CHAPTER 26 Arthroscopic Proximal Row Carpectomy
Introduction
Proximal row carpectomy is a motion-sparing salvage procedure that consists of excising the scaphoid, lunate, and capitate—thus converting a complex link joint into a simple hinge.1 Although the procedure has historically been criticized for loss of motion and strength, progressive radio capitate arthritis, and unpredictability of outcome, much of this criticism has been anecdotal.2 Recent studies, including three series with a minimum of nine years of follow-up, have demonstrated that proximal row carpectomy is as reliable a procedure as complex reconstructions and other salvage surgeries.3–16 The advantages of proximal row carpectomy include preservation of a functional arc of motion, satisfactory strength, pain relief, and high patient satisfaction.
Wrist motion has been shown to be equal or slightly less than preoperative motion. Grip strength has been reported to range between 64 and 100% of the contralateral normal wrist.4,7,11,12,17–21 In addition, patients may be converted to a wrist arthrodesis or arthroplasty if painful osteoarthritis develops. The disadvantages of proximal row carpectomy include loss of carpal height, an incongruous joint, and possible progression of radiocapitate arthrosis. Imbriglia et al. have shown that the radius of curvature of the capitate is approximately two-thirds of the lunate fossa of the distal radius. Using cineradiography, they demonstrated that the motion of the capitate on the distal radius is translational with a moving center of rotation.21 Imbriglia reported that 12 of 27 patients in his long-term follow-up study developed radiographic evidence of cartilage space narrowing, although without clinical consequence.13
Literature regarding arthroscopic proximal row carpectomy is sparse. There are no long-term studies, although short-term results are promising. The majority of the literature mentions arthroscopy as an available technique for proximal row carpectomy without discussing clinical results.5,22–25
Indications and Contraindications
Proximal row carpectomy26 has also been described in the treatment of failed carpal implants, cerebral palsy, spasticity, acute and chronic fractures and dislocations, and replantation. We do not currently recommend arthroscopic proximal row carpectomy in this latter subset of patients.
Other relative contraindications to proximal row carpectomy in general include degenerative changes of the capitate head or lunate fossa of the distal radius, multicystic carpal disease, and preexisting ulnar translocation of the carpus. Due to the high failure rate of open proximal row carpectomy in patients with inflammatory arthropathy (e.g., rheumatoid arthritis), both Culp et al. and Ferlic et al. do not recommend its use in these patients.4,27
Technique
The patient is positioned supine on the operating table, with the affected arm positioned on a radiolucent hand table. A well-padded arm tourniquet is placed proximal to the arm. The procedure can be carried out under general or regional anesthesia because operative times are generally less than two hours. The wrist is then suspended in a traction tower and 10 to 15 pounds of traction is applied (Figure 26.1). After distraction is obtained, landmarks are outlined on the dorsum of the wrist and the portals are made. The tourniquet is routinely inflated without additional exsanguination. Routinely, the 3-4 portal is the initial viewing portal.
Next, the midcarpal joint must be well visualized to ensure an adequate proximal capitate cartilaginous surface (Figure 26.2). If the status of the capitate joint is questionable, an alternative procedure is performed: four-corner fusion, capitolunate arthrodesis, proximal row carpectomy with interposition arthroplasty, or wrist arthrodesis. Assessment of the midcarpal articular surfaces is accomplished through the radial midcarpal portal, which is approximately 1 cm distal to the 3-4 portal. Arthroscopic instruments that will be needed to perform the proximal row carpectomy include a hook probe, a 2.9 shaver or radiofrequency device, a 4.0 bur, small sharp osteotomes, pituitary rongeurs, and an image intensifier.
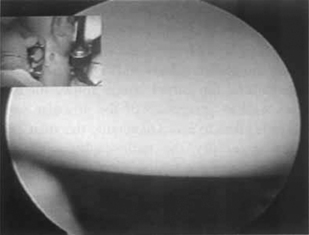
FIGURE 26.2 View from radial midcarpal portal demonstrating a healthy-appearing proximal capitate.
(Reproduced with permission from Culp RW, Osterman AL, Talsania JS. Arthroscopic proximal row carpectomy. Tech Hand and Upp Ext 1997;2(1):116–19).
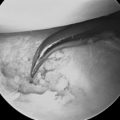
The first step in performing the proximal row carpectomy, after one is satisfied with the cartilage status of the proximal pole of the capitate and the lunate fossa, is to remove the scapholunate and lunatotriquetral ligaments with a shaver or radiofrequency device. This is performed through the 4-5 and/or 6-R portal. Next, the core of the lunate is removed with a bur. Care is taken to avoid damaging the lunate fossa and proximal capitate by leaving an “eggshell” rim of lunate, which is morcellized with a pituitary rongeur under direct vision and/or with image intensification (Figure 26.3).
Next, using the 3-4 or 4-5 portal as a working portal the scaphoid and triquetrum are fragmented with an osteotome and bur under image intensification (Figures 26.4 and 26.5) and removed piecemeal with a pituitary rongeur. Coring out and fragmenting the carpal bones allows for easy removal as well as protection of the articular cartilage. Great care is taken to avoid damaging the articular cartilage and to avoid damaging the volar extrinsic ligaments, especially the radioscaphocapitate—which will be responsible for maintaining the stability of the capitate in the lunate fossa.
FIGURE 26.4 Fluoroscopic guidance is utilized to aid fragmentation of the scaphoid and triquetrum.
(Reproduced with permission from Culp RW, Osterman AL, Talsania JS. Arthroscopic proximal row carpectomy. Tech Hand and Upp Ext 1997;2(1): 116–19).
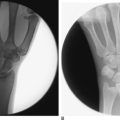
After the entire proximal row is removed, the wrist is examined under radiographic image intensification (Figures 26.6 and 26.7). Care is taken to ensure that there is not impingement of the trapezium against the radial styloid. Some authors advocate a modest styloidectomy. Although we rarely perform this procedure, if necessary it can be done arthroscopically with the aid of image intensification.

FIGURE 26.6 Preoperative radiograph demonstrating chronic scapholunate dissociation.
(Reproduced with permission from Culp RW, Osterman AL, Talsania JS. Arthroscopic proximal row carpectomy. Tech Hand and Upp Ext 1997;2(1):116–19).
Complications
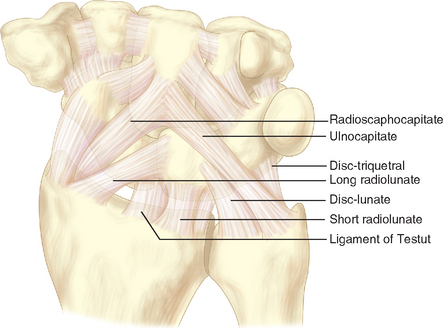
Care must be taken to avoid disrupting the volar extrinsic carpal ligaments, particularly the radioscaphocapitate ligament, during excision of the proximal carpal row (Figure 26.8). To avoid ligamentous injury, a thin shell of cortical bone may be left attached to the volar radiocarpal ligaments. In addition, there is also the potential to irritate nerves (particularly the dorsal ulnar sensory branch), and the possibility of damage to the median and ulnar nerves (particularly the ulnar nerve) while using the osteotomes.
1 Stamm TT. Excision of the proximal row of carpus. Proc Roy Soc Med. 1944;38:74-75.
2 Lee RW, Hassan DM. Proximal row carpectomy. In: Watson HK, Weinzweig J, editors. The Wrist. Philadelphia: Lippincot Williams & Wilkins; 2001:545-554.
3 Culp RW. Proximal row carpectomy. Operat Tech Orthop. 1996;2:69-71.
4 Culp RW, McGuigan FX, Turner MA, Lichtman DM, Osterman AL, McCarroll HR. Proximal row carpectomy: A multicenter study. J Hand Surg. 1993;18A:19-25.
5 Roth JH, Poehling GG. Arthroscopic “-ectomy” surgery of the wrist. Arthroscopy J Arthroscop Relat Surg. 1990;6(2):141-147.
6 Siegel JM, Ruby LK. A critical look at intercarpal arthrodesis: Review of the literature. J Hand Surg. 1996;21A:717-723.
7 Tomaino MM, Delsignore J, Burton RI. Long-term results following proximal row carpectomy. J Hand Surg. 1994;19A:694-703.
8 Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advance collapse wrist: Proximal row carpectomy versus four-corner arthrodesis. J Hand Surg. 1995;20A:965-970.
9 Cohen MS, Kozin SH. Degenerative arthritis of the wrist: Proximal row carpectomy versus four corner arthrodesis. J Hand Surg. 2001;26A:94-104.
10 Culp RW, Williams CS. Proximal row carpectomy for the treatment of scaphoid nonunion. Hand Clin. 2001;17(4):663-669.
11 Jebson PJL, Hayes EP, Engber WD. Proximal row carpectomy: A minimum 10-year follow-up study. J Hand Surg. 2003;28A:561-569.
12 DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: A study with a minimum of ten years of follow-up. J Bone Joint Surg [Am]. 2004;86:2359-2365.
13 Imbriglia JE. Proximal row carpectomy. Technique and long-term results. Atlas Hand Clin. 2000;5:101-109.
14 van Kooten EO, Coster E, Segers MJM, Ritt MJPF. Early proximal row carpectomy after severe carpal trauma. Injury. 2005;36:1226-1232.
15 Thomas AA, Rodriguez E, Segalman K. Keinbock’s disease in an elderly patient treated with proximal row carpectomy. J Hand Surg. 2004;29A:685-688.
16 Diao E, Andrews A, Beall M. Proximal row carpectomy. Hand Clin. 2005;21(4):553-559.
17 Begley BW, Engber WD. Proximal row carpectomy in advanced Kienbock’s disease. J Hand Surg. 1994;19A:1016-1018.
18 Nevaiser RJ. On resection of the proximal carpal row. Clin Orthop. 1986;202:12-15.
19 Nevaiser RJ. Proximal row carpectomy for posttraumatic disorders of the carpus. J Hand Surg. 1983;8A:301-305.
20 Clendenin MB, Green DP. Arthrodesis of the wrist: Complications and their management. J Hand Surg. 1981;6A:253-257.
21 Imbriglia JE, Broudy AS, Hagberg WC, McKernan D. Proximal row carpectomy: Clinical evaluation. J Hand Surg. 1990;15A:462-530.
22 Culp RW, Osterman AL, Talsania JS. Arthroscopic proximal row carpectomy. Tech Hand and Up Extrem Soc. 1997;2(1):116-119.
23 Gupta R, Bozentka DJ, Osterman AL. Wrist arthroscopy: Principles and clinical applications. J Am Acad Orthop Surg. 2001;9(3):200-209.
24 Nagle DJ. Laser-assisted wrist arthroscopy. Hand Clin. 1999;15(3):495-499. ix.
25 Atik TL, Baratz ME. The role of arthroscopy in wrist arthritis. Hand Clin. 1999;15(3):489-494.
26 Calandruccio JH. Proximal row carpectomy. J Am Soc Surg Hand. 2001;2(1):112-122.
27 Ferlic DC, Clayton ML, Mills MF. Proximal row carpectomy: Review of rheumatoid and non-rheumatoid wrists. J Hand Surg. 1991;16A:420-424.