CHAPTER 10 Arthroscopic Medial Plication for Patellar Instability
An acute dislocation of the patella may be described as a primary disruption of the patellofemoral relationship, where the patella is displaced out of the femoral sulcus. The direction of dislocation is most commonly lateral, although superior,1 medial,2 intra-articular,1 and vertical intercondylar3 have also been described. This chapter will deal only with the most common lateral patellar dislocation.
The incidence of acute dislocation of the patella is difficult to assess accurately, and has only been addressed in a few studies. McManus and colleagues4 have reviewed the records of 94,875 pediatric visits to their emergency room over a 4-year period and found some evidence of patellar dislocation in 55 (0.05%), although only 33 (0.03%) could be proven to be acute dislocations. Cash and Hughston5 reported treating 399 patients with this disorder over a 30-year period (13.3 patients/year). Castelyn and Handelberg6 have reported an incidence of acute patellar dislocation of 2.44% in their series of knee injuries. More recently, Nietosvaara and associates7 have reported an incidence of acute patellar dislocation in 43/100,000 adolescents/year (0.04%).
Most reports in the literature agree that acute patellar dislocation occurs in a young population, with an average age of approximately 20 years most commonly reported.4,5 However, within this group, the incidence of redislocation appears to be significantly higher in patients who sustain their first dislocation at an earlier age.4,8 Although earlier studies suggested that females appeared to be at a higher risk for both acute and recurrent dislocation.8–10 more recent data suggest that the gender incidence may be equal.11
The natural history of acute dislocation has been addressed in a number of studies. Hawkins and coworkers12 treated 20 patients conservatively (3 weeks of immobilization). At 40 months of average follow-up, 3 had redislocated (15 %), 4 had apprehension or complaints of instability (20%), and 15 had pain associated with patellofemoral (PF) crepitus. Remarkably, 100% were able to return to work and recreational sports. Cofield and Bryan9 studied 48 patients with acute dislocations treated conservatively (closed reductions and immobilization for 1 to 6 weeks). Of these, 44% redislocated and 27% went on to require subsequent surgery. If subjective criteria are include, 52% were considered failures.
McManus and colleagues4 reviewed 28 patients with acute dislocations; 21 were treated without surgery. Five patients redislocated and 11 were considered symptomatic. Cash and Hughston5 have reported a redislocation rate of 20% to 43% among first-time dislocators treated with immobilization alone, with the rate depending on the presence of congenital predisposition (patellofemoral dysplasia). In a more recent study of 74 acute patellar dislocations, Atkin and assoociates11 reported that 58% of patients were still symptomatic during strenuous activities at an early follow-up of 6 months.
ANATOMY
The patella is the largest sesamoid bone in the human body13 and, like other sesamoid bones, most likely evolved as a mechanism to protect the adjacent tendon (quadriceps in this case) from abrasion and to improve distribution of forces across the tendon.14 In addition, the patella acts to improve the biomechanical leverage of the quadriceps during extension, acting as a fulcrum,15 with its greatest effect seen at 20 degrees of flexion.16
Most animal species load the knee in a flexed position and have a well-stabilized patella maintained within the confines of the trochlea throughout the range of motion. Humans, on the other hand often load the knee near full extension, with the patella out of the confines of the trochlea and susceptible to instability. Interestingly, in great apes, the femoral diaphysis is straight and the trochlea is flat, with no elevation of the lateral trochlea ridge; however, the patella remains stable because the flexed angle of their knee. In humans, the distal femur evolved into an obliquity angle of 8 to 10 degrees, necessitating the development of a deeper trochlea sulcus, with an elevated lateral trochlear lip, to stabilize the patella.17
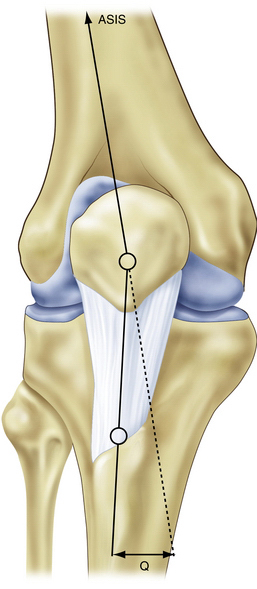
The Q angle is defined as the angle between the quadriceps mechanism and the patellar tendon, and is a helpful measure of patellar tracking. The greater the anatomic valgus, or the greater the external rotation present in the tibia, the larger the Q angle will be, resulting in a laterally directed force vector (Fig. 10-1). A normal Q angle is typically considered to be less than 15 degrees. Increased femoral anteversion will also result in a high Q angle by causing internal rotation of the femur relative to the tibia.
Causative Factors
Disruption or distortion of any of these anatomic factors can result in patellofemoral instability.
Medial Patellofemoral Ligament Insufficiency
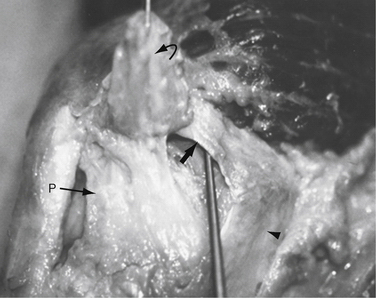
Numerous studies have shown that the medial patellofemoral ligament (MPFL) is the most important stabilizer of the patella to lateral translation. Hautamaa and associates18 have shown in a cadaver biomechanical study that with serial sectioning the MPFL contributes 50% of the patellofemoral stability (Fig. 10-2).19 In a similar study, Desio and coworkers19 have shown that the MPFL contributes 60% of the stability, with the medial patellomeniscal ligament contributing an additional 13%. Clinical studies on patients with patellar dislocation also seem to confirm this finding, with both surgical and MRI evidence of disruption of the MPFL after patella dislocation.20–22
Trochlear Dysplasia
Trochlear dysplasia is thought to be a contributor to patellar instability, but is often difficult to measure accurately radiographically. Magnetic resonance imaging (MRI) is the most accurate method of measurement, with an MRI study showing a 100% sensitivity and a 96% specificity when a criteria of less than a 3-mm trochlear depth was used, measured 3 cm above the femorotibial articulation.23 However, trochlear dysplasia is rare and, even when present, does not usually require direct treatment. In addition, patients with unilateral instability have trochlear dysplasia bilaterally, but only instability on the side where they have disrupted their MPFL. For rare cases of patella instability thought to be caused by severe trochlear dysplasia, several procedures have been described to deepen the trochlea (trochleoplasty), including osteotomy and elevation of the lateral trochlea with bone grafting24 or undermining and deepening of the trochlea groove.25 It is my experience that even in the presence of trochlear dysplasia, trochleoplasty is usually not necessary. The vast majority of cases of patellar instability can be managed with proximal soft tissue realignment, and occasionally with the addition of a tibial tubercle osteotomy.
Weak Vastus Medialis Obliquus.
The VMO is a distinct muscle grouping of the vastus medialis that has a distinct nerve supply26 and whose fibers insert into the superomedial aspect of the patella at approximately 65 degrees to the longitudinal axis.27 There can be anatomic variation on the insertion site to the patella. A more medial insertion results in a more medial stabilizing effect. A more superior insertion changes the force vector, providing less medial stabilizing force, and may be a contributor to lateral instability. Weakness of the VMO removes a significant dynamic stabilizing influence on the patella. Strengthening of this muscle is an important component of any rehabilitation program. The VMO contracts maximally in the terminal range of extension, and can be best strengthened with terminal, short-arc extension exercises.
PATIENT EVALUATION
History
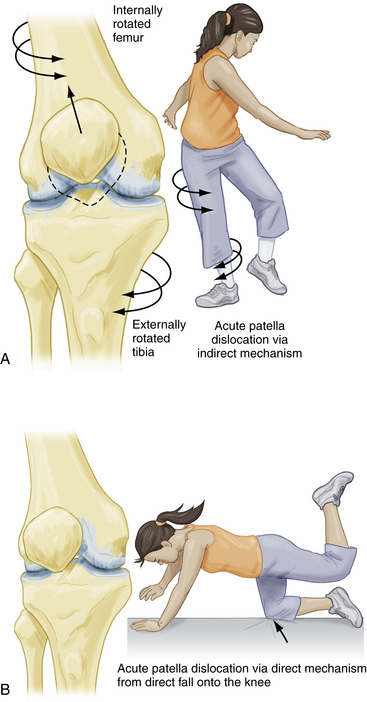
Understanding the mechanism of injury may be helpful in determining the diagnosis. Two mechanisms for acute lateral patellar dislocation have been proposed, direct and indirect. The indirect mechanism of injury results from a powerful quadriceps contracture against an internally rotated femur (externally rotated tibia) and usually involves a sudden twisting motion on a firmly planted foot, such as a sudden change of direction while playing soccer with cleats. The direct mechanism of dislocation involves a direct blow to the medial aspect of the patella, resulting from a fall or contact with another player during athletic activity. A combination of these two mechanisms may contribute to a single injury (Fig. 10-3).
Physical Examination
The first step in evaluating a patient for instability is to inspect the knee with the patient standing. Valgus alignment, foot pronation, and the presence of squinting patellae should be noted. The Q angle is an essential parameter for evaluating instability. It is measured from the anterosuperior iliac spine (ASIS) to the center of the patella, and from the center of the patella to the tibial tubercle. This angle should be evaluated in full extension as well as at 30 degrees of knee flexion and seated at 90 degrees. There is controversy regarding which evaluation is most useful, and there has been significant intraobserver error reported.28 In my practice, the 0- and 30-degree Q angles are most helpful.
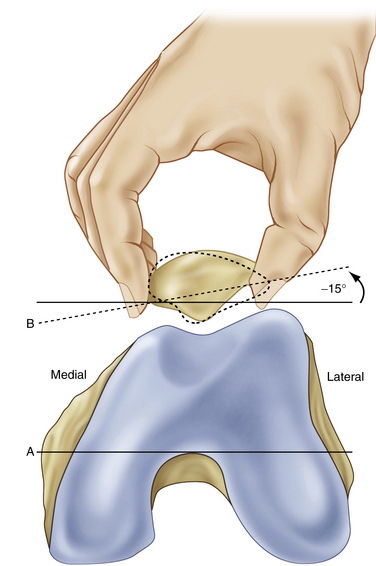
The lateral retinaculum is then assessed for tightness, with the patient supine and the leg fully extended. If the examiner cannot lift the lateral edge of the patella 15 degrees, or to a neutral plane parallel to the examination table, the patellar tilt test is positive and indicates a tight lateral retinaculum. The examiner should also attempt to translate the patella medially. Movement of less than 15 mm, or one quadrant of the patellar width, indicates a tight lateral retinaculum (Fig. 10-4).
The J sign is a dynamic test that demonstrates severe lateral translation of the patella with active terminal extension of the knee, and often is seen with more severe cases of instability, especially with a high-riding patella. The patient is asked to extend the knee actively against gravity. As the patella disengages from the trochlea, it jumps laterally, making an inverted J sign (Fig. 10-5).
Diagnostic Imaging
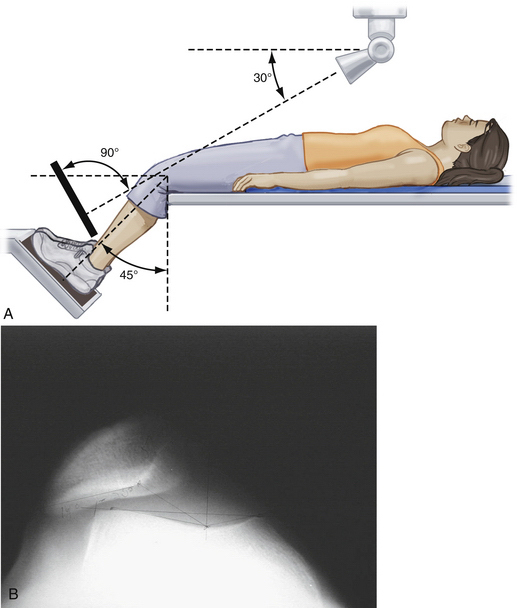
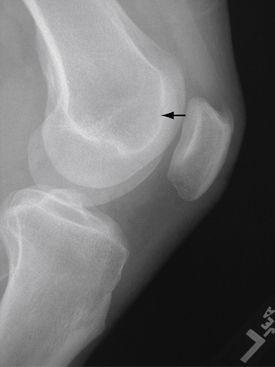
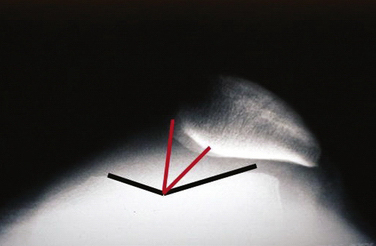
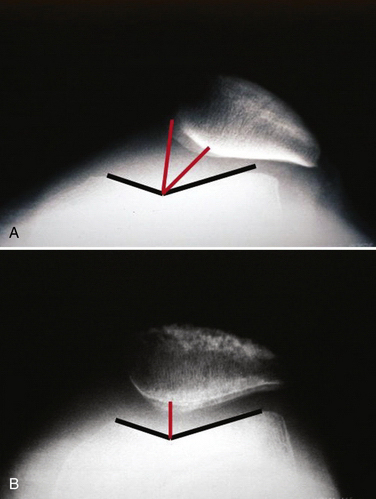
The standard evaluation of patients with PF symptoms will include an anteroposterior (AP), lateral and 45-degree tangential view of the patella (Merchant view; Fig. 10-6). The AP view is rarely helpful, but will reveal the presence of a bipartite patella or a patellar fracture. The lateral view is useful to identify loose bodies and patella alta or baja, and will reveal the presence of early degenerative changes with inferior or superior patella osteophytes. The lateral view will also reveal calcification or traction spurs associated with chronic patellar-quadriceps tendinitis, and will demonstrate irregularity of the tibial tubercle associated with Osgood-Schlatter disease. Trochlear depth and dysplasia may also be determined on the lateral view (Fig. 10-7),29 although there is poor reproducibility and interobserver reliability.30
The Merchant view is useful to evaluate patellar alignment. Various measurements can be performed on this x-ray that are useful in assessing patellar tracking, including the congruence angle, tilt angle, and lateral translation (Fig. 10-8).
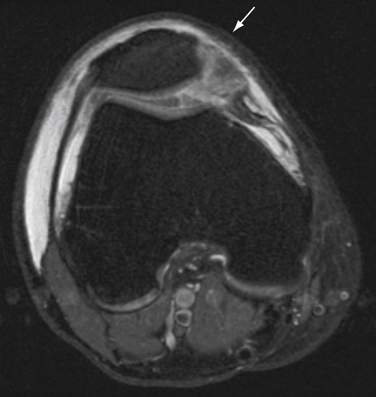
For acute dislocations that have spontaneously reduced, radiographs are often normal. However, the radiographs will be helpful if they reveal an osteochondral fracture fragment from the medial patellar facet or lateral trochlea. An avulsion fracture of the retinaculum off the medial border of the patella is even more diagnostic. Teitge31 has suggested the use of an axial oblique view to visualize this avulsion better. The incidence of chondral and osteochondral fracture is up to 46% in patients with acute patellar dislocation,32 although most of these are only visible by arthroscopic and MRI evaluation. Occasionally, the diagnosis of patellar dislocation can only be made by the demonstration of a torn medial retinaculum as seen by MRI (Fig. 10-9). In several studies, MRI was thought to be diagnostic in 81% to 87% of cases, whereas surgical evaluation was diagnostic in confirming a torn medial retinaculum in 94% to 100% of cases.20–22
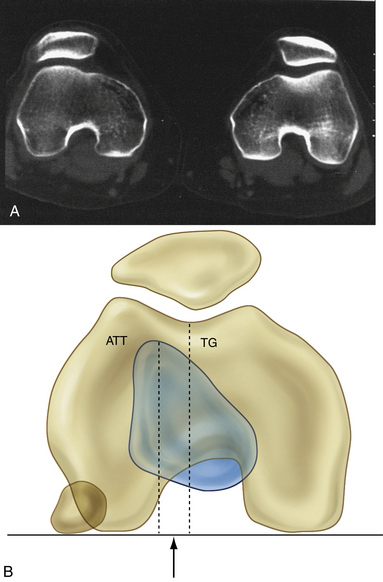
MRI may also be useful to find subtle changes of chondromalacia in the patella and trochlea associated with the instability, or to observe chondral fractures and loose bodies. Computed tomography (CT) scanning can be useful to evaluate the patellofemoral joint in lesser degrees of flexion, when the standard 45-degree Merchant view does not demonstrate anticipated malalignment,31,33 although I rarely order this study. Both MRI and CT scanning can be used to measure the TTTG distance; I prefer to use MRI, which provides similar information without radiation exposure, and also provides additional information about the status of the MPFL and cartilaginous structures (Fig. 10-10).
TREATMENT
Conservative Management
The traditional treatment for a primary acute patellar dislocation has been nonoperative, although the exact method of treatment is controversial. Most literature studies recommend some type of immobilization followed by an aggressive rehabilitation program.5,9,12 However the benefit of immobilization following patellar dislocation has not been proven, and results after immobilization and early range of motion appear to be the same.5,9 Furthermore, there does not seem to be a correlation between the length of immobilization and results.5,9,12
Long-term results suggest that the natural history of nonoperative treatment of patellar instability is not as favorable as commonly thought. In a group of 20 patients with acute dislocations treated conservatively, Hawkins and coworkers12 have reported a 20% incidence of ongoing instability and a 15% incidence of pain and crepitus. In their series of 48 patients with acute dislocations, Cofield and Bryan9 reported a 44% incidence of redislocation; 27% of these patients went on to subsequent surgery and, taking into account subjective criteria, 52% were considered failures. In 21 patients treated nonoperatively, McManus and colleagues4 have reported 5 redislocations and 11 patients who remained symptomatic. Cash and Hughston5 have reported a redislocation rate of 20% to 43%, depending on anatomic evidence of dysplasia predisposing to instability. In a more recent study, Fithian and associates34 have shown that of 189 patients followed over a period of 2 to 5 years after an acute patellar dislocation, 17% of first-time dislocators and 49% of patients with a previous history of dislocation had recurrences. The risk for recurrence was higher in women.
Surgical Management
With the advent of less invasive methods of treatment, and with more critical reviews of the results of nonoperative treatment, more authors are recommending surgical treatment, even for acute patellar dislocation.10,21,35,36 Relative indications for surgical treatment of a patellar dislocation include failure of conservative treatment, the presence of an osteochondral fracture (loose body), recurring instability, and significant residual subluxation on a postreduction Merchant view radiograph. Contraindications to the treatment of patients with patellas instability are rare, but would include patients with pain syndromes or reflex sympathetic dystrophy (RSD) that could be made worse with surgery. Care must also be taken with patients with unusual underlying pathology, such as Ehlers-Danlos syndrome, although I have successfully treated patients with such rare conditions as Charcot-Marie-Tooth disorder and nail patella syndrome.
Arthroscopic Technique
Role of Lateral Release.
Various surgical techniques have been proposed to correct patellar instability. Lateral release alone has been described, although results have been mixed, with a high incidence of recurring instability.37–39 Lateral release alone does not address the disrupted anatomy of the medial retinaculum and is not considered by most to be an effective treatment for true patellar instability or malalignment (subluxation).40 I do not recommend isolated lateral release for patellar instability.
Role of Medial Retinacular Repair and Reefing.
When surgery is indicated for patellar instability, most recommend treatment for the disrupted medial retinacular structures and medial PF ligament, often called proximal soft tissue realignment. Complex surgical reconstruction of the medial structures, such as the extensive open reconstruction as described by Insall and colleagues,41 have fallen out of favor, and minimally invasive open procedures for direct anatomic repair of the medial retinaculum and medial patellofemoral ligament have become the preferred method of repair.36 Several arthroscopically assisted procedures have also been reported,42–44 as well as an all- inside arthroscopic method,45 which is my preferred technique at this time.
Whether to add a lateral release at the time of medial repair is controversial. Several authors routinely perform a lateral release at the time of medial repair,36 whereas others have shown no advantage to adding a lateral release22 or individualize the decision based on tightness of the lateral retinaculum.32 My current recommendation is to base the decision on the tightness of the lateral retinaculum at the time of surgery, with a tendency toward recommending the lateral release if there is any doubt. An overly tight lateral retinaculum tethers the patella laterally, and will inhibit proper realignment despite medial reefing, especially in more chronic cases of recurring instability.
Arthroscopically Assisted Proximal Realignment
Initial recommendations for arthroscopic patellar realignment consisted primarily of arthroscopically assisted techniques using a medial incision. Yamamoto44 has treated 30 acute patellar dislocations with arthroscopic lateral release, along with an arthroscopically assisted repair of the medial retinaculum. The transcutaneous passage of sutures through the retinaculum using a large curved needle was recommended, although the sutures were still tied through a medial skin incision. Only acute dislocations were treated. Reported results were excellent, with only one case of redislocation.
Small43 reported a modified version of the Yamamoto technique, also using an arthroscopically assisted method and a small medial incision (Fig. 10-11). Patients with acute and recurrent dislocations were included, as well as those with malalignment and subluxation. Results were good to excellent in 92.5% of their 24 patients (27 knees), according to a subjective questionnaire. There were two recurrent subluxations, one reoperation for arthrofibrosis, and one superficial infection.
Henry and Pflum42 have described an arthroscopically assisted technique using cannulated needles, but tied the sutures through a medial incision as well. No follow-up series or results were reported.
All-Arthroscopic Proximal Realignment:
A number of authors have described entirely arthroscopic proximal realignment procedures, with good results.36,45–47 All these procedures have the advantage of eliminating any type of medial incision. The technique for arthroscopic realignment presented here is my preferred method of treatment for most patients with uncomplicated patellar instability.
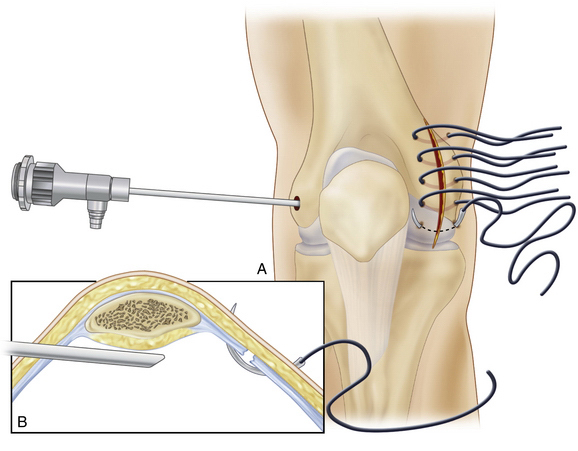
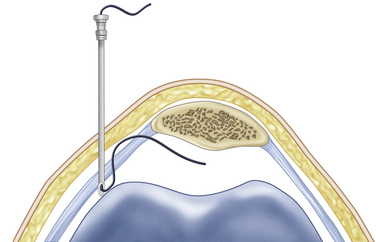
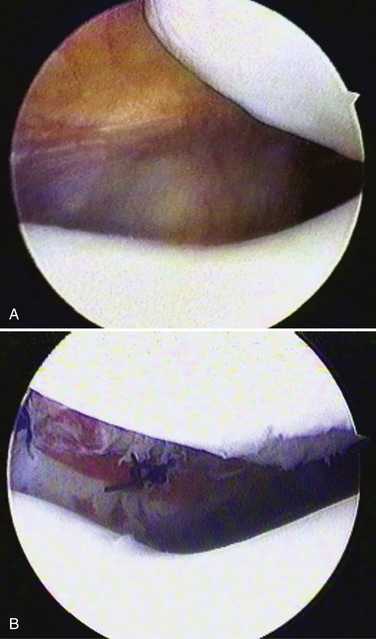
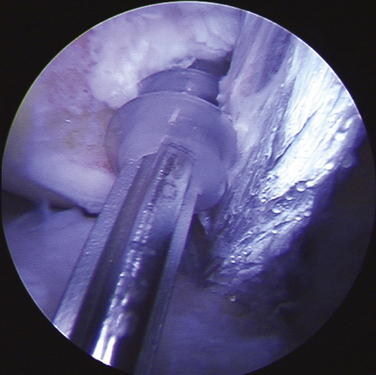
Surgery is performed under general anesthesia with a thigh holder in place. A tourniquet is applied, but rarely inflated. Before plication, a healing response is created along the medial retinaculum by gently abrading the tissue with a rasp or shaving with a whisker blade (Fig. 10-12). Medial retinacular sutures are introduced percutaneously using an epidural needle (Tuohy needle; Teleflex Medical (Rusch), Deluth, Ga). An epidural needle is essential because the noncutting edge on the inner bevel of the tip prevents cutting or damaging the suture. The needle is placed adjacent to the patella and a no. 1 PDS suture is passed manually through the needle and retrieved arthroscopically through an accessory superolateral portal (Fig. 10-13). Although nonabsorbable braided suture could be used, I prefer an absorbable suture in this highly sensitive area to avoid postoperative irritation from permanent knots.
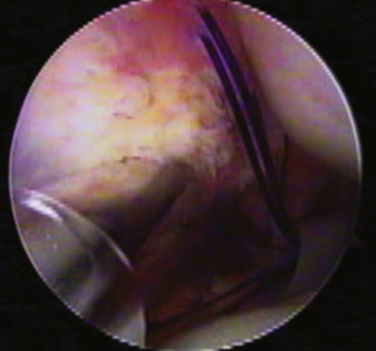
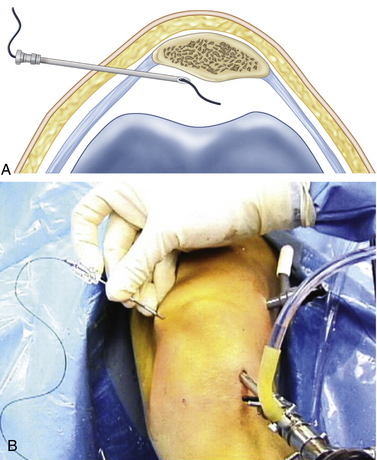
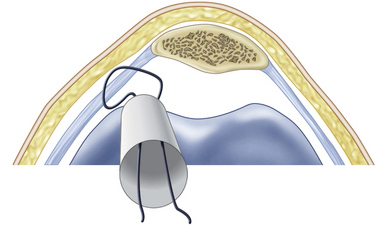
The needle is gently withdrawn from the retinaculum but not out of the skin. The needle is then redirected subcutaneously approximately 2 to 3 cm posteriorly and reinserted through the retinaculum (Fig. 10-14). This creates a loop of suture that is again retrieved through the same accessory portal. The needle is withdrawn completely and the process is repeated until four or five sutures are in place. The sutures are retrieved through an accessory proximal lateral portal and clamped for later imbrication of the medial retinaculum (Fig. 10-15). An arthroscopic lateral release is then performed with a standard electrocautery device. After the lateral release, the medial sutures are tied inside the joint from the proximal lateral or anteromedial portal using standard arthroscopic knot-tying techniques (Fig. 10-16).
Alignment and stability are checked and additional sutures added as necessary. I generally use four to six sutures. Occasionally, some dimpling of the skin will occur in the area of the sutures as the intra-articular knots are tied. The dimpling resolves with resorption of the sutures and postoperative rehabilitation, and has not been a problem. However, if desired, the dimpling can be addressed intraoperatively by spreading gently in the subcutaneous tissues with a small scissor through the medial portal to release the subcutaneous tissue.
PEARLS
PEARLS
Postoperative Management
Avoiding Complications
Although I prefer an all-arthroscopic method of proximal realignment, open and arthroscopically assisted proximal realignment procedures can also be effective in preventing recurring instability. However, these procedures are more frequently accompanied by complications, including the risk of joint stiffness, scar tissue, and overcorrection. Medial PF reconstruction using a graft is reserved for rare cases of failed arthroscopic realignment, or patients with inadequate native tissue. I reserve distal realignment for patients with instability associated with significant arthrosis, or those rare patients with a TTTG distance of more than 20 mm on overlapped CT or MR imaging. In these patients, biomechanical unloading and bony realignment of the patellofemoral joint are indicated, in conjunction with a soft tissue arthroscopic realignment.
OUTCOMES
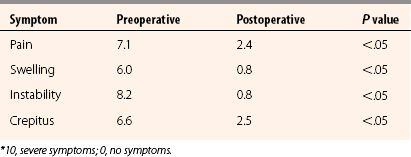
In a review of my 5-year results,45 93% of patients reported significant subjective improvement. The average Lysholm score improved from 41.5 to 79.3 (P < .05). Preoperative and postoperative radiographs were measured for congruence angle, lateral patellofemoral angle, and lateral patellar displacement, and all showed significant improvement postoperatively (P < .05; Fig. 10-17). There were no complications and no redislocations. Patients reported a significant improvement in pain, swelling, stair climbing, crepitus, and ability to return to sports (P < .05). Although the average Q angle in the study was 11 degrees, this procedure was successfully performed on patients with Q angles up to 20 degrees. None of the patients required a second operation for débridement of scar tissue or manipulation. All patients regained full range of motion as compared with the opposite side (Table 10-1).
CONCLUSIONS
I have now had over 10 years of follow-up on many patients, with continued good results. Arthroscopic realignment for patellar instability offers excellent results for stability and patient satisfaction, without the morbidity associated with more complex patellar realignment procedures. I continue to use this procedure as the main surgical treatment for most patients with lateral patellar instability.
1. Friden T. A case of superior dislocation of the patella. Acta Orthop Scand. 1987;58:429-430.
2. Larson RL, Jones OC. Dislocations and ligamentous injuries of the knee. In: Fractures in Adults. 2nd ed. Philadelphia: Lippincott; 1984.
3. Kaufman I, Habermann ET. Intercondylar vertical dislocation of the patella. A case report. Bull Hosp Joint Dis. 1973;34:222-225.
4. McManus MB, Rang M, Heslin J. Acute dislocation of the patella in children. Clin Orthop Relat Res. 1979;(139):88-91.
5. Cash JD, Hughston JC. Treatment of acute patella dislocation. Am J Sports Med. 1988;16:244-249.
6. Casteleyn PP, Handelberg F. Arthroscopy in the diagnosis of acute dislocation of the patella. Acta Orthop Belg. 1989;55:381-383.
7. Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop. 1994;14:513-515.
8. Larsen E, Lauridsen F. Conservative treatment of patella dislocations: influence of evident factors on the tendency to redislocate and the therapeutic result. Clin Orthop Relat Res. 1982;171:131-136.
9. Cofield RH, Bryan RS. Acute dislocation of the patella: results of conservative treatment. J Trauma. 1977;17:526-531.
10. Vainionpaa S, Laasonen E, Silvenoinen T, et al. Acute dislocation of the patella. A prospective review of operative treatment. J Bone Joint Surg Br. 1990;72:366-369.
11. Atkin DM, Fithian DC, Marangi KS, et al. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28:472-479.
12. Hawkins RJ, Bell RH, Anisette G. Acute patella dislocations: the natural history. Am J Sports Med. 1986;14:117-120.
13. Holingshead HW. Anatomy for Surgeons. 2nd ed. Vol 3. The Back and Limbs. Baltimore: Williams & Wilkins; 1990.
14. Dye SF. Patellofemoral anatomy. In: Fox JM, Del Pizzo W. The Patellofemoral Joint. New York: McGraw-Hill; 1993:1-11.
15. Fu FH, Seel MJ, Berger R. Patellofemoral biomechanics. In: Fox JM, Del Pizzo W. The Patellofemoral Joint. New York: McGraw-Hill; 1993:49-51.
16. Perry J, Antonelli D, Ford W. Analysis of knee joint forces during flexed knee stance. J Bone Joint Surg Am. 1975;57:961-967.
17. Tardieu C, Dupont JY. The origin of femoral trochlear dysplasia: comparative anatomy, evolution and growth of the patellofemoral joint. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:373-383.
18. Hautamaa PV, Fithian DC, Kaufmann KR, et al. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res. 1998;349:174-182.
19. Desio SM, Burks RT, Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26:59-65.
20. Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23:260-263.
21. Sanders TG, Morrison WB, Singleton BA, et al. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comput Assist Tomogr. 2001;25:957-962.
22. Sallay PI, Poggi J, Speer KP, et al. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24:52-60.
23. Pfirrmann CW, Zanetti M, Romero J, et al. Femoral trochlear dysplasia: MRI findings. Radiology. 2000;216:858-864.
24. Keene G, Marans HJ. Osteotomy for patellofemoral dysplasia. In: Fox JM, Del Pizzo W. The Patellofemoral Joint. New York: McGraw Hill; 1993:169-176.
25. Peterson L, Karlsson J, Brittberg M. Patellar instability with recurrent dislocation due to patellofemoral dysplasia. Results after surgical treatment. Bull Hosp Jt Dis Orthop Inst. 1988;48:130-139.
26. Weinstabl R, Scharf W, Firbas W, et al. The extensor apparatus of the knee joint and its peripheral vasti. Anatomic investigation and clinical relevance. Surg Radiol Anat. 1989;11:17-22.
27. Huberti HH, Hayes WC, Stone JL, et al. Force ratios in the quadriceps tendon and ligamentum pateallae. J Orthop Res. 1984;2:49-54.
28. Greene CC, Edwards TB, Wade MR, et al. Reliability of the quadriceps angle measurement. Am J Knee Surg. 2001;14:97-103.
29. Grelsamer RP, Tedder JL. The lateral trochlear sign. Femoral trochlear dysplasia as seen on a lateral view roentgenograph. Clin Orthop Relat Res. 1992;281:159-162.
30. Remy F, Chantelo C, Folntaine C, et al. Inter-and intraobserver reproducibility in radiographic diagnosis and classification of femoral trochlear dysplasia. Surg Radiol Anat. 1998;20:285-289.
31. Teitge RA. Radiology of the Patellofemoral Joint. Orthopedic Surgery Update Series. Princeton, NJ: Continuing Professional Education Center; 1985.
32. Harilainen A, Myllynen P. Operative treatment in acute patella dislocation: radiologic predisposing factors, diagnosis and results. Am J Knee Surg. 1988;1:178-185.
33. Schutzer SF, Rambsy GR, Fulkerson JP. Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am. 1986;17:235-248.
34. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114-1121.
35. Boring TH, O’Donoghue DH. Acute patella dislocation. Results of immediate surgical repair. Clin Orthop Relat Res. 1978;136:182-185.
36. Ahmad CS, Stein BE, Matuz D, et al. Immediate surgical repair of the medial patellar stabilizers for acute patellar dislocation. A review of eight cases. Am J Sports Med. 2000;28:804-810.
37. Aglietti P, Pisaneschi A, De Biase P. Lussazione recidivante di rotula: Tre tipi di trattamento chirurgico. G Ital Ortop Traumat. 1992;13:25-36.
38. Dandy DJ, Griffiths D. Lateral release for recurrent dislocation of the patella. J Bone Joint Surg Br. 1989;71:121-125.
39. Sherman OH, Fox JM, Sperling H, et al. Patellar instability: Treatment by arthroscopic electrosurgical lateral release. Arthroscopy. 1987;3:152-160.
40. Fulkerson JP, Cautilli RA. Chronic patella instability: subluxation and dislocation. In: Fox JM, Del Pizzo W, eds. The Patellofemoral Joint. New York: McGraw-Hill; 1993: 135-147.
41. Insall JN, Bullough PG, Burstein AH. Proximal tube realignment of the patella for chondromalacia patellae. Clin Orthop Relat Res. 1979;144:63-69.
42. Henry JE, Pflum FAJr. Arthroscopic proximal patella realignment and stabilization. Arthroscopy. 1995;11:424-425.
43. Small NC. Arthroscopically assisted proximal extensor mechanism realignment of the knee. Arthroscopy. 1993;9:63-67.
44. Yamamoto RK. Arthroscopic repair of the medial retinaculum and capsule in acute patellar dislocations. Arthroscopy. 1986;2:125-131.
45. Halbrecht JL. Arthroscopic patella realignment: An all-inside technique. Arthroscopy. 2001;17:940-945.
46. Haspl M, Cicak N, Klobucar H, et al. Fully arthroscopic stabilization of the patella. Arthroscopy. 2002;18:E2.
47. Fukushima K, Horaguchi T, Okano T, et al. Patellar dislocation: arthroscopic patellar stabilization with suture anchors. Arthroscopy. 2004;20:761-764.
48. Halbrecht JL. Patella problems in athletes. In: Johnson DJ, Pedowitz RA, editors. Practical Orthopaedic Sports Medicine and Arthroscopy. Philadelphia: Lippincott, Williams & Wilkins; 2006:677-707.