplasty in arthroscopic subacromial decompression of the shoulder. Arthroscopy. 1991;7:301-307.
27. Rogerson JS. The role of arthroscopic decompression and distal clavicle resection. In: Abrams JS, Bell RH, editors. Arthroscopic Rotator Cuff Surgery: A Practical Approach to Management. New York: Springer; 2007:83-104.
28. Odenbring S, Wagner P, Atroshi I Long-term outcomes of arthroscopic acromioplasty for chronic shoulder impingement syndrome: a prospective cohort study with a minimum of 12 years’ follow-up. Arthroscopy, 24; 2008:1092-1098.
29. Matsen F Rotator cuff. The Shoulder. Philadelphia: WB Saunders; 1998:755-839
30. Bonsel S. Detached deltoid during arthroscopic subacromial decompression. Arthroscopy. 2000;16:745-748.
31. Wellmann M, Petersen W, Zantop T, et al. Effect of coracoacromial ligament resection on glenohumeral stability under active muscle loading in an in vitro model. Arthroscopy. 2008;24:1258-1264.
32. Levy O, Copeland SA. Regeneration of the coracoacromial ligament after acromioplasty and arthroscopic subacromial decompression. J Shoulder Elbow Surg. 2001;10:317-320.
33. Kempf JF, Gleyze P, Bonnomet F, et al. A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy. 1999;16:56-66.