CHAPTER 30 Arthroscopic Proximal Row Carpectomy
Proximal row carpectomy (PRC) is a reliable alternative to arthrodesis in the treatment of wrist osteoarthritis. PRC is a motion-preserving salvage procedure that involves excision of the scaphoid, lunate, and triquetrum and converts the complex link joint of the wrist into a simple hinge.1 The procedure has faced considerable criticism in regard to alteration of the normal anatomy of the wrist joint, impairment of strength and motion, improper redistribution of joint loading, subsequent radiocapitate arthritis, and an unpredictable outcome.2 Conversely, many investigators have documented satisfactory motion preservation, maintained grip strength, pain relief, and patient satisfaction. Several medium- and long-term follow-up studies have demonstrated that PRC is a reliable procedure with outcomes comparable to those of other reconstructive and salvage procedures of the wrist.3–17
ANATOMY
The proximal row of carpal bones operates as an intercalated segment between the distal radius and the distal carpal row. Proximal row intercarpal ligament disruption leads to wrist instability. Injuries to the scapholunate interosseous ligament and the extrinsic ligamentous complex allow the lunate to extend, creating dorsal intercalated segment instability.18 The resultant palmar flexion of the scaphoid alters load distribution across the radioscaphoid articulation, increasing contact pressures and eventually leading to degenerative changes.19 The sequential progression of arthritis that ensues is referred to as scapholunate advanced collapse (SLAC) wrist.20
Another form of scaphoid pathology associated with wrist arthritis is that which results from nonunion or malunion after a scaphoid fracture. This arthritic condition also follows a predictable pattern of progression, known as scaphoid nonunion advanced collapse (SNAC).21 In stage I, incongruity of the distal radioscaphoid articulation leads to degenerative changes that compromise the scaphoid’s ability to stabilize the carpal rows. Stage II involves arthrosis of the scaphocapitate articulation. As wrist stability deteriorates in stage III, the capitate migrates proximally, and arthrosis between the capitate head and scapholunate complex results. The radiolunate and proximal scaphoid pole articulations are typically spared even in advanced disease.
PATIENT EVALUATION
History and Physical Examination
Middle-aged men, notably laborers, make up much of this patient population. Patients present with a history of a prior injury most likely incurred by a fall onto an outstretched hand or a previous wrist surgery. Although the SLAC wrist is not always symptomatic, the patient typically complains of decreased grip and pinch strength and of activity-related pain, particularly wrist extension and radial deviation.
Physical examination may be facilitated by employing Watson’s standard approach to the examination of radial-sided wrist pain.22 The first maneuver assesses the articular–nonarticular (ANA) junction as the wrist is ulnarly deviated and the junction between the articular and nonarticular cartilage is palpated. Second, the scaphotrapeziotrapezoid (STT) joint is palpated by following the second metacarpal proximally until a space is reached, denoting the STT joint. Third, the dorsal wrist syndrome is ruled out by palpating between the second and fourth dorsal compartments of the wrist. A fourth test is the Watson scaphoid shift, which is performed by attempting to push the scaphoid dorsally from its volar side while passively radially deviating the wrist. A positive test elicits wrist pain as a result of scapholunate injury or ligamentous laxity. The fifth examination maneuver is the finger extension test, in which the wrist is flexed and the fingers are extended against resistance; increased loading of the radiocarpal joint and extensor tendon pressure produce pain.
TREATMENT
Indications and Contraindications
The indications for the standard open PRC are also those that are applied to the arthroscopic technique. They include degenerative conditions of the proximal carpal row, such as SLAC, SNAC, chronic perilunate dislocation, Preiser’s disease, and Kienböck’s disease. One indication for PRC is complex fracture dislocation of the wrist.14 The rationale cited by the authors of this 2005 case series14 was to avoid the disadvantages of arthrodesis while anticipating the likely post-traumatic arthrosis in this patient population. Failed carpal implants, cerebral palsy and spasticity, and reimplantation have also been described as indications for PRC, although we do not recommend the latter groups of patients for an arthroscopic technique.23
The relative contraindications to PRC are multicystic carpal disease, preexisting ulnar translocation of the carpus, and degenerative changes of the lunate fossa or capitate head. A 2007 study investigated a method to salvage a PRC for patients with degenerative changes of the head of the capitate. Tang and Imbriglia performed osteochondral resurfacing of the capitate in eight patients undergoing PRC who had a grade II to IV (modified Outerbridge scale) area of capitate chondrosis less than 10 mm in diameter.24 The results with osteochondral resurfacing compared favorably with published results of conventional PRC in terms of pain relief, employment status, range of motion, and grip strength. Culp and associates4 and Ferlic and colleagues25 did not recommend PRC for patients with inflammatory arthropathy because of its high failure rate.
Therapeutic Options
The biomechanical literature has focused on compensatory radiocarpal loading and kinematics after PRC. Blankenhorn and coworkers performed a cadaveric study using computed tomography to assess wrist motion before and after PRC.26 Their results showed that wrist range of motion after PRC was sufficient for activities of daily living. Flexion and extension motion at the radiocarpal joint after PRC was greater than motion at the radiocarpal and midcarpal joints of the intact wrist, whereas overall wrist motion decreased. After PRC, the normal rotational motion of the capitate head (in the intact wrist midcarpal joint) was altered to a combination of rotation and translation.
More contemporary reports have included Disabilities of the Arm, Shoulder, and Hand (DASH) scores as a measurement of upper extremity disability after PRC. Whereas several Scandinavian studies17,27–30 with variable follow-up times published DASH scores ranging from 28 to 36, DiDonna and associates reported an average DASH score of 9 in their study of 22 wrists after a minimum follow-up of 10 years.12
Cohen and Kozin published their results for a prospective cohort of similar patient groups with wrist osteoarthritis treated with scaphoid excision and four-corner fusion or PRC.9 Follow-up examination revealed no significant difference in the flexion-extension arc, ulnar deviation, or grip strength between the groups. The investigators also reported pain relief and patient satisfaction to be similar.
Based on combined outcomes from the larger series in the literature, PRC results in approximately 60% of the average flexion-extension arc and 71% of the grip strength of the contralateral wrist.4,7–9,31–36 The degree of patient satisfaction is high, ranging from 80% to 100%,7–9,11,13,31–40 and failure rates tend to be low, ranging from 0% to 20%.4,31,32,34,38 One criticism of PRC is that it causes radiocapitate arthrosis. DiDonna and colleagues observed degeneration of the radiocapitate articulation in 14 of 17 wrists during an average follow-up time of 14 years. Despite the degree of radiographic degenerative changes, there was no significant association between the arthrosis and wrist pain, range of motion, work restrictions, or patient satisfaction.12
Arthroscopy has become an increasingly valuable tool in the treatment of wrist pathology. The breadth of treatment options in the wrist surgeon’s armamentarium continues to grow, as do advances in the arthroscopic equipment available. The pathologic conditions of the wrist that the arthroscopist is capable of treating include triangular fibrocartilage complex tears, distal radius and carpal fractures, cartilage injuries, and bone resections. There is scant literature available discussing arthroscopic PRC. Although there are no long-term follow-up studies, the short-term studies have described promising results.5,41–44
Arthroscopic Technique
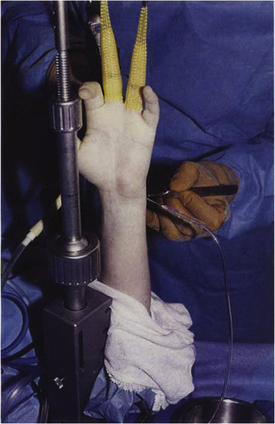
The patient is placed in the supine position, with the affected upper extremity on a radiolucent hand table. Operative time is usually less than 2 hours, and regional or general anesthesia is adequate for this procedure. A well-padded tourniquet is wrapped around the upper arm, and the wrist is suspended in a traction tower with 10 to 15 pounds applied (Fig. 30-1). The tourniquet is inflated, but additional exsanguination is unnecessary. After distraction is introduced, the dorsal aspect of the wrist is palpated for landmarks, and the portals are made. The 3-4 portal is routinely used as the primary viewing portal.
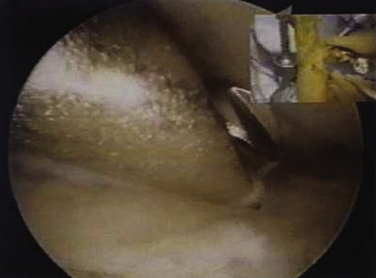
To assess the integrity of the proximal capitate surface, the midcarpal joint is visualized (Fig. 30-2). If the quality of this cartilaginous surface is questionable, we proceed to an alternative procedure (i.e., four-corner fusion, capitolunate arthrodesis, PRC with interpositional arthroplasty, or wrist arthrodesis). Visualization of the midcarpal joint is performed by establishing a radial midcarpal portal. This location is determined by measuring approximately 1 cm distal to the 3-4 portal.
FIGURE 30-2 A healthy-appearing proximal capitate is seen through the midcarpal portal.
(From Culp RW, Osterman AL, Talsania JS. Arthroscopic proximal row carpectomy. Tech Hand Up Extrem Soc. 1997;2:116-119.)
After the surgeon is satisfied with the status of the cartilaginous surfaces of the proximal capitate and lunate fossa, the first step in performing the PRC is to remove the scapholunate and lunatotriquetral ligaments with a shaver or radiofrequency probe. This step is carried out through the 4-5 portal or the 6-R portal, or both. This is followed by removal of the core of the lunate with a burr (Fig. 30-3). Care is taken not to damage the proximal capitate or lunate fossa, which is accomplished by leaving behind an eggshell rim of the lunate. This remainder of the lunate is then morcellized with a pituitary rongeur under direct vision or image intensification.
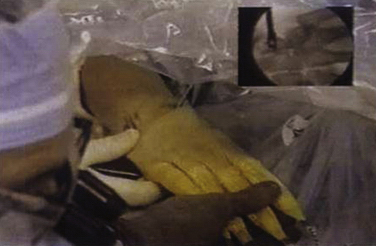
The next step is fragmentation of the scaphoid and triquetrum with an osteotome and burr under image intensification and removal of the fragments in a piecemeal fashion with a pituitary rongeur while working through the 3-4 or 4-5 portal (Figs. 30-4 and 30-5). The surgeon can ensure easy removal and greater protection of the articular cartilage by first coring out and fragmenting these carpal bones.

FIGURE 30-4 An osteotome used with x-ray guidance to remove part of the scaphoid and triquetrum.
(From Culp RW, Osterman AL, Talsania JS. Arthroscopic proximal row carpectomy. Tech Hand Up Extrem Soc. 1997;2: 116-119.)
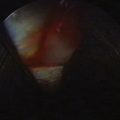
After the entirety of the proximal carpal row has been removed, the wrist is examined under image intensification (Fig. 30-6). Special attention is paid to the radial styloid area to be sure there is no impingement against the trapezium. Some surgeons recommend a moderate styloidectomy. Although we rarely carry out this aspect of the procedure, it can be done quite easily with the aid of the image intensifier.
PEARLS& PITFALLS
Postoperative Rehabilitation
Initially, patients are placed in a short arm volar plaster splint. Between 7 and 10 days postoperatively, the portal sutures are removed, and immobilization is continued with a short arm thermoplastic splint for an additional 3 weeks. At 4 weeks, the splint is removed and gentle range-of-motion exercises are begun. Strengthening is started approximately 8 weeks after surgery.
COMPLICATIONS
Iatrogenic articular cartilage damage must be avoided, especially at the lunate fossa and proximal capitate. The surgeon must not violate the extrinsic ligaments, particularly the radioscaphocapitate ligament, while excising the proximal carpal row (see Figs. 30-4 and 30-5). This is accomplished by coring out these carpals in such a way that a thin shell of cortical bone is left attached to the volar radiocarpal ligaments.
CONCLUSIONS
Arthroscopic PRC requires less dissection and therefore leads to potentially less morbidity. However, this technique requires excellent arthroscopic skills. The overall patient satisfaction level has been high, and postoperative pain levels have been low. Patients are pleased with the smaller scars associated with arthroscopy. In our experience, patients who undergo arthroscopic PRC have had functional range of motion, satisfactory grip strength, and acceptable pain relief.
1. Stamm TT. Excision of the proximal row of the carpus. Proc R Soc Med. 1944;38:74-75.
2. Lee RW, Hassan DM. Proximal row carpectomy. In: Watson HK, Weinzweig J, editors. The Wrist. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:545-554.
3. Culp RW. Proximal row carpectomy. Operat Tech Orthop. 1996;2:69-71.
4. Culp RW, McGuigan FX, Turner MA, et al. Proximal row carpectomy: a multicenter study. J Hand Surg Am. 1993;18:19-25.
5. Roth JH, Poehling GG. Arthroscopic “-ectomy” surgery of the wrist. Arthroscopy J Arthroscop Relat Surg. 1990;6:141-147.
6. Siegel JM, Ruby LK. A critical look at intercarpal arthrodesis: review of the literature. J Hand Surg Am. 1996;21:717-723.
7. Tomaino MM, Delsignore J, Burton RI. Long-term results following proximal row carpectomy. J Hand Surg Am. 1994;19:694-703.
8. Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: proximal row carpectomy versus four-corner arthrodesis. J Hand Surg Am. 1995;20:965-970.
9. Cohen MS, Kozin SH. Degenerative arthritis of the wrist: proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg Am. 2001;26:94-104.
10. Culp RW, Williams CS. Proximal row carpectomy for the treatment of scaphoid nonunion. Hand Clin. 2001;17:663-669.
11. Jebson PJ, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study. J Hand Surg Am. 2003;28:561-569.
12. DiDonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: a study with a minimum of ten years of follow-up. J Bone Joint Surg Am. 2004;86:2359-2365.
13. Imbriglia JE. Proximal row carpectomy: technique and long-term results. Atlas Hand Clin. 2000;5:101-109.
14. Van Kooten EO, Coster E, Segers MJM, Ritt MJPF. Early proximal row carpectomy after severe carpal trauma. Injury. 2005;36:1226-1232.
15. Thomas AA, Rodriguez E, Segalman K. Kienböck’s disease in an elderly patient treated with proximal row carpectomy. J Hand Surg Am. 2004;29:685-688.
16. Diao E, Andrews A, Beall M. Proximal row carpectomy. Hand Clin. 2005;2:553-559.
17. De Smet L, Robijns F, Degreef I. Outcome of proximal row carpectomy. Scand J Plast Reconstr Surg Hand Surg. 2006;40:302-306.
18. Linscheid RL, Dobyns JH, Beabout JW, Bryan RS. Traumatic instability of the wrist: diagnosis, classification, and pathomechanics. J Bone Joint Surg Am. 1972;54:1612-1632.
19. Burgess RC. The effect of rotatory subluxation of the scaphoid on radioscaphoid contact. J Hand Surg Am. 1987;12(pt 1):771-774.
20. Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9:358-365.
21. Vender MI, Watson HK, Wiener BD, Black DM. Degenerative change in symptomatic scaphoid nonunion. J Hand Surg Am. 1987;12:514-519.
22. Watson HK, Weinzweig J. Physical examination of the wrist. Hand Clin. 1997;13:17-34.
23. Calandruccio JH. Proximal row carpectomy. J Am Soc Surg Hand. 2001;2:112-122.
24. Tang P, Imbriglia J. Osteochondral resurfacing (OCRPRC) for capitate chondrosis in proximal row carpectomy. J Hand Surg Am. 2007;32:1134-1142.
25. Ferlic DC, Clayton ML, Mills MF. Proximal row carpectomy: review of rheumatoid and non-rheumatoid wrists. J Hand Surg Am. 1991;16:420-424.
26. Blankenhorn BD, Pfaeffle HJ, Tang P, et al. Carpal kinematics after proximal row carpectomy. J Hand Surg Am. 2007;32:37-46.
27. Nagelvoort R, Kon M, Schuurman A. Proximal row carpectomy: a worthwhile salvage procedure. Scand J Plast Reconstr Surg Hand Surg. 2002;36:289-299.
28. Lukas B, Herter F, Englert A, Backer K. Advanced carpal collapse: proximal row carpectomy or midcarpal arthrodesis?. Handchir Mikrochir Plast Chir. 2003;35:304-309.
29. Streich N, Martini A, Daeke W. Proximal row carpectomy in carpal collapse. Handchir Mikrochir Plast Chir. 2003;35:299-303.
30. Trankle M, Sauerbier M, Blum K, et al. Proximal row carpectomy: a motion preserving procedure in the treatment of advanced carpal collapse. Unfallchirurg. 2003;106:1010-1015.
31. Jorgensen EC. Proximal row carpectomy: an end-result study of twenty-two cases. J Bone Joint Surg Am. 1969;51:1104-1111.
32. Neviaser RJ. Proximal row carpectomy for posttraumatic disorders of the carpus. J Hand Surg Am. 1983;8:301-305.
33. Green DP. Proximal row carpectomy. Hand Clin. 1987;3:163-168.
34. Imbriglia JE, Broudy AS, Hagberg WC, McKernan D. Proximal row carpectomy: clinical evaluation. J Hand Surg Am. 1990;15:426-430.
35. Tomaino MM, Miller RJ, Cole I, Burton RI. Scapholunate advanced collapse wrist: proximal row carpectomy or limited wrist arthrodesis with scaphoid excision. J Hand Surg Am. 1994;19:134-142.
36. Krakauer JD, Bishop AT, Cooney WP. Surgical treatment of scapholunate advanced collapse. J Hand Surg Am. 1994;19:751-759.
37. Crabbe WA. Excision of the proximal row of the carpus. J Bone Joint Surg Br. 1964;46:708-711.
38. Inglis AE, Jones EC. Proximal-row carpectomy for diseases of the proximal row. J Bone Joint Surg Am. 1977;59:460-463.
39. Neviaser RJ. On resection of the proximal carpal row. Clin Orthop. 1986;202:12-15.
40. Begley BW, Engber WD. Proximal row carpectomy in advanced Kienböck’s disease. J Hand Surg Am. 1994;19:1016-1018.
41. Culp RW, Osterman AL, Talsania JS. Arthroscopic proximal row carpectomy. Tech Hand Up Extrem Soc. 1997;2:116-119.
42. Gupta R, Bozentka DJ, Osterman AL. Wrist arthroscopy: principles and clinical applications. J Am Acad Orthop Surg. 2001;9:200-209.
43. Nagle DJ. Laser-assisted wrist arthroscopy. Hand Clin. 1999;15:495-499.
44. Atik TL, Baratz ME. The role of arthroscopy in wrist arthritis. Hand Clin. 1999;15:489-494.