CHAPTER 3 Arthroscopic Management of Tibial Plateau Fractures
ANATOMY
As reviewed by Lubowitz and colleagues,1,2 the knee is anatomically designed well to achieve its function—providing stability, bending and rotational range of motion, and transmission of load. The tibia is the major weight-bearing bone of the knee joint. At its proximal articular surface, the tibia widens to form medial and lateral condyles. Between the condyles, the intercondylar eminence serves as the attachment for the menisci and the anterior and posterior cruciate ligaments. The relatively flattened condylar portions of the proximal tibia compromise the weight-bearing aspects of the plateau. The medial and lateral condyles articulate with corresponding medial and lateral femoral condyles.
PATIENT EVALUATION
History and Physical Examination
Classic patient history is trauma as a result of a fall or motor vehicle versus a pedestrian accident.1,2 Tibial plateau fractures are common in sports, particularly in skiers. Avulsion fractures commonly occur in children and adolescents, with 50% caused by a fall from a bicycle. However, it is sometimes misunderstood that this condition occurs only in the young. Although less common, ACL avulsion also occurs in adults.
Diagnostic Imaging
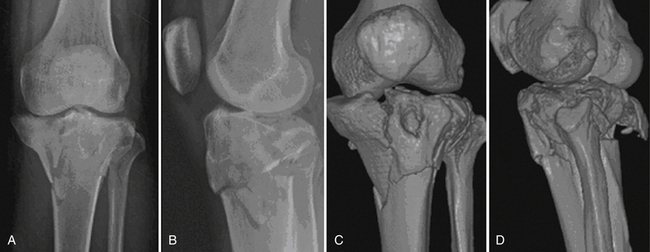
Standard radiologic knee trauma views usually reveal plateau fractures, but displaced fractures and compression fractures can be missed. X-rays are not accurate for determining the amount of depression when a compression fracture component is visible. Computed tomography (CT) with three-dimensional reconstruction provides precise information regarding the extent and pattern of articular and extra-articular components of the fracture. In addition to CT scanning to assess bony pathology, magnetic resonance imaging (MRI) is also recommended. MRI is the examination of choice for soft tissue injuries associated with tibial plateau fractures.
TREATMENT
Indications and Contraindications
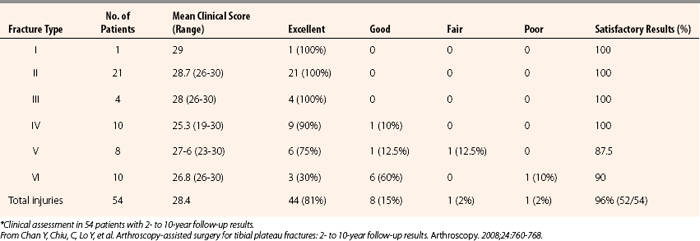
The key point is that surgery is generally indicated based on fracture classification. The Schatzker classification of tibial plateau fractures is illustrated in Figure 3-1. I recommend ARIF for all type III fractures, and ARIF should be considered for types I, II, and IV fractures. Arthroscopy-assisted surgery for Schatzker type V and VI fractures (skin incision and plating, with arthroscopy but no arthrotomy), can also be considered. Chen and associates3 have reported 85.1% and 90% satisfactory results for types V and VI fractures, respectively (Table 3-1).

FIGURE 3-1 Schatzker classification of tibial plateau fractures.
(Adapted from Lubowitz J, Elson W, Guttmann D. Part I: arthroscopic management of tibial plateau fractures. Arthroscopy. 2004;20:1063-1070.)
TABLE 3-1 Results of Arthroscopic Reduction and Internal Fixation of Schatzker Types V and VI Tibial Plateau Fractures*
The Meyers and McKeever classification of tibial intercondylar eminence fractures is illustrated in Figure 3-2. Surgery is indicated for type I fractures if they are associated with meniscus tears or other concomitant pathology that requires arthroscopy. Otherwise, these may be immobilized at or near full extension. Aspiration of hemarthrosis may result in substantial pain relief. There is sufficient evidence that surgery should be strongly considered for type II bird’s beak pattern fractures because of the high association of anterior horn of the medial (or occasionally the lateral) meniscus lodged within the fracture site.2,4–7 Closed reduction may be attempted for large type IIIB fractures because associated condylar contact may allow bony reduction after aspiration and hyperextension. For displaced type III fractures, ARIF is the state of the art procedure.2
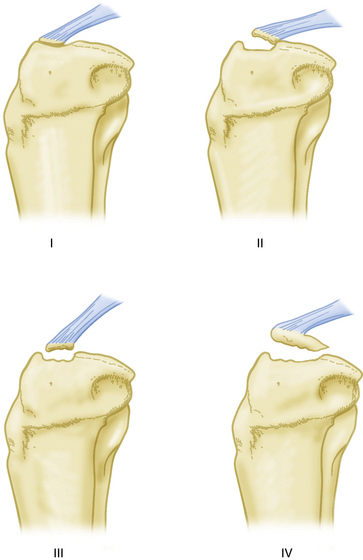
FIGURE 3-2 Meyers and McKeever classification of tibial plateau fractures.
(Adapted from Lubowitz, J, Elson, W, Guttmann, D. Part II: arthroscopic treatment of tibial plateau fractures: intercondylar eminence avulsion fracture. Arthroscopy. 2005;21:86-92).
An impressively large series by Chan and coworkers3 is summarized in Table 3-1. The key point is that fracture types I, II, III, and IV had 100% satisfactory results. Fracture type V had 87.5% satisfactory results and Schatzker type VI had 90% satisfactory results.
Hunter and Willis8 have described the outcome of suture or screw fixation of Myers and McKeever types II and III tibial intercondylar eminence fractures. At 32.6-month follow-up, the mean Tegner score was 6.35 and mean Lysholm score was 94.2. The best outcomes were seen in younger patients. No significant differences were seen in outcome with regard to type of fixation.
Conservative Management
As noted,1 not all fractures of the tibial plateau require surgery. Fractures that are stable and minimally displaced may be amenable to cast immobilization, or bracing may allow early motion (but with delayed weight bearing). Other indications for nonoperative treatment may include injuries to the peripheral (submeniscal) rim of the plateau, a unique fracture pattern, and fractures in older adult, low-demand, or osteoporotic patients. Meyers and McKeever type I tibial intercondylar eminence fractures may be immobilized near full extension. Aspiration may relieve pain in patient with intense hemarthrosis.
Arthroscopic Technique
My recommended ARIF technique was inspired by Caspari and colleagues,9 Jennings,10 and Buchko and Johnson.11 Operative treatment must be specifically determined for each fracture type.
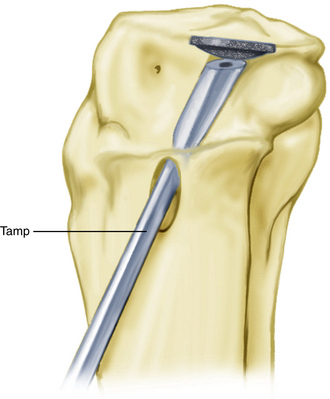
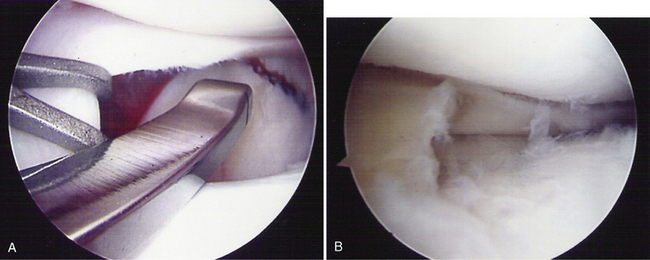
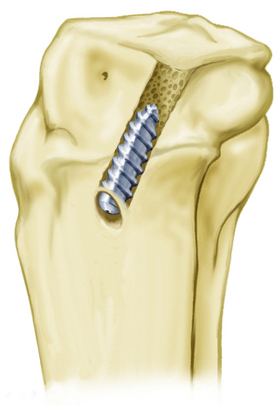
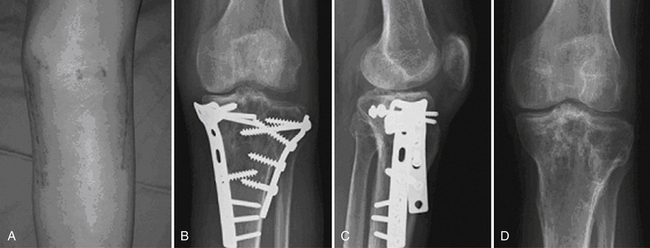
Note that split fractures should be reduced first. For type I fractures, percutaneous, cannulated lag screws may be placed over a guide wire. In types II, III, and IV patterns, compression is first elevated using an angled tamp placed over a guide wire (Fig. 3-3). An ACL guide with a modified spoon-shaped tip to mimic the curve of the femoral condyle is used to place the guide pin in the center of the compressed fragments through a small incision in the proximal anteromedial tibial metaphysis. A coring reamer circumferentially penetrates the tibia cortex while removing as little bone as possible. A cannulated tamp is used to elevate the fracture site under arthroscopic visualization (Fig. 3-4). The underlying metaphyseal bone and cortical disk serve as autograft. A calcium- or hydroxyapatite-impregnated bioabsorbable cannulated interference screw of large diameter is then advanced through the cortical window to elevate the fracture further under direct arthroscopic visualization (Fig. 3-5). The screw first provides elevation. Next, the screw provides rigid internal fixation of the compressed fracture.12 Moreover, for type III patterns, the screw obviates the need for percutaneous placement of subchondral, metal, cannulated buttress screws, which radically reduces morbidity. For type III fractures, using this new technique, fluoroscopy is not required. Locked buttress plating (ARIF with arthroscopy without arthrotomy) has been reported for types V and VI fractures (Figs. 3-6 to 3-8).
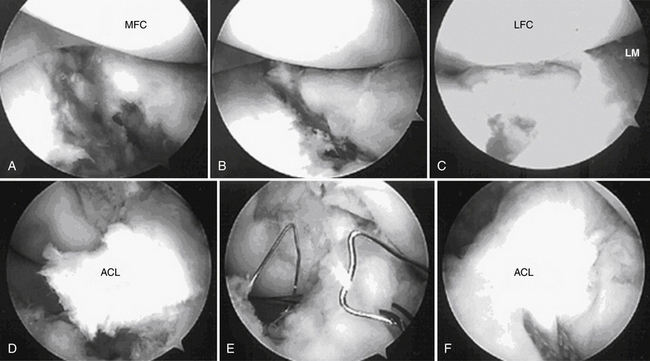
FIGURE 3-7 A, Preoperative arthroscopic view. A depressed medial tibial plateau is evident with a large bony gap. B, The depressed portion of the tibial articular cartilage is elevated by the technique of arthroscopy-assisted reduction with bilateral buttress plate fixation. C, The depressed portion of subchondral bone and the lateral tibial articular surface is elevated and reduced. D, Final management of ACL avulsion fracture with displacement. E, Arthroscopically assisted fixation by pullout suture. F, Four no. 5 Ethibond sutures (Ethicon, Somerville, NJ) were tied firmly at the proximal tibial site, and well reduction of ACL avulsion fracture could be visualized by arthroscopy. LFC, lateral femoral condyle; LM, lateral meniscus; MFC, medial femoral condyle.
(From Chan Y, Chiu, C, Lo Y, et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthroscopy. 2008;24:760-768.
Surgical Management: Tibial Intercondylar Eminence Avulsion Fractures
ARIF of ACL avulsions with screws was first described in 1993 by Lubowitz and Grauer,13,14 but I now acknowledge disadvantages, including risks of comminution of the fracture fragment, posterior neurovascular injury, and the need for hardware removal. Because of these risks, ARIF using nonabsorbable sutures passed through drill holes and tied over the tibial tubercle is now my preferred technique.
The patient is placed in a circumferential leg holder, with the knee off the end of the table. A tourniquet facilitates visualization, and the most recently published technique concludes that no fluoroscopy is needed for this procedure.12 Calf compartments must be continually palpated to ensure that fluid extravasation does not result in compartment syndrome. Although intercondylar eminence avulsion fractures are contained injuries, they may be associated with capsular disruption.2
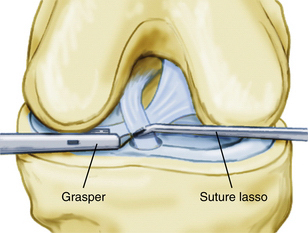
A 90-degree suture lasso may be placed percutaneously (or via an accessory portal) through the fibers of the ACL in its midcoronal plane and as close to the bony fragment (distally) as possible. The wire loop within the lasso is secured with an arthroscopic grasper (Fig. 3-9) and pulled via a cannula through either of the portals and loaded with a no. 2 high-strength suture. The high-strength suture is pulled back through the ligament fibers and out through the skin and accessory portal.
A Nitinol wire loop is passed up through the cannulated retro pins, medially and laterally, respectively. Routine suture passage brings the suture ends out through the medial and lateral drill holes. Distal traction reduces the fracture. The sutures are tied under tension while an assistant performs a reverse Lachman maneuver. With the use of supersutures, only one suture is usually required (Fig. 3-10).
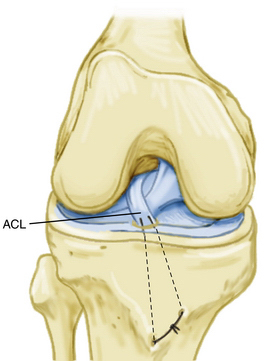
FIGURE 3-10 The fracture is reduced by pulling down on the suture ends, which are tied over the tibial tubercle.
(Adapted from Lubowitz, J, Elson, W, Guttmann, D. Part II: arthroscopic treatment of tibial plateau fractures: intercondylar eminence avulsion fracture. Arthroscopy. 2005;21:86-92).
Postoperative radiographs may suggest a few millimeters of superior displacement of the fracture fragment. This is usually not seen on the arthroscopic view, and as long as the surgeon is certain that the meniscus is not entrapped, this should not be considered a failure of surgical treatment. Despite this radiographic finding, which is often subtle, excellent functional outcome and knee stability are the rule.2
PEARLS& PITFALLS
POSTOPERATIVE MANAGEMENT
For ARIF of tibial plateau fractures, continuous passive motion is recommended. Early range of motion is encouraged, with the goal of 0 to 90 degrees at 2 weeks and full range of motion at 6 weeks. Weight bearing is not permitted for 3 months. Partial weight bearing is recommended during the fourth month, especially in the case of compressed fractures. Hinged bracing for 6 weeks is recommended for patients with associated collateral ligament injuries.1
For intercondylar eminence avulsion fractures, the patient can be discharged on the day of surgery. Crutches are optional and recommended at first, and patients are permitted to bear full weight with the knee locked in a brace in full extension. The brace is unlocked or removed for CPM. Formal physical therapy is recommended to achieve and monitor the goal of 90 degrees of knee flexion at 2 weeks and full range of motion by 6 weeks. Isometric quadriceps and hamstring and abductor and adductor strengthening with the knee locked in the brace are permitted during the first 6 weeks. After 6 weeks, the brace is discontinued. Resisted flexion is permitted through full range of motion, and resisted extension is permitted through a range of 30 to 90 degrees. Terminal resisted extension is not performed until 3 months.2
CONCLUSIONS
As noted,1,2 arthroscopy is a valuable tool for the assessment of tibial plateau fractures and is the treatment of choice for associated intra-articular pathology. ARIF of selected tibial plateau fractures allows anatomic reduction and rigid internal fixation with less morbidity than with ORIF, and has the advantage of superior visualization of the entire joint. I recommend ARIF for type III fractures and consideration of ARIF for types I, II and IV. Some authors have applied ARIF to more complex (type V or VI) fracture patterns, with satisfactory outcomes.3
1. Lubowitz, J, Elson, W, Guttmann, D. Part I: arthroscopic management of tibial plateau fractures. Arthroscopy. 2004;20:1063-1070.
2. Lubowitz, J, Elson, W, Guttmann, D. Part II: Arthroscopic treatment of tibial plateau fracturesintercondylar eminence avulsion fracture. Arthroscopy. 2005;21:86-92.
3. Chan Y, Chiu, C, Lo Y, et al. Arthroscopy-assisted surgery for tibial plateau fractures: 2- to 10-year follow-up results. Arthroscopy. 2008;24:760-768.
4. Burnstein DB, Viola A, Fulkerson JP. Entrapment of the medial meniscus in a fracture of the tibial eminence. Arthroscopy. 1998;4:47-50.
5. McLennan JG. The role of arthroscopic surgery in the treatment of fractures of the intercondylar eminence of the tibia. J Bone Joint Surg Br. 1982;64:477-480.
6. Falstie-Jensen S, Sondergard-Petersen PE. Incarceration of the meniscus in fractures of the intercondylar eminence of the tibia in children. Injury. 1984;15:236-238.
7. Zaricznyj B. Avulsion fracture of the tibial eminence treated by open reduction and pinning. J Bone Joint Surg Am. 1997;59:1111-1114.
8. Hunter RE, Willis JA. Arthroscopic fixation of avulsion fractures of the tibial eminence: technique and outcome. Arthroscopy. 2004;20:113-121.
9. Caspari RB, Hutton PM, Whipple TL, Meyers JF. The role of arthroscopy in the management of tibial plateau fractures. Arthroscopy. 1985;1:76-82.
10. Jennings JE. Arthroscopic management of tibial plateau fractures. Arthroscopy. 1985;1:160-168.
11. Buchko GM, Johnson DH. Arthroscopically assisted operative management of tibial plateau fractures. Clin Orthop Relat Res. 1996;(332):29-36.
12. Lubowitz J, Vance K, Ayala M, et al. Interference screw technique for arthroscopic reduction and internal fixation of compression fractures of the tibial plateau. Arthroscopy. 2006;22:1359e1-1359e3.
13. Lubowitz J, Grauer, J. Arthroscopic treatment of anterior cruciate ligament avulsion. Clin Orthop. 1993;294:242-246.
14. Lubowitz J, Grauer J. Arthroscopic Treatment of Anterior Cruciate Ligament Avulsion. Chicago: Mosby-Year Book; 1994.