CHAPTER 9 Arthroscopic RASL
Introduction
Treatment of scapholunate instability due to rupture of the scapholunate interosseous ligament remains a challenge, with no predictable or reproducible procedure. The natural progression of SL instability has been documented, and in the last 30 years several treatments have been described to halt the ensuing pathomechanics.1 Soft-tissue reconstructions include capsulodesis procedures such as the Blatt procedure or the Szabo modification, which uses the dorsal intercarpal ligament. These techniques do not reduce the scapholunate (SL) interval, but are nonetheless thought to provide symptomatic relief.2,3 Brunelli has described a tenodesis of the scaphotrapezial joint using a strip of the FCR tendon, but long-term follow-up is lacking.4
Bone procedures include arthrodesis of the scaphoid and lunate (which has a high complication and nonunion rate) and the scaphotrapezialtrapezoid arthrodesis advocated by Watson.5,6 Results of this procedure have not been reproducible, and there is the suggestion of progressive arthrosis and limitation of motion over time. Unfortunately, both soft and bony techniques will ultimately impair grip strength and total arc of motion at the expense of scaphoid stabilization.2
Herbert initially described a surgical technique involving open reduction and reattachment of the ligament to the bone, combined with Herbert screw fixation across the scapholunate joint. The screw is normally left in situ for 12 to 18 months, allowing sufficient time for ligament healing and restoration of carpal stability.7
Rosenwasser and colleagues recently popularized this technique and endeavored to create a stable fibrous pseudarthrosis between the scaphoid and lunate by reducing and stabilizing the SL joint (or reduction association of the scaphoid-lunate RASL) with a Herbert bone screw (HBS). Long-term data is not available on this procedure, but early results are encouraging.8 The procedure they describe uses both dorsal and radial incisions for joint preparation and reduction (as well as screw placement). Further experience with the procedure led us to develop an arthroscopic (ARASL) technique, which minimizes the tissue trauma and facilitates precise reduction of the joint and placement of the screw.
History and Literature Review
As early as 1978, Palmar and colleagues tried to treat scapholunate instability with a tenodesis technique using the ERCL or ERCB. The reports led to modifications of the procedure by Glickel7 and Almquist. However, the intervention often demonstrated a loss of grip strength and wrist motion of 20 to 25% (while many still complained of pain). By 1985, Watson described fusion of the scaphoid, trapezium, and trapezoid bones (triscaphe arthrodesis) to control scaphoid rotation (with improved results in grip strength).
Other authors were not able to duplicate his clinical results, and Watson modified the procedure by including a generous radial styloidectomy to prevent radioscaphoid arthrosis.6 However, by spanning the proximal and distal carpal rows mobility was decreased 40% and complications often included nonunion. Although a fusion procedure was generally considered if the SL gap was >4mm, or if the scaphoid was nonreducible, many believed that post-traumatic arthritis was inevitable with limited arthrodeses due to the abnormal wrist kinetics.
Blatt subsequently used the dorsal capsule to tether the distal pole of the scaphoid in extension, whereas Szabo and colleagues demonstrated success utilizing the dorsal intercarpal ligament.9 Although motion appears to improve at the expense of grip strength, these reconstructions tend to fail over time (as evidenced by radiographic carpal collapse and SL widening). Long-term outcomes are not well documented, but there is cause for concern that late degeneration may occur (because the abnormal carpal alignment is not corrected). Overall, the results are variable (with soft-tissue reconstructions wherein mobility decreases 10 to 44% and strength decreases to 13 to 35% of the contralateral limb).2 Despite symptomatic improvement, Moran et al. recorded a 15% loss of motion and 20% decrease in grip strength with dorsal capsulodesis (with radiographic alignment lost at two-year follow-up).3
In 1991, Hom and Ruby attempted limited arthrodesis of the scaphoid and lunate with high rates of nonunion. However, the pseudoarthrosis rendered many patients symptom free.5 This led to Rosenwasser to decribe the RASL procedure with encouraging clinical results in early 2000 (American Society for Surgery of the Hand meeting, October 2000, Seattle, WA). The RASL has been reported to minimize the loss of grip strength and mobility 10 to 15%. The technique uses a cannulated Herbert screw to stabilize the scaphoid and lunate.
The dumbbell-shaped screw allows for some rotation, while restoring the scapholunate interval and preventing AP translation at the joint. The RASL requires two incisions: one to perform the reduction and a second for a radial styloidectomy.8 Shortly thereafter, the ARASL technique was developed using three portals to achieve similar results. Performing this procedure arthroscopically facilitates both establishing the initial diagnosis of a scapholunate injury as well as visualizing the adequacy of reduction of the scapholunate subluxation during HBS screw placement.
Anatomy and Biomechanics
The SLIL is an important intrinsic restraint that allows the scaphoid and lunate to seamlessly rotate in unison during wrist motion. As the wrist palmar or dorsiflexes, the scaphoid moves in concert with the lunate. As the wrist deviates ulnarly or radially, the scaphoid and lunate extend and flex (respectively).10 If there is an isolated SLIL rupture, the extrinsic ligamentous complex maintains the position of the scaphoid and lunate, albeit with added stress, because the two bones are no longer internally coupled. Attrition of the extrinsic restraints occurs over time, and ultimately the SL interval widens and a dorsal intercalated segment instability (DISI) pattern appears. It is important to understand that both the intrinsic SLIL and extrinsic restraints have to be compromised in order to observe radiographic abnormalities. However, symptoms can still be present despite the lack of radiographic findings. One of the advantages of using the arthroscope is the ability to assess the integrity of the SLIL.
The SLIL consists of three segments, with the ligament being the strongest and thickest dorsally. The volar portion is less robust, and the mid-substance is the weakest (being comprised of fibrocartilagenous material).2 The volar extrinsic ligaments include the radioscaphocapitate (RSC), long and short radiolunate ligaments (LRL, SRL), and the ulnotriquetral and ulnolunate ligaments. The RSC acts as a fulcrum for the scaphoid to flex and extend. Dorsally, the radiocarpal (DRC) and dorsal intercarpal (DIC) ligaments are stout restraints that prevent dorsal translation of the carpal bones.10 When the SLIL, along with any of the external ligaments, is injured the scaphoid is free to flex over the RSC and pronate. During the ARASL, adequate reduction of the rotary subluxation is achieved by dorsiflexion and supination of the scaphoid at the same time the lunate is palmar flexed. If the SL instability is allowed to go untreated, the abnormal kinematics that ensue will lead to a scapholunate advanced collapse (SLAC) deformity.1
Indications
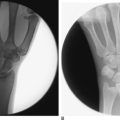
Class A injuries are the least severe (in which no radiographic signs are present). However, there is clinical suspicion of SL injury. Generally, this represents a partial simple tear of the intrinsic SL ligament and can often be treated conservatively. Class B is considered a “dynamic” state in which stress radiographic views reveal SL widening consistent with an injury to both the intrinsic and extrinsic restraints. Class C demonstrates a static SL gap on radiographs. Such injuries can be further classified into flexible and fixed deformities (Figure 9.1a and b).
Patients with a class A or “predynamic” state can be treated with splinting, pain medication, or cortisone injection until symptoms improve. However, attrition of the extrinsics may develop in which the patient will progress to class B. Patients who present with classes B and C injuries require surgical intervention to control the scaphoid instability and are candidates for the ARASL procedure. Some of the alternative methods of treatment may be contraindicated in the presence of radiocarpal arthritis. However, an early SLAC wrist does not preclude one from undergoing the ARASL coupled with a radial styloidectomy. Patients with stage II SLAC wrist have demonstrated symptomatic improvement in our small series, and the ARASL can be performed prior to considering a salvage procedure. Absolute contraindications include SLAC wrists beyond stage II.
Technique
Preparation
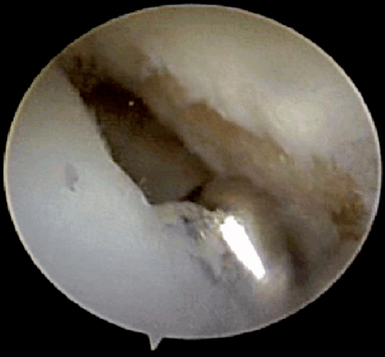
Once the diagnosis is confirmed and a “drive-through” sign is seen (Figure 9.2), the arthroscope is placed in the radial midcarpal portal. A 2.9-mm shaver is placed in the 3-/,4 portal. The adjacent articular surfaces of the scaphoid and lunate are denuded of cartilage and excoriated until punctate bleeding is seen. The surfaces are not, however, completely decorticated.
Reduction Procedure
Step 2
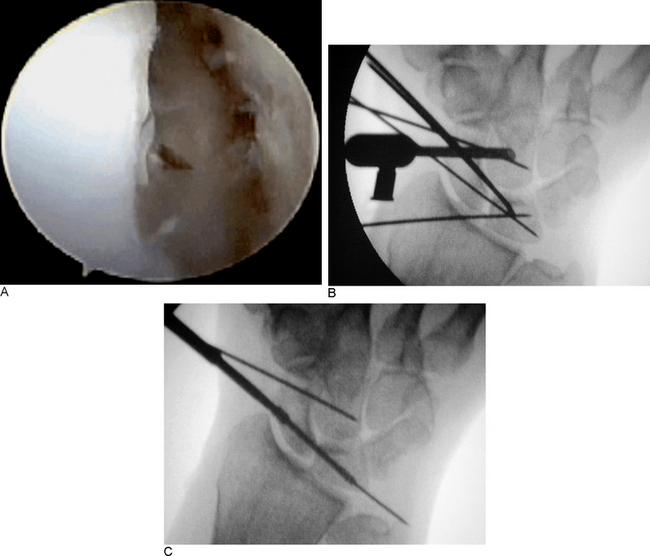
Next, a 1-/,2 portal is created just dorsal to the APL tendon. This will allow for insertion of the cannulated HBS screw guide wire. The subcutaneous tissues are spread to the capsule, and small Ragnell retractors are used to introduce a protective cannula. The entrance position of the 0.35-mm guide wire may be observed from either the 3-/,4 portal or under fluoroscopic control (Figure 9.3).
Step 3
Once the correct position is confirmed, the pin is withdrawn slightly so as not to interfere with the reduction (Figure 9.4a). The scapholunate joint is anatomically reduced by levering the K-wire in the distal pole dorsally and rotating the pin to supinate the scaphoid. The scaphoid and lunate are then firmly fixed by pinning them to the radius and capitate (Figure 9.4b). Confirming again that an anatomic reduction has been achieved, the guide pin is advanced across the scapholunate joint and advanced to the proximomedial corner of the lunate.
Step 4
Next, a new cannulated drill is used. The two scaphoid cortices are perforated. Power may be desirable to penetrate the lunate cortex to avoid pressure that could distract the joint. Once in the lunate, the drill should be advanced by hand up to the medial corner of the lunate. The position is confirmed with the image intensifier and the scapholunate joint is checked to ensure there has been no distraction (Figure 9.4c). It is helpful to compress the joint with the .062 pins during drilling to prevent distraction.
Step 5
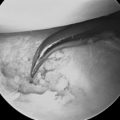
Once the drilling is completed, the screw is inserted. If the joint is well reduced, the standard compression screw is used. However, if there is any distraction the high-compression HBS screw can be used to compensate. The screw is advanced until it is barely beneath the subchondral surface of the scaphoid (Figure 9.5a through c). Motion is checked with the image intensifier while the position of the screw and reduction of the joint are confirmed. The instruments are then withdrawn and the portals closed. A short arm cast is applied.
Results
A total of seven patients (five males and two females, ages 28 to 77) were included in our study. Four patients had static deformities, whereas three had progressed to an SLAC pattern. Two patients had stage II, and one patient had a stage III SLAC pattern. Total arc of wrist motion was reduced 22.5% at a mean follow-up of 19 months. One patient, who had the SLAC III wrist, experienced a poor result (with a 47% reduction in wrist range of motion and persistent pain). This patient opted for the ARASL prior to having a salvage procedure to minimize her worsening mobility. Without this poor result, the mean reduction in wrist range of motion for the remaining six patients was 17.6%. Radiographically, the mean SL distance was reduced from 4.2 to 1.75 mm and the mean SL angle was reduced from 81.6 to 61.8 degrees.
1 Watson HK, Ballet FL. The SLAC wrist: Scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg [Am]. 1984;9:358-365.
2 Bloom HT, Freeland AE, Bowen V, Makonjic L. The treatment of chronic scapholunate dissociation: An evidence-based assessment of the literature. Orthopedics. 2003;26:195-203.
3 Moran SL, Cooney, Berger RA, Strickland J. Capsulodesis for the treatment of chronic scapholunate instability. J Hand Surg [Am]. 2005;30:16-23.
4 Brunelli GA, Brunelli GR. A new technique to correct carpal instability with scaphoid rotary subluxation: A preliminary report. J Hand Surg [Am]. 1995;20:S82-S85.
5 Hom S, Ruby LK. Attempted scapholunate arthrodesis for chronic scapholunate dissociation. J Hand Surg [Am]. 1991;16:334-339.
6 Watson HK, Ryu J, Akelman E. Limited triscaphoid intercarpal arthrodesis for rotatory subluxation of the scaphoid. J Bone Joint Surg [Am]. 1986;68:345-349.
7 Glickel SZ, Millender LH. Ligamentous reconstruction for chronic intercarpal instability. J Hand Surg [Am]. 1984;9:514-527.
8 Lipton CB, Ugwonali OF, Sarwahi V, Chao JD, Rosenwasser MP. Reduction and association of the scaphoid and lunate for scapholunate ligament injuries (RASL). Atlas Hand Clin. 2003;8:249-260.
9 Szabo RM, Slater PRJr., Palumbo CF, Gerlach T. Dorsal intercarpal ligament capsulodesis for chronic, static scapholunate dissociation: Clinical results. J Hand Surg [Am]. 2002;27:978-984.
10 Wolfe SW, Neu C, Crisco JJ. In vivo scaphoid, lunate and capitate kinematics flexion and extension. J Hand Surg [Am]. 2000;5:860-869.