CHAPTER 10 Arthroscopic Radial Head Resection
Radial head resection is a useful treatment alternative for symptomatic radiocapitellar or proximal radioulnar joint pathology. Radial head excision may improve forearm rotation and reduce impingement between the radial head and the capitellum or proximal ulna. Most reports in the literature involve open radial head resection.1 Arthroscopic radial head resection has been described only recently,2 and reports of outcomes are limited.3–5 However, as experience with arthroscopic radial head resection continues to increase, we expect more evidence to be forthcoming.
ANATOMY AND BIOMECHANICS
The radial head is an important stabilizer of the elbow. A number of biomechanical studies have investigated the effect of radial head resection on the kinematics and stability of the elbow. The radial head is particularly important as a stabilizer in the setting of valgus instability due to medial collateral ligament insufficiency.6–9 It is also important in tensioning the lateral collateral ligament,7 and posterolateral rotatory instability has been reported after radial head excision in vitro7,10 and clinically.11,12 The role of the radial head in axial stability of the forearm is evident by the common finding of proximal migration of the radius after radial head resection.13–17
Radial head excision results in increased loading of the remaining ulnohumeral articulation. This effect is caused by the altered elbow kinematics and the fact that the loads originally borne by the radiocapitellar articulation must be accepted by the ulnohumeral joint.8 Although this increased ulnohumeral load has not been studied biomechanically, it is thought to explain the high incidence of ulnohumeral osteoarthritis reported in patients after acute radial head resection for radial head fractures.14–17 Extensive biomechanical evidence supports the beneficial stabilizing effects of prosthetic replacement of the radial head.7–9,18,19 These findings suggest that, whenever possible, the radial head should be replaced after it is resected, particularly in cases of acute trauma, in which occult ligament injuries are common.
PATIENT EVALUATION
History and Physical Examination
A detailed physical examination should be performed. The carrying angle and bony contours of the elbow should be observed. Prior traumatic and surgical incisions should be documented. The range of motion of the elbow and forearm should be measured with the use of a goniometer. The examiner should confirm that the proximal radius articular deformity is the impediment to rotation. Motion can be lost as a result of soft tissue or osseous deformities. The synovial tissue in patients with hemophilic arthropathy is hypertrophic, highly vascular, and prone to impingement between the articular surfaces.22 A soft end point suggests a soft tissue cause, whereas a firm end point suggests osseous impingement. The distal radioulnar joint may be contributing to the forearm rotational stiffness.
Physical examination and imaging of the wrist are important, especially in patients with prior traumatic injuries, congenital deformities, and rheumatoid arthritis, in which distal radioulnar joint pathology is common. A careful examination of elbow and forearm stability is critical because valgus, posterolateral rotational, and axial instability are contraindications to radial head resection. Joint laxity may be caused by loss of articular cartilage, ligament attenuation resulting from chronic inflammation, or prior traumatic injuries. The examination for valgus instability includes valgus stress testing,26,27 the milking maneuver,28 and the moving valgus stress test.29 The examination for posterolateral rotatory instability includes the pivot shift test,12 the posterolateral drawer test,30 and the supine and seated push-up tests.31,32 Longitudinal radioulnar instability is difficult to detect on clinical examination. These patients often have tenderness or dorsal prominence of the ulna at the distal radioulnar joint.
Diagnostic Imaging
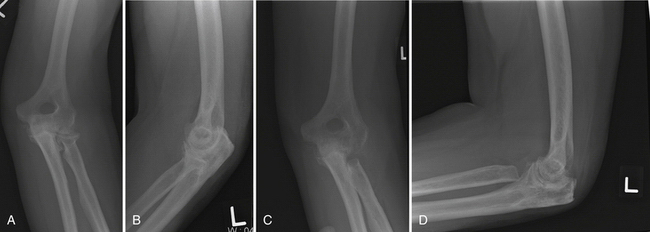
Imaging can confirm the presence of a proximal radius articular deformity or arthritis (Fig. 10-1). In addition to anteroposterior and lateral views, a radiocapitellar view can help to throw the radial head into profile. Bilateral radiographs of the wrists should be performed to assess for other contributions to the painful or limited rotation, such as radioulnar synostosis or distal radioulnar joint pathology, and to assess for longitudinal radioulnar dissociation. Stress views or a fluoroscopic examination should be considered to rule out valgus, varus, and axial instability if there is any concern resulting from the physical examination. Computed tomography (CT) with sagittal, coronal, and three-dimensional reconstructions can better define the bony anatomy (Fig. 10-2). CT may offer additional information about the ulnohumeral, radiocapitellar, and proximal radioulnar joint spaces and about articular congruity. Loose bodies and heterotopic ossification also may be better defined. Resecting the radial head without addressing these other osseous deformities may result in suboptimal results.
TREATMENT
Indications and Contraindications
The most common conditions for which arthroscopic radial head resection has been described are rheumatoid arthritis3–5,20,21 and post-traumatic arthritis (particularly radial head fractures).2–5,20,21 Radial head resection is sometimes indicated for hemophilic arthropathy of the elbow. Chronic hemophilic synovitis of the elbow can lead to enlargement and irregularity of the radial head. The margins of this hypertrophic radial head impinge against the proximal ulnar facet, acting as a mechanical block to forearm rotation. Reports in the literature of radial head resection for hemophilic arthropathy are limited to open techniques.22–25 Congenital and acquired radial head dislocations can also be treated by arthroscopic radial head resection in selected cases. Surgical intervention is typically reserved for symptoms refractory to nonoperative measures, such as activity modification and anti-inflammatory drugs. In the setting of rheumatoid arthritis, this includes an adequate trial of disease-modifying medications.
Radial head excision is contraindicated in patients with valgus, posterolateral rotatory, or axial instability. The loss of this secondary stabilizer can exacerbate preexisting instability. Advanced ulnohumeral arthritis is a relative contraindication because radial head excision alone cannot address symptoms originating from the ulnohumeral articulation. Radial head excision results in increased loading of the remaining ulnohumeral articulation, which may further exacerbate ulnohumeral joint pain.8 Radial head replacement and radiocapitellar replacement can be considered when isolated radial head excision is contraindicated, such as in the setting of instability.33 Older, lower-demand patients with advanced articular destruction and bony deformity may be better treated with a total elbow arthroplasty. Arthroscopic excision of the radial head usually is not recommended for acute radial head fractures because of the high incidence of concomitant ligament injuries.34,35 The torn capsule in the acute fracture setting can result in significant extravasation of fluid, making it a higher-risk procedure and more technically challenging.
A surgeon’s inexperience with arthroscopy of synovitic elbows can be considered a relative contraindication. Arthroscopy of synovitic elbows is technically demanding because synovial proliferation, stiffness, and deformity result in diminished capsular volume, reducing the available working room in the elbow.36 An inexperienced surgeon may better manage these patients with open surgery because of the increased risk of nerve injuries in the setting of inflammatory arthritis.37
Alternative Treatments
Retention of the radial head should be considered in most patients undergoing synovectomy and débridement for rheumatoid and primary osteoarthritis unless there is severe deformity interfering with rotation or there are symptoms specifically referable to the radial head. Removing the stabilizing effect of the radial head can result in long-term overload of the medial collateral ligament, valgus instability, posterolateral rotatory instability, proximal migration of the radius, and progressive articular destruction due to increased ulnohumeral loading.38,39 Although not well studied, radial head contouring has been used by some surgeons in the setting of rheumatoid arthritis with the aim of improved forearm rotation.38
If radial head resection is deemed necessary, radial head replacement can preserve the stabilizing effect of the radial head.7–9,18,19 However, radial head replacement is not ideal if there is anticipated maltracking of a prosthetic radial head, as seen in the setting of chronic subluxation or dislocation of the proximal radioulnar joint. Likewise, a significantly deformed native capitellum may become a pain generator if it articulates with a radial head hemiarthroplasty, making excision without replacement more ideal in that setting. Radiocapitellar prostheses have recently become available but have not been extensively studied.
Arthroscopic Technique
General anesthesia is typically employed. In patients with more severe stiffness and advanced articular damage, a continuous brachial plexus block is useful for postoperative pain control and early mobilization. Standard elbow arthroscopic positioning, equipment, and portals are used. We prefer a lateral decubitus position with the arm positioned over a well-padded bolster. Gravity inflow is used to maintain low pressures to avoid excessive joint swelling. A 4.0-mm arthroscope is used for visualization. The initial view after arthroscope insertion is often poor because of extensive synovitis. A full radius resector is used for synovectomy as needed for visualization (see Chapter 11). In addition to the radial head deformity, the entire elbow should be inspected for the presence of associated abnormalities, such as cartilage defects of the capitellum, synovitis, loose bodies, and capsular contracture.
PEARLS& PITFALLS
PEARLS
Postoperative Management
Postoperative management involves discharge from the hospital on the same day and immediate active range of motion as tolerated. If a concomitant contracture release is performed, the patient is admitted for a continuous regional block for the first few days, combined with immediate rehabilitation efforts with a continuous passive motion device. Indomethacin (25 mg three times daily for 3 weeks) should be considered to reduce the incidence of heterotopic ossification in patients who do not have a contraindication to this medication.40
OUTCOMES
Our understanding of the outcomes of arthroscopic radial head resection is based largely on our experience with open radial head resection. The available literature on arthroscopic resection is limited to very few cases with only short-term follow-up.2–5 There are no published clinical trials comparing the outcomes of open versus arthroscopic radial head resection.
McLaughlin and colleagues3 reported the largest published series of arthroscopic radial head resections. They reviewed 36 patients who underwent surgery for radiocapitellar joint arthritis at a mean age of 46 years and had a mean follow-up of 52 months. Radiocapitellar arthrosis was caused by post-traumatic radial head fracture in 17 patients, primary osteoarthritis beginning with the radiocapitellar joint in 10 patients, rheumatoid arthritis with radiocapitellar subluxation in 3 patients, arthrofibrosis in 2 patients, and osteonecrosis, psoriatic arthritis, post-radial head fracture synostosis, and acute radial head fracture in 1 patient each. Eight patients underwent arthroscopic radial head resection alone, and the remaining 26 patients underwent a concurrent arthroscopic modification of the Outerbridge-Kashiwagi procedure, which was added if there was concurrent ulnohumeral arthritis. Both groups had similar flexion-extension loss preoperatively. They found that isolated radial head excision resulted in an increased flexion-extension arc averaging 62 degrees, whereas the average was 46 degrees with the combined procedure. Similarly, patients who underwent radial head excision alone had a greater increase in functional scores. All of the eight patients who underwent radial head excision alone were satisfied with the procedure and reported significant pain relief. The study authors concluded that patients treated early in the disease process had greater success overall than those who chose to receive later treatment. Two patients required additional surgery. One required a flexion contracture release, and one underwent radial head replacement for continued pain after excision of the radial head associated with proximal migration of the radial shaft.
Menth-Chiari and coworkers4 reported a series of 12 patients (10 with post-traumatic arthrosis secondary to radial head fractures and 2 with rheumatoid arthritis) who underwent arthroscopic radial head resections. The average age was 38.5 years, and the mean follow-up was 39 months. Their indication for surgery was chronic mechanical elbow pain with arthroscopic findings of radiocapitellar arthritis primarily involving the radial head. Limitation in range of motion was not a major indication in this series. Eleven of 12 patients were satisfied with the procedure and experienced improved pain, mechanical symptoms, and range of motion. One patient who underwent partial radial head resection suffered from radiocapitellar impingement. Range of motion improved in all patients. The flexion arc improved from a preoperative mean of 23 to 110 degrees to a postoperative mean of 9 to 136 degrees. Preoperatively, two patients had limited pronation (both lacking 5 degrees), and two had limited supination (lacking 15 degrees in one and 30 degrees the other). All patients had full rotation postoperatively. The only complications identified were a moderate loss of strength (that did not interfere with activities of daily living) in three patients and proximal radial migration of 2 and 3 mm in two patients. There was no objective or subjective evidence of elbow instability, cubitus valgus, heterotopic ossification, infection, nerve injury, or vascular injury.
Savoie and associates5 reported on series of 24 patients treated with an arthroscopic modification of the open Outerbridge-Kashiwagi procedure. Their indication was a painful arthritic elbow with restricted motion refractory to nonoperative treatment. The primary diagnosis was post-traumatic arthritis in 15 patients, rheumatoid arthritis in 5 patients, and primary osteoarthritis in 4 patients. The average age was 59 years, and the mean follow-up was 32 months. The technique they described included arthroscopic synovectomy, débridement, osteophyte removal, olecranon fossa fenestration, and radial head resection when indicated. The radial head was excised arthroscopically in 18 of the 24 patients. They found an increase in range of motion and a significant relief of pain in all of their patients, with 23 of 24 patients being satisfied with their results. The flexion arc improved from a preoperative mean of 40 to 90 degrees to a postoperative mean of 8 to 139 degrees. The 13% complication rate included a superficial infection in one patient, heterotopic ossification in one patient, and recurrent effusions in two patients. There was no report of late instability. One patient who did not undergo radial head resection continued to have radiocapitellar symptoms and required a radial head resection later. Because this study reported the results of treatment of the entire arthritic elbow (i.e., radiocapitellar, proximal radioulnar, and ulnohumeral articulations), it is difficult to extrapolate how much of the improvements seen can be attributed to the radial head resection alone or to the extensive joint débridement and capsulectomy.
These three small series comprise the bulk of information available about the results of arthroscopic radial head resection. However, there are numerous studies documenting the beneficial effects of open radial head excision and synovectomy in early to moderate rheumatoid arthritis.1,41–49 Improvement in rotation has been consistently reported in this setting.1 The beneficial effect deteriorates with time, and the procedure seems to fail more quickly in patients with valgus instability after excision of the radial head.21 Radial head excision unbalances the elbow, concentrating stress on the lateral portion of the ulnohumeral articulation and thereby potentially accelerating degenerative wear.
Gendi and colleagues42 reported the largest series of open radial head resections for rheumatoid arthritis. Of 115 patients treated by open synovectomy, 113 had a concomitant radial head resection. The average age was 55 years, and the mean follow-up was 6.5 years. The investigators reported a 19% failure rate during the first year and a decline in survival averaging 2.6% per year. Forearm rotation improved by 50 degrees, whereas the flexion-extension range improved by only 10 degrees compared with the preoperative state. Preoperative forearm rotation of less than 50% of normal and preservation of preoperative flexion-extension range were predictors of success. Complications included instability in 18% and recurrent synovitis in 43%, both of which were associated with poor outcomes.
Arthroscopic radial head excision will likely have complications similar to those reported after open resection, including cubitus valgus, proximal radial migration, distal radioulnar joint symptoms, posterolateral rotatory instability, residual radiocapitellar or proximal radioulnar impingement due to inadequate resection, loss of strength, degenerative osteoarthritis, heterotopic ossification, and nerve injury.11,38,39,50 Although neurovascular structures are at risk with arthroscopic and open procedures, joint distention, the use of retractors, and careful portal placement should reduce the proximity of these structures and thereby reduce the incidence of injury.
CONCLUSIONS
Radial head resection is uncommonly indicated. Surgeons should aim to preserve or replace the radial head when possible to maintain the stability of the elbow and prevent late complications. Elbow instability must be assessed preoperatively, and radial head resection should be avoided if present. Arthroscopic radial head resection may offer theoretical benefits over open resection, such as less injury to the lateral collateral and annular ligaments, an earlier return of function, and less stiffness due to the less invasive surgical approach. However, comparative evidence in the literature is lacking. Much of what we know about the outcomes of arthroscopic radial head resection is extrapolated from our knowledge of open resections. Although complications associated with radial head resection are well recognized, resection of the radial head in selected patients with painful, deformed, and arthritic joints can be rewarding.
1. Lee BPH, Morrey BF. Synovectomy of the elbow. In: Morrey BF, editor. The Elbow and Its Disorders. 3rd ed. Philadelphia, PA: WB Saunders; 2000:708-717.
2. Lo IK, King GJ. Arthroscopic radial head excision. Arthroscopy. 1994;10:689-692.
3. McLaughlin RE, Savoie FH 3rd, Field LD, Ramsey JR. Arthroscopic treatment of the arthritic elbow due to primary radiocapitellar arthritis. Arthroscopy. 2006;22:63-69.
4. Menth-Chiari WA, Ruch DS, Poehling GG. Arthroscopic excision of the radial head: clinical outcome in 12 patients with post-traumatic arthritis after fracture of the radial head or rheumatoid arthritis. Arthroscopy. 2001;17:918-923.
5. Savoie FH 3rd, Nunley PD, Field LD. Arthroscopic management of the arthritic elbow: indications, technique, and results. J Shoulder Elbow Surg. 1999;8:214-219.
6. Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop. 1991;265:187-195.
7. Beingessner DM, Dunning CE, Gordon KE, et al. The effect of radial head excision and arthroplasty on elbow kinematics and stability. J Bone Joint Surg Am. 2004;86:1730-1739.
8. Johnson JA, Beingessner DM, Gordon KD, et al. Kinematics and stability of the fractured and implant-reconstructed radial head. J Shoulder Elbow Surg. 2005;14:195S-201S.
9. King GJ, Zarzour ZD, Rath DA, et al. Metallic radial head arthroplasty improves valgus stability of the elbow. Clin Orthop Relat Res. 1999;368:114-125.
10. Jensen SL, Olsen BS, Søjbjerg JO. Elbow joint kinematics after excision of the radial head. J Shoulder Elbow Surg. 1999;8:238-241.
11. Hall JA, McKee MD. Posterolateral rotatory instability of the elbow following radial head resection. J Bone Joint Surg Am. 2005;87A:1571-1579.
12. O’Driscoll SW, Bell DF, Morrey BF. Posterolateral rotatory instability of the elbow. J Bone Joint Surg Am. 1991;73:440-446.
13. Morrey BF, Chao EY, Hui FC. Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am. 1979;61:63-68.
14. Ikeda M, Oka Y. Function after early radial head resection for fracture: a retrospective evaluation of 15 patients followed for 3-18 years. Acta Orthop Scand. 2000;71:191-194.
15. Janssen RP, Vegter J. Resection of the radial head after Mason type-III fractures of the elbow: follow-up at 16 to 30 years. J Bone Joint Surg Br. 1998;80:231-233.
16. Leppilahti J, Jalovaara P. Early excision of the radial head for fracture. Int Orthop. 2000;24:160-162.
17. Stephen IB. Excision of the radial head for closed fracture. Acta Orthop Scand. 1981;52:409-412.
18. Pomianowski S, Morrey BF, Neale PG, et al. Contribution of monoblock and bipolar radial head prostheses to valgus stability of the elbow. J Bone Joint Surg Am. 2001;83:1829-1834.
19. Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg Am. 2004;86A:975-982.
20. Menth-Chiari WA, Poehling GG, Ruch DS. Arthroscopic resection of the radial head. Arthroscopy. 1999;15:226-230.
21. Steinmann SP, King GJW, Savoie FH. Arthroscopic treatment of the arthritic elbow. Instr Course Lect. 2006;55:109-117.
22. Silva M, Luck JV. Radial head excision and synovectomy in patients with hemophilia. J Bone Joint Surg Am. 2007;89:2156-2162.
23. Luck JVJr, Kasper CK. Surgical management of advanced hemophilic arthropathy. An overview of 20 years’ experience. Clin Orthop Relat Res. 1989;242:60-82.
24. Lofqvist T, Nilsson IM, Petersson C. Orthopaedic surgery in hemophilia: 20 years’ experience in Sweden. Clin Orthop Relat Res 1996. 1996;332:232-241.
25. Rodriguez-Merchan EC, Magallon M, Galindo E, Lopez-Cabarcos C. Hemophilic synovitis of the knee and the elbow. Clin Orthop Relat Res. 1997;343:47-53.
26. Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68:1158-1163.
27. Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9:99-113.
28. Veltri DM, O’Brien SJ, Field LD, et al. The milking maneuver: a new test to evaluate the MCL of the elbow in the throwing athlete, Programs and Abstracts of the 10th Open Meeting of the American Shoulder and Elbow Surgeons. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1994.
29. O’Driscoll SWM, Lawton RL, Smith AM. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med. 2005;33:231-239.
30. O’Driscoll SW. Classification and spectrum of elbow instability: recurrent instability. In: Morrey BF, ed. The Elbow and its Disorders.. 2nd ed. Philadelphia, PA: WB Saunders; 1993:453-463.
31. Regan WD, Morrey BF. The physical examination of the elbow. In: Morrey BF, editor. The Elbow and its Disorders. 2nd ed. Philadelphia, PA: WB Saunders; 1993:73-85.
32. Regan W, Lapner PC. Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J Shoulder Elbow Surg. 2006;15:344-346.
33. Shore BJ, Mozzon JB, MacDermid JC, et al. Chronic posttraumatic elbow disorders treated with metallic radial head arthroplasty. J Bone Joint Surg Am. 2008;90:271-280.
34. van Riet RP, Morrey BF. Documentation of associated injuries occurring with radial head fracture. Clin Orthop Relat Res. 2008;466:130-134.
35. Itamura J, Roidis N, Mirzayan R, et al. Radial head fractures: MRI evaluation of associated injuries. J Shoulder Elbow Surg. 2005;14:421-424.
36. Gallay SH, Richards RR, O’Driscoll SW. Intra-articular capacity and compliance of stiff and normal elbows. Arthroscopy. 1993;9:9-13.
37. Kelly EW, Morrey BF, O’Driscoll SW. Complications of elbow arthroscopy. J Bone Joint Surg Am. 2001;83A:25-34.
38. Kauffman JI, Chen AL, Stuchin S, Di Cesare PE. Surgical management of the rheumatoid elbow. J Am Acad Orthop Surg. 2003;11:100-108.
39. Morrey BF. Radial head fracture. In: Morrey BF, editor. The Elbow and Its Disorders.. 3rd ed. Philadelphia, PA: WB Saunders; 2000:341-364.
40. Gofton WT, King GJ. Heterotopic ossification following elbow arthroscopy. Arthroscopy. 2001;17:E2.
41. Woods DA, Williams JR, Gendi NS, et al. Surgery for rheumatoid arthritis of the elbow: a comparison of radial-head excision and synovectomy with total elbow replacement. J Shoulder Elbow Surg. 1999;8:291-295.
42. Gendi NST, Azon JMC, Carr AJ, et al. Synovectomy of the elbow and radial head excision in rheumatoid arthritis. J Bone Joint Surg Br. 1997;79B:918-923.
43. Lonner JH, Stuchin SA. Synovectomy, radial head excision, and anterior capsular release in stage III inflammatory arthritis of the elbow. J Hand Surg Am. 1997;22A:279-285.
44. Ferlic DC, Patchett CE, Clayton ML, Freemand AC. Elbow synovectomy in rheumatoid arthritis. Long-term results. Clin Orthop Relat Res. 1987;220:119-225.
45. Maenpaa HM, Kuusela PP, Kaarela K, et al. Reoperation rate after elbow synovectomy in rheumatoid arthritis. J Shoulder Elbow Surg. 2003;12:480-483.
46. Makai F, Chudacek J. Hamalainen M, Hagena FW, eds. Rheumatoid Surgery of the Elbow. Hamalainen M, Hagena FW, editors, Long-term results of synovectomy of the elbow with excision of the radial head in rheumatoid arthritis. Vol. 15, Basel, Switzerland: Karger; 1991:22-26.
47. Tulp NJ, Winia WP. Synovectomy of the elbow in rheumatoid arthritis: long-term results. J Bone Joint Surg Br. 1989;71:664-666.
48. Taylor AR, Mukerjea SK, Rana NA. Excision of the head of the radius in rheumatoid arthritis. J Bone Joint Surg Br. 1976;58:485.
49. Rymaszewski LA, Mackay I, Amis AA, Miller JH. Long-term effects of excision of the radial head in rheumatoid arthritis. J Bone Joint Surg Br. 1984;66:109-113.
50. Morrey BF, Schneeberger AG. Anconeus arthroplasty: a new technique for reconstruction of the radiocapitellar and/or proximal radioulnar joint. J Bone Joint Surg Am. 2002;84:1960-1969.