CHAPTER 18 Arthroscopic Fusion for Degenerative Arthritis of the Subtalar Joint
Arthrodesis of the subtalar joint is an accepted treatment option for many problems of the hindfoot, such as post-traumatic and primary arthritis, posterior tibial tendon dysfunction, symptomatic congenital deformities, and inflammatory arthritis.1–3 Although sometimes viewed as a salvage procedure, results from subtalar fusions have been reported to be good or excellent in many patients.4–6
The many advantages of isolated subtalar arthrodesis compared with triple arthrodesis and other salvage procedures have been recognized. The major advantage of isolated fusion compared with triple arthrodesis or pantalar arthrodesis is that isolated subtalar fusion preserves motion in adjacent joints.7 In a study of 48 isolated subtalar arthrodeses, Mann found that preserving motion of the transverse tarsal joints decreased the incidence of clinically significant symptoms of arthritis.6
ANATOMY
The subtalar joint is composed of three articulations: the posterior, middle, and anterior joints or facets (Figs. 18-1 and 18-2). Several extra-articular ligaments stabilize the subtalar joint. The major ligaments encountered during subtalar arthroscopy are the intra-articular components, which consist of the interosseous, lateral, and anterior talocalcaneal ligaments. These components coalesce to form the division between the posterior and the middle facets of the subtalar joint. The interosseous ligament is a broad, stout structure that is approximately 2.5 cm wide from its medial to lateral side. It marks the arthroscopic boundary for posterior subtalar arthroscopy.
Open subtalar arthrodesis has historically been the fusion method of choice, and results have generally been favorable. Studies reporting the results of open fusion techniques have all described similar results for fusion rate, time to union, and complications, such as nonunion or malunion, infection, and symptomatic hardware problems.8–12 Open procedures entail removal of the interosseous ligaments and their vasculature and a lateral incision that can result in nerve dysfunction. Nonunion rates of 5% to 16% have been reported.4,6 The successful results of arthroscopic ankle fusion have stimulated the development of an arthroscopic approach for subtalar joint arthrodesis, which has the advantages of reduced perioperative morbidity and preservation of the blood supply.13–15
Arthroscopic subtalar arthrodesis was designed to improve traditional methods by using a minimally invasive technique. Subtalar arthroscopy has been described by several investigators, but few reports of arthroscopic subtalar fusion have been published.16 The development of an arthroscopic technique for subtalar arthrodesis was intended to lower morbidity using techniques and principles similar to those used for arthroscopic ankle fusion. It was hypothesized that perioperative morbidity could be reduced, blood supply preserved, and proprioceptive and neurosensory input enhanced. These theoretical advantages prompted us to initiate a prospective study to document the effectiveness of the procedure and to determine the time until complete fusion, the incidence of delayed unions and nonunions, and the incidence of complications.
PATIENT EVALUATION
Diagnostic Imaging
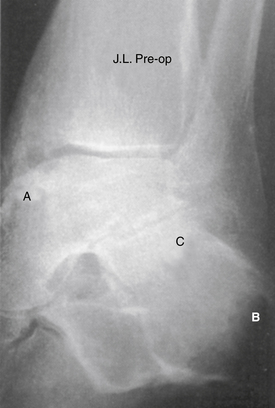
Evaluation for subtalar pathology should include plain radiographs of the ankle and subtalar joints. The Broden view provides the best visualization of the posterior subtalar joint and may be sufficient to confirm the diagnosis of subtalar pathology (Fig.18-3). Profound degenerative radiographic changes in the joint are not needed to confirm a diagnosis, because only small alterations in the biomechanics of this joint can produce significant symptoms. Computerized tomography (CT) is best able to define the bony anatomy, and with thin sections, scanning reconstructions in the axial, coronal, and sagittal planes can be performed. Magnetic resonance imaging (MRI) can be used to confirm associated bony changes such as subchondral bone edema and may be useful in evaluating the adjacent soft tissues to rule out other causes of hindfoot pain. Bone scanning and arthrography are usually not required, and these studies have largely been replaced by MRI.
TREATMENT
Indications and Contraindications
The contraindications to arthroscopic subtalar arthrodesis include prior failed subtalar fusions, gross malalignment requiring correction, infection, and significant bone loss. A patient with moderate malalignment may be a candidate for in situ stabilization. Although significant bone loss has not frequently been encountered, moderate bone loss has not presented a serious problem in a study of arthroscopic ankle arthrodesis.15
Arthroscopic Technique
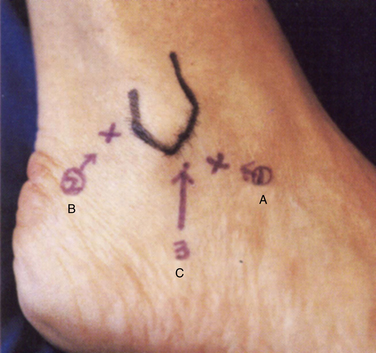
The anterolateral and the posterolateral portals are conventionally used. An accessory portal usually needs to be established approximately 1 cm posterior to the anterolateral portal (Fig. 18-4). This portal can be used for debridement or for outflow enhancement and may occasionally be used for visualization. The anterolateral and posterolateral portals are used in an alternating manner for viewing and for instrumentation. If significant arthrofibrosis makes entry and visualization difficult, the accessory anterolateral portal is quite useful.
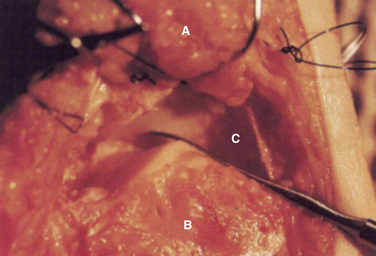
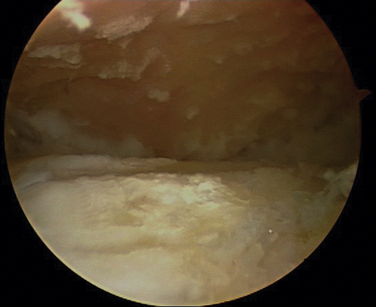
It is important to confirm that the arthroscope is in the subtalar joint and that the ankle joint or the fibular talar recess have not been inadvertently entered. All débridement and decortication is done posterior to the interosseous ligament because only the posterior facet is fused (Fig. 18-5). The middle and anterior facets are not seen under normal circumstances unless the interosseous ligament is absent. Most of the procedure is performed with the arthroscope in the anterolateral portal and the instruments in the posterolateral portal. The remaining débridement is accomplished by alternating the use of these portals.
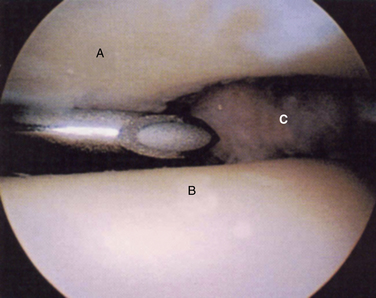
FIGURE 18-5 An arthroscopic view of the subtalar joint shows the talus (A), calcaneus (B), and posteromedial corner (C).
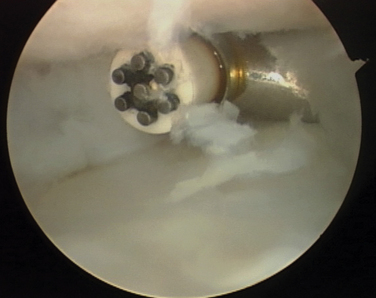
At the beginning of the procedure, a primary synovectomy and debridement are necessary for visualization, usually through the accessory anterolateral portal (Fig. 18-6). The articular surface is debrided, making the joint more capacious and making the use of instrumentation easier. Complete removal of the articular surface down to subchondral bone is performed next (Figs. 18-7 and 18-8). The unique talocalcaneal geometry requires a variety of instruments, including straight and angled curettes and a complete set of shavers and burrs.
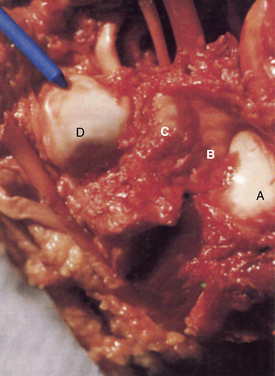
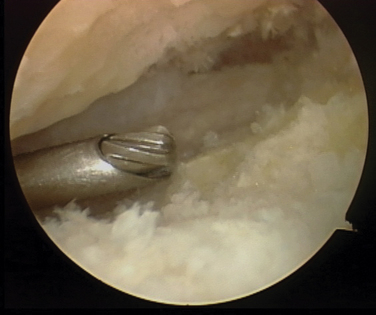
After the articular cartilage has been resected, approximately 1 to 2 mm of subchondral bone is removed to expose the highly vascular cancellous bone. Care must be taken not to alter the articular surface geometry and not to remove excessive bone because this will lead to poor coaptation of the joint surfaces. After the subchondral plate is removed, small “spot-weld” holes approximately 2 mm deep are fashioned on the surfaces of the calcaneus and talus to create vascular channels (Fig. 18-9). Careful assessment of the posteromedial corner must be made, because residual bone and cartilage can interfere with talocalcaneal coaptation. The curette often safely breaks down this corner and can provide the surgeon with tactile feedback. The neurovascular bundle is located in the posteromedial corner, and it must be protected throughout the procedure.
The fusion is fixed with a large, cannulated, 7.5-mm screw. The guide pin is started at the dorsal anteromedial talus and angled posterior and inferior to the posterolateral calcaneus; however, it does not violate the calcaneal cortical surface. Using fluoroscopy, the guidewire is placed with the ankle in maximum dorsiflexion to avoid screw head encroachment or impingement on the anterior lip of the tibia (Fig. 18-10). After the guidewire is placed, the ankle can be relaxed, the screw inserted under fluoroscopic control, and the fusion site compressed (Fig. 18-11). The screw runs along the natural axis of rotation of the subtalar joint using this technique. Starting the screw from the dorsal and medial aspect of the talus avoids painful screw head prominence over the calcaneus and reduces the need for a second procedure to remove the screw. There have been no fractures or complications with this particular fixation technique.15 An alternate method of fixation uses a single screw placed from the calcaneus into the talus in the appropriate direction.
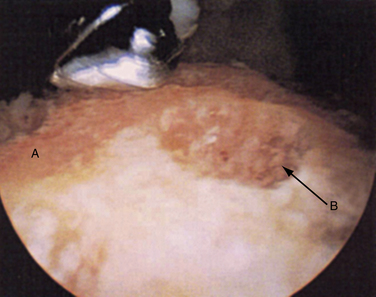
FIGURE 18-9 The superior surface of the calcaneus (A) is shown after decortication and “spot welding” (B).
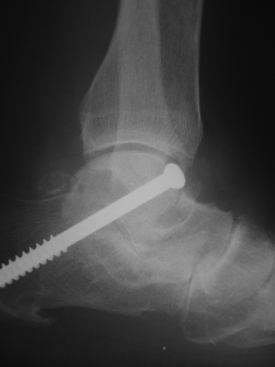
FIGURE 18-11 A 7.3-mm, partially threaded, cannulated screw is used to achieve fixation across the subtalar joint.
PEARLS& PITFALLS
PEARLS
PITFALLS
RESULTS OF TREATMENT AND COMPLICATIONS
Since September 1992, we have followed 25 consecutive patients undergoing arthroscopic subtalar fusion, and there has been sufficient follow-up time to determine the effectiveness of the procedure. Fusion rate, time until complete union, surgical technique, and the complication rate were analyzed. One standard surgical procedure was used, and the method of internal fixation was consistent throughout this study. The posterior subtalar joint was the only joint fused during this procedure. Three of the 25 patients had a combined arthroscopic ankle and subtalar fusion. In this study, 8 patients had osteoarthritis, 10 had post-traumatic arthritis, 4 had posterior tibial tendon dysfunction, 2 had rheumatoid arthritis, and 1 patient had a talocalcaneal coalition. Every patient had a radiographic evaluation at 2-week intervals to determine the rate and quality of fusion. Clinical and radiographic forms of evidence were required to categorize an arthrodesis as completely fused. The parameters required for a successful arthrodesis are evidence of bone consolidation across the subtalar joint, no motion at the screw, the absence of pain with weight bearing, and pain-free forced inversion and eversion. The mean follow-up time was 22 months (range, 6 to 92 months). The subtalar joint of all 25 patients had united clinically and radiographically; the average time until complete fusion was 8.9 weeks (range, 6 to 16 weeks).15
COMPARISON OF PROCEDURES
Glanzmann conducted a prospective analysis of 41consecutive arthroscopic subtalar arthrodeses. The average modified American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score improved from 53 points (range, 22 to 69) preoperatively to 84 points (range, 41 to 94) at the final follow-up assessment (average, 55 months). Union was achieved in all cases.17 These data echo the results demonstrated by Tasto and colleagues,22 showing reproducible excellent results with arthroscopic subtalar fusion.
In a comparison of open and arthroscopic isolated subtalar arthrodesis, Scranton reported a union rate of 100% in the five arthroscopic procedures and one nonunion in the 17 open procedures.12 This was a small study with limited statistical power, and a larger, prospective, randomized trial is needed before a direct comparison of open versus arthroscopic subtalar arthrodesis can be made. However, some studies show a trend toward higher fusion rates with the use of arthroscopic procedures. Easley and coworkers4 reported a union rate of 84% for 148 patients who had isolated open subtalar arthrodesis, compared with the 100% rate of union in the two arthroscopic studies performed by Tasto and Glanzmann.22 Smoking, the presence of more than 2 mm of avascular bone at the arthrodesis site, and the failure of a previous operative procedure were identified as factors contributing to a less favorable union rate.4 Perhaps the observed higher fusion rate in the arthroscopic cohort reflects the preservation of the blood supply and the ability to initiate early weight bearing. One disadvantage of arthroscopic subtalar arthrodesis is that it requires a high level of experience in ankle and subtalar arthroscopy.
In the original technique for arthroscopic subtalar arthrodesis reported by Tasto,22 the arthroscope enters the subtalar joint from the lateral position. This approach has been demonstrated to be safe and reliable.15 Amendola has added to the literature by describing a posterior arthroscopic subtalar arthrodesis.18,19
There are advantages to prone positioning. Parisien and Vagsness14 found that posterior lesions and loose bodies were seen and treated more effectively through two posterior portals when the limb was situated prone. There is concern, however, that the tibial nerve, the posterior tibial artery, and the medial calcaneal nerve are at risk when the posteromedial portal is used.20–23 Voto and colleagues23 found that the posteromedial portal is “potentially hazardous” even if placed adjacent to the Achilles tendon. Ferkel21 reported a series of 612 ankle arthroscopies with a neurologic complication rate of 4.4%. He recommended against use of anterocentral, trans-Achilles, and posteromedial portals.
Acevedo and coworkers24 demonstrated that coaxial posteromedial and posterolateral portals were safe, effective, and reproducible. Sitler and colleagues,25 in a cadaver study with the limb prone, demonstrated an average distance between the posteromedial portal and the tibial nerve, posterior tibial artery, and medial calcaneal nerve of 6.4 mm, 9.6 mm, and 17.1 mm, respectively. Based on these results, some consider the posteromedial portal to be safe, provided it is kept directly adjacent to the Achilles tendon and the patient is in the prone position.
1. Goldner JL, Poletti SC, Gates HS, Richardson W. Severe open subtalar dislocations. J Bone Joint Surg Am.. 1995;77A:1075-1079.
2. Huang PJ, Fu YC, Cheng YM, Lin SY. Subtalar arthrodesis for late sequelae of calcaneal fractures. fusion in situ versus fusion with sliding corrective osteotomy, Foot Ankle Int. 201999 166-170.
3. Rammelt S, Zwipp H. Calcaneus fractures. facts, controversies and recent developments, Injury. 352004 443-461.
4. Easley ME, Trnka HJ, Schon LC, Myerson MS. Isolated subtalar arthrodesis. J Bone Joint Surg Am. 2000;82A:613-624.
5. Lundeen RO. Arthroscopic fusion of the ankle and subtalar joint. Clin Podiatr Med Surg. 1994;11:395-396.
6. Mann RA, Beaman DN, Horton GA. Isolated subtalar arthrodesis. Foot Ankle Int. 1998;19:511-519.
7. Stroud CC. Arthroscopic arthrodesis of the ankle, subtalar, and first metatarsophalangeal joint. Foot Ankle Clin. 2002;7:135-146.
8. Amendola A, Lammens P. Subtalar arthrodesis using interposition iliac crest bone graft after calcaneal fracture. Foot Ankle Int. 1996;17:608-614.
9. Buch BD, Myerson MS, Miller SD. Primary arthrodesis for the treatment of comminuted calcaneal fractures. Foot Ankle Int. 1996;17:61-70.
10. Crosby LA, Yee TC, Formanek TS, Fitzgibbons TC. Complications following arthroscopic ankle arthrodesis. Foot Ankle Int. 1996;17:340-342.
11. Dahm DL, Kitaoka HB. Subtalar arthrodesis with internal compression for post-traumatic arthritis. J Bone Joint Surg Br. 1998;80B:134-138.
12. Scranton PE. Comparison of open isolated subtalar arthrodesis with autogenous bone graft versus outpatient arthroscopic subtalar arthrodesis using injectable bone morphogenic protein-enhanced graft. Foot Ankle Int. 1999;20:162-165.
13. Godberger MI, Conti SF. Clinical outcome after subtalar arthroscopy. Foot Ankle Int. 1998;19:462-465.
14. Parisien JS, Vangsness T. Arthroscopy of the subtalar joint. an experimental approach, Arthroscopy. 11985 53-57.
15. Tasto JP, Frey C, Laimans P, et al. Arthroscopic ankle arthrodesis. Instr Course Lect. 2000;49:259-280.
16. Ferkel RA. Arthroscopic Surgery. The Foot and Ankle. 1996 Lippincott-Raven Philadelphia, PA
17. Glanzmann MC, Sanhueza-Hernandez R. Arthroscopic subtalar arthrodesis for symptomatic osteoarthritis of the hindfoot. Foot Ankle Int. 2007;28:2-7.
18. Amendola A, Lee KB, Saltzman CL, Sub JS. Technique and early experience with posterior arthroscopic subtalar arthrodesis. Foot Ankle Int. 2007;28:298-302.
19. Lee KB, Saltzman CL, Suh JS, et al. A posterior 3 portal arthroscopic approach for isolated subtalar arthrodesis. Arthroscopy. 2008;24:1306-1310.
20. Feiwell LA, Frey C. Anatomic study of arthroscopic portal sites of the ankle. Foot Ankle. 1993;14:142-147.
21. Ferkel RD. Complications in ankle and foot arthroscopy. In: Ferkel RD, Whipple TL, editors. Arthroscopic Surgery: The Foot and Ankle. Philadelphia, PA: Lippincott-Raven; 1996:291-304.
22. Tasto JP. Subtalar arthroscopy. In: McGinty JB, Burkhart SS, Jackson RW, et al, editors. Operative Arthroscopy. 3rd ed. New York: Lippincott Williams & Wilkins; 2002:944-952.
23. Voto SJ, Ewing JW, Fleissner PR. Ankle arthroscopy. neurovascular and arthroscopic anatomy of standard and trans-Achilles tendon portal placement, Arthroscopy. 51989 41-46.
24. Acevedo JI, Busch MT, Ganey TM, et al. Coaxial portals for posterior ankle arthroscopy. an anatomic study with clinical correlation on 29 patients, Arthroscopy. 162000 836-842.
25. Sitler DF, Amendola A, Bailey CS, et al. Posterior ankle arthroscopy. an anatomic study, J Bone Joint Surg Am. 84A2002 763-769.