CHAPTER 12 Arthroscopic Plication of Lunotriquetral Ligament Tears
Introduction
Arthroscopy of the wrist has been promoted as an important adjunct to the diagnosis of subtle ligamentous instability because of the ability to directly view the interosseous ligaments, secondary articular cartilage changes, and intra-articular pathology.1 With the development of advanced techniques and improved instrumentation, wrist arthroscopy is also becoming an important tool in the treatment of complex injuries (including carpal instability).
History and Physical Exam
The initial evaluation of the wrist begins with the patient’s history, specifically reviewing mechanism of injury, hand dominance, athletic participation, work history, and recent activities. Areas of swelling, tenderness, and crepitation should be identified. Ballottement or shuck testing is often helpful in diagnosing intercarpal instability.2 To perform this maneuver, stabilize the lunate or triquetrum and feel for increased motion of the LT joint during palmar and dorsal stressing. Important physical findings are tenderness over the LT joint and/or the TFCC, increased translation of the lunate with respect to the triquetrum, and crepitation with pain during pronation, supination, or ulnar deviation.
Radiographic evaluation of a painful wrist should include a zero rotation posteroanterior,3,4 true lateral, and oblique views of the wrist. Ulnar variance, lunotriquetral interval, greater and lesser arc continuity, and the radiolunate and scapholunate angles are assessed. In cases where the physical examination findings are equivocal, an arthrogram or MRI can be obtained.
Ulnar Ligamentous Anatomy
Our approach to LT injuries had evolved from the anatomical concepts of the ulnar ligaments in relationship to the lunotriquetral joint and the TFCC. The lunotriquetral interosseous ligament is thicker both volarly and dorsally5 with a membranous central portion. Normal lunotriquetral kinematics is imparted from the integrity of the LTIOL,6 ulnolunate, ulnotriquetral,6–8 dorsal radiotriquetral (RT), and scaphotriquetral (ST) ligaments.6,7,9 Severe instability such as a volar intercalated segmental instability (VISI) requires damage to both the dorsal RT and ST ligaments.6,7,9
The TFCC is the primary stabilizer of the distal radioulnar joint via the dorsal and volar radioulnar ligaments.10,11 This helps to stabilize the ulnar carpus, and transmits axial forces to the ulna.12,13 The TFCC originates from the ulnar aspect of the lunate fossa of the radius and inserts on the base of the ulnar styloid and distally on the lunate, triquetrum, hamate, and fifth metacarpal base. The integrity of the triangular fibrocartilage, volar radiocarpal, and dorsal radiocarpal ligaments is visible at arthroscopy. TFCC compromise is often a part of more extensive ulnar-sided injuries.14 The volar and dorsal aspects of the lunotriquetral ligament merge with the ulnocarpal extrinsic ligaments volarly and the dorsal radiolunotriquetral ligament dorsally, anchoring the triquetrum.15
The ulnocarpal volar ligaments are composed of the ulnolunate (also known as the disc-lunate), the ulnotriquetral (UT)—also known as the disc-triquetral ligaments—and the ulno-capitate. The ulnolunate and ulnotriquetral ligaments originate on the volar triangular fibrocartilage complex (TFCC) and insert on the volar lunate and volar triquetrum (respectively) as well as the LT ligament.14,16,17 Just palmar lies the ulno-capitate ligament, providing a direct attachment from the ulna to the palmar ulnar ligamentous complex.
Ligament plication has been implemented to manage capitolunate instability.18 The central portion of the volar radiocapitate ligament was tethered to the radiotriquetral ligament by a volar approach. UT-UL ligament plication, developed by one of the authors (FHS), mimics this technique. It has been used in treating those injuries that do not severely destabilize the LT joint, such as those producing a VISI deformity that requires functional compromise of the dorsal extrinsic ligaments (dorsal radiotriquetral and scaphotriquetral). Arthroscopic volar ulnar ligament plication both reduces surgical trauma and allows concurrent assessment of its effect while viewing through the radiocarpal and midcarpal joints.
Arthroscopic Operative Technique
Congruency
Laxity
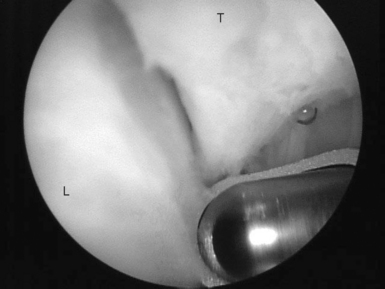
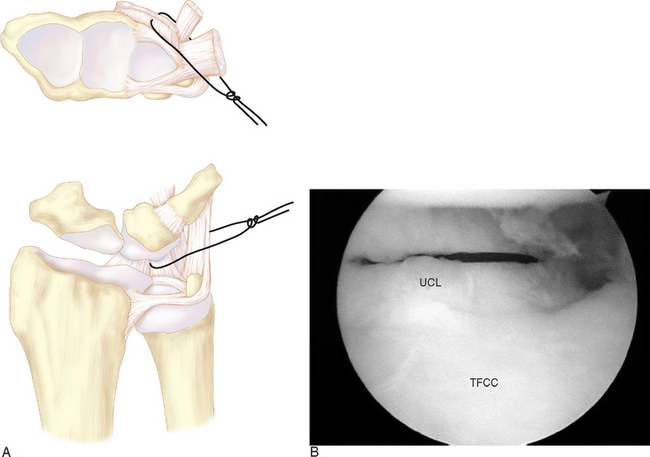
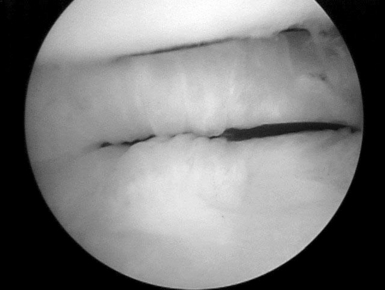
The interval between the disc-lunate and disc-triquetral ligament identifies the lunotriquetral joint and interosseous ligament. The LTIOL is gently debrided (Figure 12.1). Through the v6-U portal, an 18-gauge spinal needle is passed just volar to the disc-triquetral, ulno-capitate, and disc-lunate—entering the radiocarpal joint at the radial edge of the UL ligament just distal to the articular surface of the radius. A #2–0 PDS suture is placed through the needle into the joint. The suture is retrieved either sequentially through the 6-R and then through the v6-U or directly through the v6-U—using a wire loop suture retriever. It is then tagged as the first plicating suture (Figure 12.2).
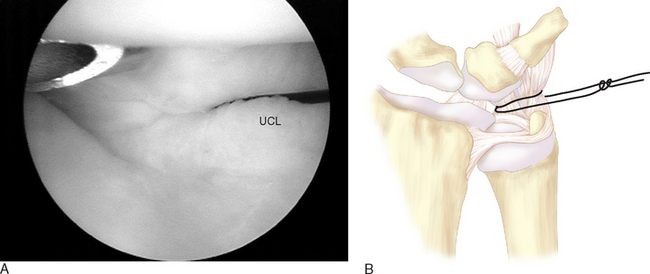
In likewise fashion, a second plicating suture is placed approximately 5 mm distal to the first so that the suture loops are parallel to the lunate and triquetrum and tagged as the second plicating suture (Figure 12.3). Tension on the first stitch often facilitates a second needle passage through the ulnolunate and ulnotriquetral ligaments. The adequacy of the plication should be assessed by applying tension to the stitch and observing its effect on the LT interval after each suture passage.
Finally, through the v6-U portal a spinal needle and then a suture are passed through the volar aspect of the capsule at the pre-styloid recess and then through the peripheral rim of the TFCC. The wire retriever is introduced through the ulnar capsule and the suture is brought out the v6-U portal to tighten the ulnar capsule. The three sets of sutures are tied at the termination of the procedure after the lunotriquetral joint has been congruently reduced and stabilized with K-wires.
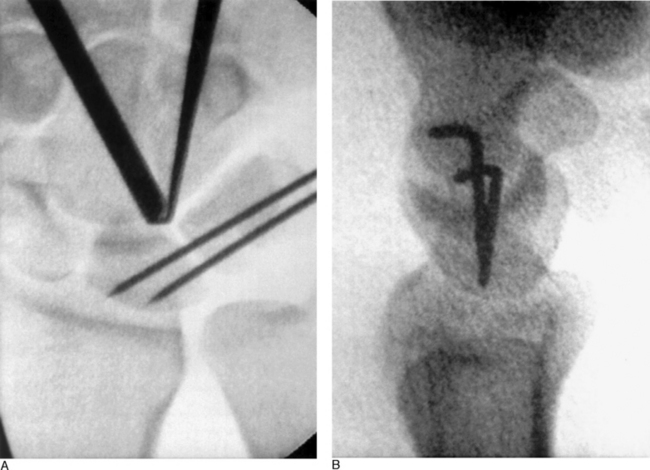
While viewing through the midcarpal radial portal, a midcarpal-ulnar (MCU) portal is created. A probe is used to assess lunotriquetral joint incongruity and mobility, and to reduce the lunotriquetral joint (Figure 12.4). A spinal needle can be placed in the midpalmar space from ulnar to radial across the distal aspect of the LT joint and used as a guide for percutaneous pin placement into the triquetrum. The triquetrum is reduced congruent with the lunate articular cartilage by applying traction to the plication sutures and firm pressure on the triquetrum.
The initial K-wire should be inserted 2 to 3 millimeters proximal to the spinal needle. Two 0.045 smooth K-wires are placed percutaneously across the lunotriquetral joint (Figure 12.5). The first pin is advanced across the lunotriquetral interval from ulnar to radial under fluoroscopic guidance, and the second pin is placed using the first pin as a guide to placement. After satisfactory reduction of the lunotriquetral joint, traction is released, the forearm is held in neutral rotation, and the plication stitches are tied at the 6-U portal (with the knots placed below the skin; Figure 12.6). The K-wires are either cut subcutaneously or bent outside the skin.
Patients with lunotriquetral ligament tears often have a positive ulnar variance.2,20,21 In an extension of the initial treatment group, patients with ulnar abutment syndrome (with associated lunate chondromalacia, TFCC tears, and LTIOL tears) have been treated by LT plication stabilization in conjunction with an arthroscopic wafer procedure.
Postoperative Care
After surgery the patient is initially placed in a long arm splint, with the elbow flexed at 90 degrees, the forearm in neutral rotation, and the wrist in neutral flexion and extension. At approximately one week after surgery, a Muenster cast is applied—with the forearm and wrist in neutral rotation and flexion, respectively. At approximately six weeks after surgery, the K-wires are removed. A removable Muenster cast is used for an additional two weeks to allow daily gentle wrist flexion, extension, pronation, and supination within a painless arc of motion. Eight weeks after surgery, strengthening exercises are instituted and work hardening can begin slowly over 8 to 24 weeks postoperatively.
Results
In a case series, we looked at a group of 21 patients, including 7 who were treated as workman’s compensation claimants and 4 patients were competitive athletes who sustained their injury during sport. All patients complained of ulnar-sided wrist pain, which was invariably increased by use of the wrist. The mean time between the onset of symptoms and treatment was 2.5 years (range 1 week to 5.5 years). Seventeen patients recalled a specific injury (hyperextension 12, twisting 2, unknown 3), and four noted a gradual onset of symptoms. Three patients had additional significant injuries to the affected extremity: elbow dislocation, humeral shaft fracture, and anterior shoulder dislocation.
Summary
Symptomatic lunotriquetral interosseous ligament tears have been managed by simple arthroscopic debridement, ligamentous repair, and intercarpal arthrodesis. Ligamentous repair or reconstruction with a tendon graft requires an extensile approach. Lunotriquetral joint fusion limits flexion and extension and radioulnar deviation by 14 and 25%, respectively.22 Arthroscopic ulnocarpal ligament plication in addition to LT joint reduction and stabilization is designed to augment the volar aspect of the LT joint. LT ligament tears are often associated with other pathology, notably ulnar-carpal ligament tears and disruption of the distal radioulnar joint.23 Suture plication of the ulnocarpal ligaments shortens their length, which acts as a check-rein to excessive lunotriquetral motion (perhaps similar to ulnar shortening procedures). Suture plication of the peripheral rim of the TFCC is thought to increase tension in the ulnar DRUJ capsule.
1 Kulick M, Chen C, Swearingen P. Determining the diagnostic accuracy of wrist arthroscopy. Annual meeting of the American Society for Surgery of the Hand, Toronto, 1990.
2 Reagan D, Linscheid R, Dobyns J. Lunatotriquetral sprains. J Hand Surg. 1984;9A:502-514.
3 Palmer A, Glisson R, Werner F. Ulnar variance determination. J Hand Surg. 1982;7:376.
4 Gilula L. Posteroanterior wrist radiography: Importance of arm positioning. J Hand Surg. 1987;12A:504-508.
5 Bednar J, Osterman A. Carpal instability: Evaluation and treatment. J Am Acad Orthop Surg. 1993;1:10-17.
6 Horii E, Garcias-Elias M, An KN, et al. A kinematic study of luno-triquetral dissociations. J Hand Surg. 1991;16A:355-362.
7 Viegas S, Peterson P, et al. Ulnar-sided perilunate instability: An anatomic and biomechanical study. J Hand Surg. 1990;15A:268.
8 Trumble T, Bour C, Smith R, et al. Kinematics of the ulnar carpus to the volar intercalated segment instability pattern. J Hand Surg. 1990;15A:384.
9 Reagan DS, Linscheid RL, Dobyns JH. Lunotriquetral sprains. J Hand Surg. 1984;9A:502-514.
10 Cooney W, Dobyns J, Linscheid R. Arthroscopy of the wrist: Anatomy and classification of carpal instability. Arthroscopy. 1990;6:113-140.
11 Mayfield J. Patterns of injury to carpal ligaments: A spectrum. Clin Orthop. 1984;187:36.
12 Palmer A, Werner F. Triangular fibrocartilage complex of the wrist: Anatomy and function. J Hand Surg. 1981;6:153.
13 Werner F, Palmer A, Fortino M, et al. Force transmission through the distal ulna: Effect of ulnar variance, lunate fossa angulation, and radial and palmar tilt of the distal radius. J Hand Surg. 1992;17A:423.
14 Melone CJr., Nathan R. Traumatic disruption of the triangular fibrocartilage complex, pathoanatomy. Clin Orthop. 1992;275:65-73.
15 Green D. Carpal dislocation and instabilities. In: Green D, editor. Operative Hand Surgery. New York: Churchill Livingston; 1988:878-879.
16 Palmer A, Werner F. Biomechanics of the distal radioulnar joint. Clin Orthop. 1984;187:26.
17 Garcias-Elias M, Domenech-Mateu J. The articular disc of the wrist: Limits and relations. Acta Anat. 1987;128:51.
18 Johnson R, Carrera G. Chronic capitolunate instability. J Bone Joint Surg. 1986;68A:1164-1176.
19 Viegas S, Wagner K, Patterson R, et al. Medial (hamate) facet of the lunate. J Hand Surg. 1990;15A:564-571.
20 Pin P, Young V, Gilula L, et al. Management of chronic lunatotriquetral ligament tears. J Hand Surg. 1989;14A:77-83.
21 Osterman A, Sidman G. The role of arthroscopy in the treatment of lunatotriquetral ligament injuries. Hand Clin. 1995;11:41-50.
22 Seradge H, Sterbank P, Seradge E, et al. Segmental motion of the proximal carpal row: Their global effect on the wrist motion. J Hand Surg. 1990;15A:236-239.
23 Ambrose L, Posner M. Lunate-triquetral and midcarpal joint instability. Hand Clin. 1992;8:653-668.