CHAPTER 5 Arthroscopic Resection of the Olecranon Bursa
TREATMENT
Open Excision
The alternative to arthroscopic resection is open resection of the bursa. There have been no comparisons of open and arthroscopic treatment. However, open treatment does involve a relatively large incision, with the attendant risk of wound complications such as poor healing.1 Patients may be left with residual hypersensitivity over the scar. However, it usually is considered a satisfactory alternative treatment in the absence of the necessary arthroscopic skills.
Control of Septic Bursitis
In a patient with septic bursitis, the sepsis should be controlled before carrying out an arthroscopic resection. The study from Stell2 indicated that acute olecranon septic bursitis could be managed on a conservative basis in many cases. The principle is to determine the infective agent. An aspirate of the bursa should be carried out with cultures and sensitivity tests performed.
Stell2 showed that most patients with acute septic bursitis could be managed conservatively without the need for surgical intervention. If intervention is required, we recommend drainage of the bursa and allowing it to heal.
Arthroscopic Technique
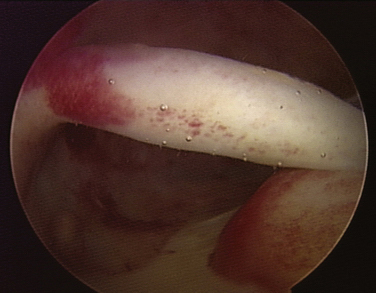
FIGURE 5-5 The view inside the olecranon bursa shows a thickened bursal sac with villous hyperplasia.
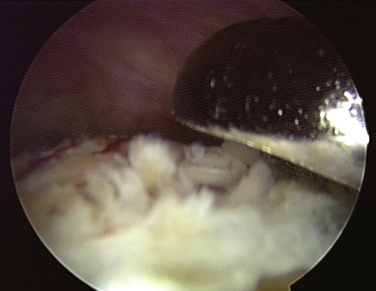
FIGURE 5-6 A 4.5-mm resector used for removing villous tissue can be seen at the 1-o’clock position.
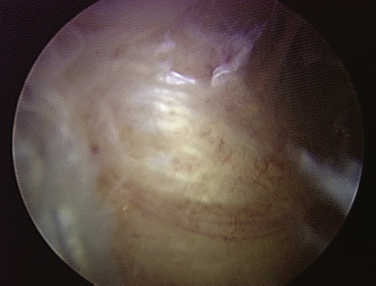
FIGURE 5-7 The arthroscopic view shows the triceps after bursal tissue has been removed. Notice the shiny fibers of the triceps tendon after stripping the bursal sac.
The portals are then closed with nylon. Marcaine is injected locally into the portals, and a compressive soft tissue dressing is applied over the olecranon.
PEARLS& PITFALLS
OUTCOMES AND CONCLUSIONS
There are only three reported arthroscopic series in the literature. In the report by Nussbaumer and colleagues,3 nine patients had resection of the olecranon bursa. There were no complications. In the report by Kerr and Carpenter,4 six patients had resection of the olecranon bursa, with complications occurring in two patients; one had gouty arthritis, and the other had CREST syndrome (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia), a limited form of scleroderma. In the report by Ogilvie-Harris,5 there were 31 cases of olecranon bursitis. Eight-six percent of the patients had no residual pain. There was residual pain over the olecranon in the remaining patients. In an unpublished review, another 14 cases were done with no complications or recurrences. These results indicate that the arthroscopic resection of the olecranon bursa can be a highly successful procedure.
1. Degreef I, De Smet L. Complications following resection of the olecranon bursa. Acta Orthop Belg. 2006;72:400-403.
2. Stell IM. Management of acute bursitis: outcome study of a structured approach. J R Soc Med. 1999;92:516-521.
3. Nussbaumer P, Candrian C, Hollinger A. Endoscopic bursa shaving in acute bursitis. Swiss Surg. 2001;7:121-125.
4. Kerr DR, Carpenter CW. Arthroscopic resection of olecranon and prepatellar bursae. Arthroscopy. 1990;6:86-88.
5. Ogilvie-Harris DJ, Gilbart M. Endoscopic bursal resection: the olecranon bursa and prepatellar bursa. Arthroscopy. 2000;16:249-253.