CHAPTER 24 Arthroscopic Radial Styloidectomy
Introduction
Radial styloidectomy has typically been employed as a palliative procedure for any condition that results in painful impingement between the scaphoid and the radial styloid. It is most attractive to patients who wish minimal surgical intervention, but it does not address the underlying cause and hence may not be a long-term solution. Recommendations for the amount of bony resection have become more conservative with time due to several biomechanical studies that demonstrated increasing radial instability, with the risk of ulnar translocation and progressive loss of the strong volar radiocarpal ligaments.1,2
Osterman has written extensively on an arthroscopic technique that not only allows an assessment of the joint surfaces but allows one to visualize and preserve these crucial volar ligaments.3–5 The arthroscopic procedure may carry less risk of injury to the superficial radial nerve branches, with less pain compared to an open procedure.
Indications
The indications for an arthroscopic radial styloidectomy are similar to the open procedure. Radial styloid impingement due to radioscaphoid arthritis is a common indication. This is often a consequence of long-standing scapholunate dissociation or end-stage Kienbock’s disease. Culp et al. suggest that patients who have painful radial deviation and a positive Watson test but have preserved wrist motion and good grip strength are ideal candidates.6 Chronic scaphoid nonunion, in which the hypertrophic distal scaphoid fragment impinges against the radial styloid during wrist radial deviation, is another common indication. If an attempt is made to internally fix the scaphoid, this impingement must be addressed. Resection of the distal scaphoid fragment will obviate the need for a radial styloidectomy.7
Secondary radial styloid impingement is a common sequella of a scaphotrapeziotrapezoidal (STT) fusion when it is used to treat rotary subluxation of the scaphoid or scaphotrapezialosteoarthritis (OA). Watson observed this in more than a third of his patients and now recommends a radial styloidectomy at the time of STT fusion.8 Impingement may also occur following a capitolunate fusion, which should be checked for at the time of surgery.9 Occasionally a limited styloidectomy is performed at the time of a proximal row carpectomy for treatment of radiocarpal OA.10
Contraindications
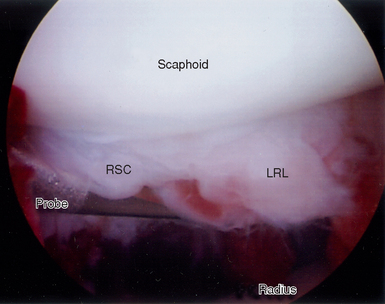
The main risk following a radial styloidectomy is ulnar translocation of the carpus. Siegal and Gelberman showed that short oblique osteotomies were the least destructive, whereas vertical oblique and horizontal osteotomies removed 92 to 95% of the radioscaphocapitate (RSC) ligament and 21 to 46% of the long radiolunate ligament (LRL).2 Cooney and coauthors emphasized the importance of the RSC and LRL ligaments in preventing ulnar translocation. If too much of these ligaments is removed, the capitate is destabilized and no longer rests in the lunate fossa—resulting in radial instability. Biomechanical testing revealed a significant increase in radial translation under loading when ≥6 mm or the radial styloid was excised.
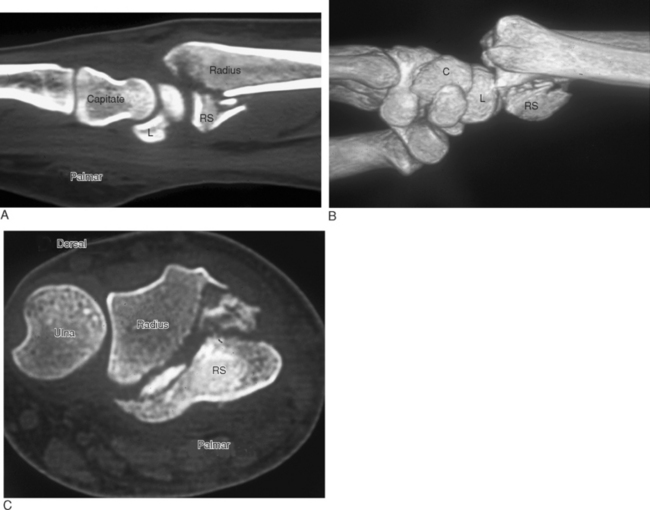
Some specimens demonstrated moderate to severe palmar and ulnar translation. They recommended limiting the bony resection to no more than 4 mm to minimize this risk.1 Patients who do not have an intact RSC ligament due to distal radius fracture11 (Figure 24.1a through c) or radiocarpal dislocation (Figure 24.2)12–14 are at risk for ulnar translocation and are not candidates for this procedure, especially if a proximal row carpectomy is contemplated.15 Ulnar translocation is a frequent sequella of long-standing rheumatoid disease. Hence, any patient with chronic wrist involvement is a poor candidate for this procedure.
Equipment
A 2.7-mm 30-degree angled scope along with a camera attachment is used. A 2.9-mm bur and/or a 4.0-mm abrader is integral to the procedure. A small osteotome may also be useful. An overhead traction tower greatly facilitates instrumentation. The use of a motorized shaver is needed for debridement. Some type of diathermy unit may be useful, as well as arthroscopic straight and curved knives for lysis of adhesions. Intraoperative fluoroscopy is employed to assess the adequacy of bone resection.
Surgical Technique
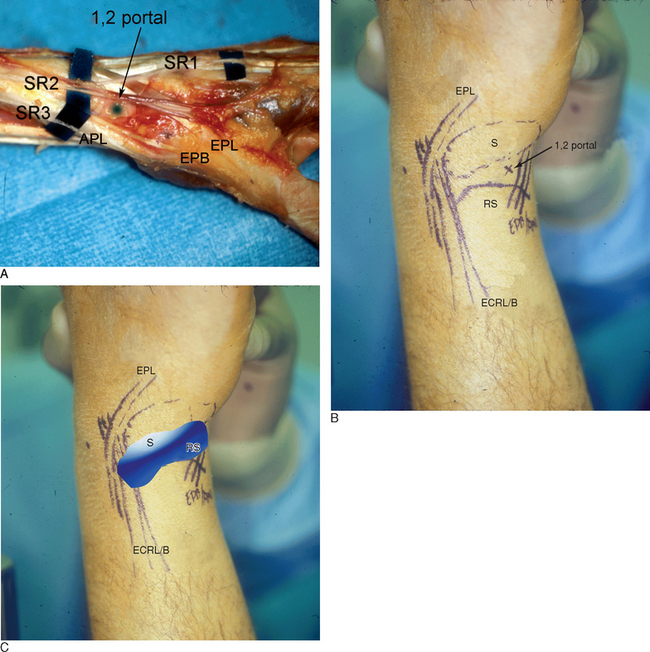
This is one procedure in which the 1-/,2 portal is particularly helpful. The patient is positioned supine on the operating table, with the arm extended on a hand table. The fingers are suspended by Chinese finger traps with 10 to 15 pounds of countertraction. The relevant landmarks in the snuffbox are palpated and outlined, including the distal edge of the radial styloid, the abductor pollicis longus (APL), the extensor pollicis brevis (EPB) and extensor pollicis longus EPL tendons, and the radial artery in the snuffbox (Figure 24.3a through c). A tourniquet is elevated to 250 mmHg.
To minimize the risk of injury to branches of the superficial radial nerve and the radial artery, the 1-/,2 portal should be placed more palmar and proximal in the snuffbox. The entry site is outlined no more than 4.5 mm dorsal to the first extensor compartment and within 4.5 mm of the radial styloid.16 A 22-gauge needle is used to identify the joint space, followed by a small superficial skin incision. The tissue is spread down to the capsule, which is pierced by tenotomy scissors. A cannula and blunt trocar are inserted with the wrist in ulnar deviation to minimize damage to the proximal scaphoid, followed by a 3-mm hook probe.
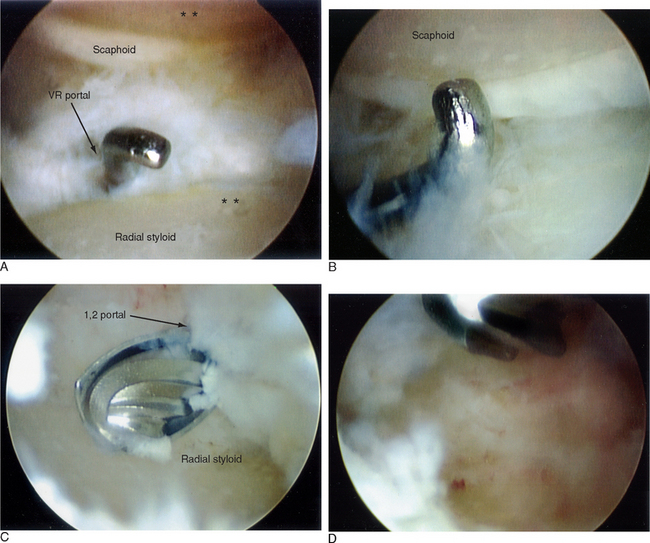
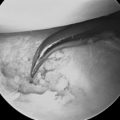
A 3-/,4 working portal is established in a similar fashion. The author uses the volar radial (VR) portal interchangeably with the 3-/,4 portal for viewing and instrumentation in order to gain complete access to the dorsoradial aspect of the styloid (Figure 24.4a through d). A large-bore outflow cannula in the 4-/,5 or 6-U portal is desirable. A standard radiocarpal and midcarpal survey are performed, with debridement and synovectomy as necessary. With the arthroscope in the 3-/,4 portal, the origins of the RSC and LRL on the distal radius are noted—which mark the ulnar extent of the resection. The diameter of the bur will give a rough guide as to the amount of bony resection, but this needs to be confirmed fluoroscopically.
Various authors recommend from 4 to 7 mm of resection. The degree of bony resection should, however, be tailored to the individual and gauged at the time of surgery. Enough bone should be resected so that there is no residual impingement between the scaphoid and the radial styloid when the wrist is radially deviated with the traction released (Figure 24.5a and b). A small osteotome should be used judiciously because inadvertent penetration of the radial joint capsule carries the risk of radial artery perforation as it traverses the snuffbox.
Postoperative Management
The patient is placed in a removable below-elbow splint for comfort, and protected wrist motion is instituted after the first week. Gradual strengthening exercises are added as tolerated by the third to fourth week.
Results
Open radial styloidectomies have been employed for more than 50 years. Arthroscopic techniques are more recent. Because it is often used in combination with other procedures, reports of isolated styloidectomies are scant. Similarly, there are no large series on arthroscopic resection. Some investigators have reported pain relief and improved wrist motion following internal fixation of scaphoid nonunions when combined with an open radial styloidectomy for arthritic changes.17 Stark and coauthors found that the principal benefit obtained was pain relief rather than increased motion or grip strength.18 Radial styloidectomy has been implicated as a causative factor in persistent scaphoid nonunion following internal fixation.19
1 Nakamura T, Cooney WPIII, Lui WH, et al. Radial styloid-ectomy: A biomechanical study on stability of the wrist joint. J Hand Surg [Am]. 2001;26:85-93.
2 Siegel DB, Gelberman RH. Radial styloidectomy: An anatomical study with special reference to radiocarpal intracapsular ligamentous morphology. J Hand Surg [Am]. 1991;16:40-44.
3 Yao J, Osterman AL. Arthroscopic techniques for wrist arthritis (radial styloidectomy and proximal pole hamate excisions). Hand Clin. 2005;21:519-526.
4 Gupta R, Bozentka DJ, Osterman AL. Wrist arthroscopy: Principles and clinical applications. J Am Acad Orthop Surg. 2001;9:200-209.
5 Osterman A. Wrist arthroscopy: Operative procedures. In: Green DP, Pederson WC, editors. Green’s Operative Hand Surgery. Fourth Edition. Philadelphia: Churchill Livingstone; 1999:207-222.
6 Culp RW. Operative wrist arthroscopy. In: Green DP, Pederson WC, Wolfe SW, editors. Green’s Operative Hand Surgery. Fifth Edition. Philadelphia: Churchill Livingstone; 2005:798.
7 Ruch DS, Papadonikolakis A. Resection of the scaphoid distal pole for symptomatic scaphoid nonunion after failed previous surgical treatment. J Hand Surg [Am]. 2006;31:588-593.
8 Rogers WD, Watson HK. Radial styloid impingement after triscaphe arthrodesis. J Hand Surg [Am]. 1989;14:297-301.
9 Calandruccio JHGR. SLAC wrist: Capitolunate fusion with scaphoid and triquetrum excision. In: Gelberman R, editor. Master Techniques in Orthopedic Surgery: The Wrist. Philadelphia: Lippincott Williams & Wilkins; 2002:234.
10 Van Heest AEHJ. Proximal row carpectomy. In: Gelberman R, editor. Master Techniques in Orthopedic Surgery: The Wrist. Philadelphia: Lippincott Williams & Wilkins; 2002:37-47.
11 Schoenecker PL, Gilula LA, Shively RA, Manske PR. Radiocarpal fracture: Dislocation. Clin Orthop Relat Res. 1985:237-244.
12 Jebson PJ, Adams BD, Meletiou SD. Ulnar translocation instability of the carpus after a dorsal radiocarpal dislocation: A case report. Am J Orthop. 2000;29:462-464.
13 Howard RF, Slawski DP, Gilula LA. Isolated palmar radiocarpal dislocation and ulnar translocation: A case report and review of the literature. J Hand Surg [Am]. 1997;22:78-82.
14 Dumontier C, Meyer zu Reckendorf G, Sautet A, et al. Radiocarpal dislocations: Classification and proposal for treatment. A review of twenty-seven cases. J Bone Joint Surg Am. 2001;83-A:212-218.
15 van Kooten EO, Coster E, Segers MJ, Ritt MJ. Early proximal row carpectomy after severe carpal trauma. Injury. 2005;36:1226-1232.
16 Steinberg BD, Plancher KD, Idler RS. Percutaneous Kirschner wire fixation through the snuff box: An anatomic study. J Hand Surg [Am]. 1995;20:57-62.
17 Herness D, Posner MA. Some aspects of bone grafting for non-union of the carpal navicular. Analysis of 41 cases. Acta Orthop Scand. 1977;48:373-378.
18 Stark HH, Rickard TA, Zemel NP, Ashworth CR. Treatment of ununited fractures of the scaphoid by iliac bone grafts and Kirschner-wire fixation. J Bone Joint Surg Am. 1988;70:982-991.
19 Schuind F, Haentjens P, Van Innis F, et al. Prognostic factors in the treatment of carpal scaphoid nonunions. J Hand Surg [Am]. 1999;24:761-776.