CHAPTER 9 Arthroscopic Evaluation and Diagnosis of the Patellofemoral Joint
In this chapter, we will focus on the following:
 Specific pathologies (radiologic assessment, arthroscopic findings)—patellofemoral pain, chondromalacia, osteochondritis dissecans (OCD), instability, patellar maltracking
Specific pathologies (radiologic assessment, arthroscopic findings)—patellofemoral pain, chondromalacia, osteochondritis dissecans (OCD), instability, patellar maltrackingPATIENT EVALUATION
History and Physical Examination
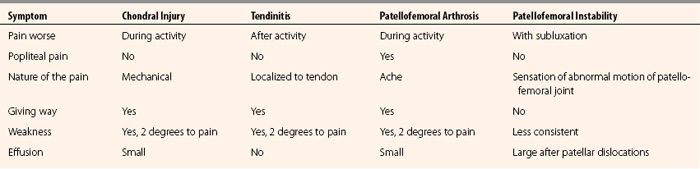
Differentiating acute from chronic problems, the quality of the patient’s pain, and what makes it better and worse all help the clinician make the diagnosis. Table 9-1 presents the major subjective differences when taking a history of a patient’s problem with patellofemoral complaints.
The physical examination should be performed with the goal of systematically evaluating the entire lower extremity. Patellofemoral problems can stem from malalignment secondary to femoral anteversion, genu recurvatum, genu varum, genu valgum, tibial torsion, pes planus, or ligamentous laxity. The extensor mechanism should be evaluated, as well as patellar position, mobility, and tracking.
Next, the examiner should evaluate the joints above and below the knee (hip along with the foot and ankle). It is easy to focus on the knee and patellofemoral joint. Examine all aspects of the knee prior to focusing on the suspected patellofemoral problem (Table 9-2).
| Parameter | Features | Abnormal Findings |
|---|---|---|
| Observation | Alignment | Varus, valgus, patella (alta, baja, or squinting), decreased foot progression angle, pes planus (increased forefoot pronation) |
| Palpation | Knee joint | Effusion, tenderness, crepitus, pain with patellar compression on ROM |
| Range of motion (ROM) | Passive and active | Amount of ROM, limited end points, extensor lag |
ASIS, anterosuperior iliac spine.
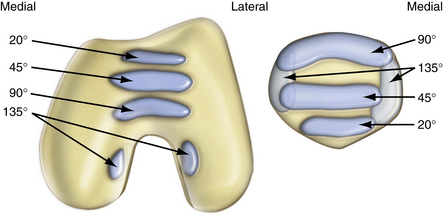
Anatomy
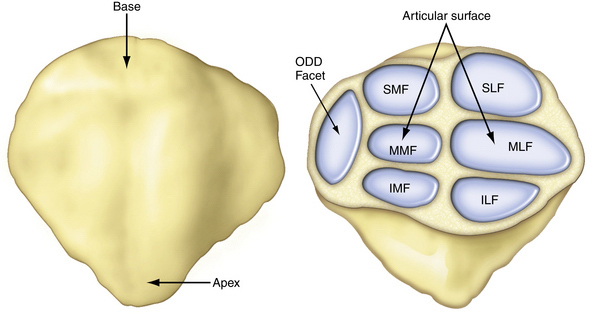
The anatomical landmarks of the patellofemoral joint are the seven facets of the posterior patella (Fig. 9-1). The medial and lateral facets are each divided into roughly equal thirds and the seventh facet is the odd facet located on the extreme medial border of the patella. On the trochlear side, the patella articulates with the femoral joint surface on the medial and lateral sides of the trochlear groove. The contact area pressures vary in location and load depending on the level of flexion. The patellofemoral contact, load, and tracking are also affected by anatomical variants, as described by Wiberg and Baumgartl (Fig. 9-2). Also, anatomic abnormalities such as patella baja, patella alta, trochlear dysplasia, rotational alignment of the femur and tibia, foot alignment, tight lateral retinaculum, and vastus medialis strength also play a role in the tracking and articulating pressures and contact locations (Fig. 9-3).
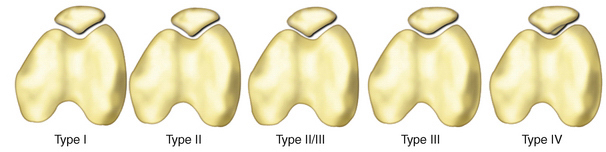
FIGURE 9-2 Anatomic variants of the patella as described by Wiberg and Baumgartl.23 I. Equal medial and lateral facets which are both slightly concave (normal anatomy), II. Smaller medial than lateral facet, medial facet is flat or slightly convex, III. Very small medial facet which is convex, IV. Without a medial ridge or medial facet.
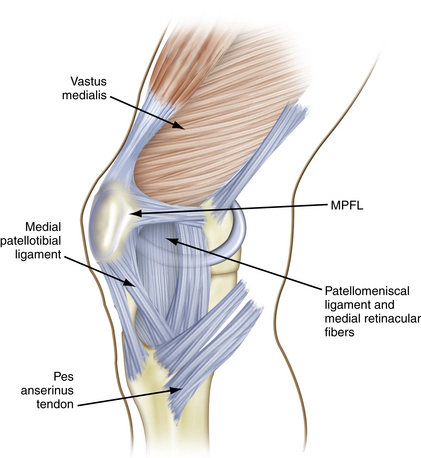
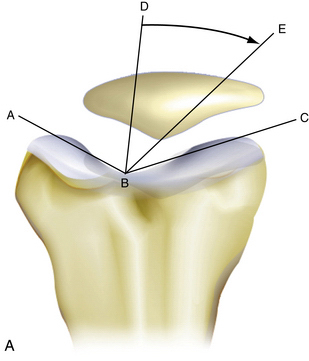
FIGURE 9-3 Anatomy of the medial aspect of the knee. The MPFL provides 53% of the restraint to lateral displacement of the patella. The patellomeniscal ligament and medial retinacular fibers are responsible for 22% of patellar restraint.
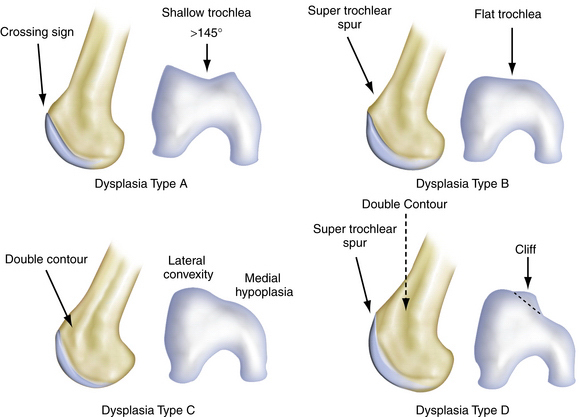
Anatomic variations responsible for patellofemoral problems vary, depending on the pathology. Excessive femoral anteversion, tibial torsion, patella alta, and shallow trochlea are all causes of patellar instability, and pain caused by instability (Fig. 9-4).
Diagnostic Imaging
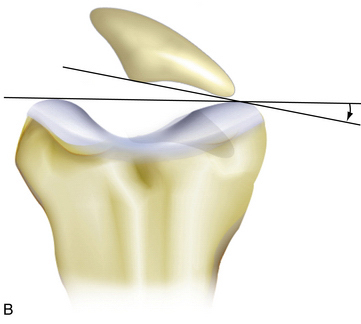
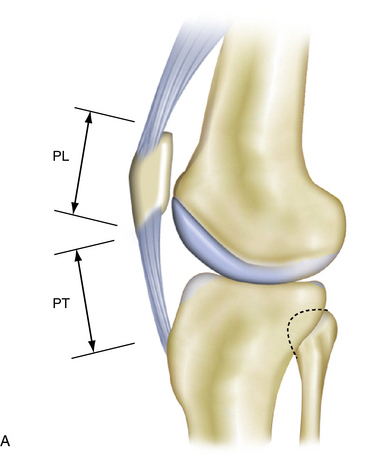
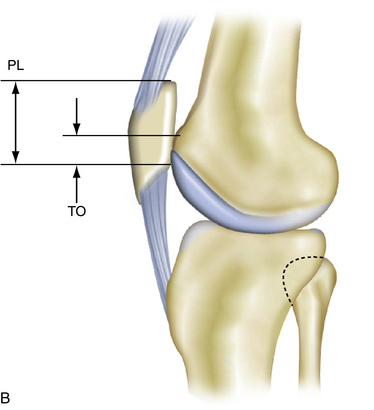
When the patella does not engage in the trochlea by 15 to 20 degrees of knee flexion, patella alta may be present. Patella alta may be radiographically assessed in many ways. Laurin and Merchant axial radiographs are obtained with the knee flexed 20 and 40 degrees, respectively (Fig. 9-5). These assess patellar tilt, but one tangential radiograph obtained at 30 degrees of flexion is sufficient in most cases. The x-ray beam is projected caudad at an angle of 30 degrees from the plane of the femur. A line is drawn along the lateral facet of the patella, and a second line is drawn between the condyles of the trochlea anteriorly. Normally, the angle between these two lines will be open laterally. However, if the lines are parallel or the angle opens medially, the patella is probably tilted.
Teitge and colleagues1 have described a radiographic technique that can be helpful for diagnosing patellar instability. They obtained bilateral axial radiographs of the patellofemoral joints in anatomic position, with constant medial and lateral force applied to the patellae with an instrumented device, and then axial radiography was repeated. It was found that a 4-mm increase in medial or lateral patellar excursion compared with the patellar excursion on the asymptomatic knee correlated with patellar instability. Stress radiographs are helpful in identifying patients with congruity of the articular surfaces whose knees may subluxate or dislocate because of deficient ligamentous structures. Patients who are unable to relax the extensor mechanism because of pain or who have bilateral symptoms are not candidates for stress radiography.
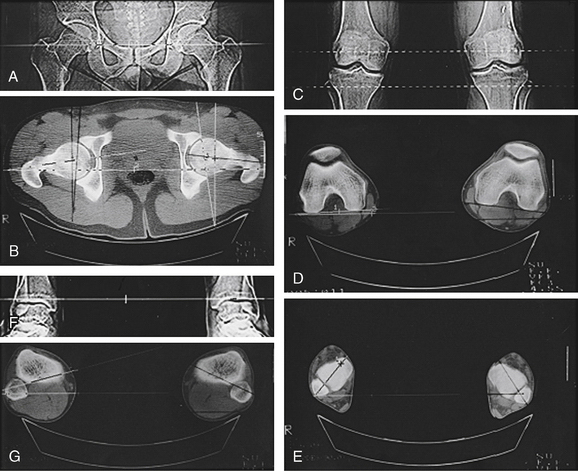
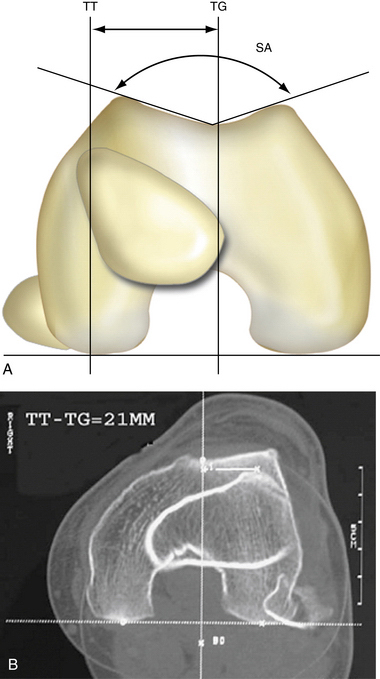
Once x-rays have been evaluated, limb alignment may be further evaluated for rotational malalignment with an overlay alignment CT scan to measure femoral anteversion and tibial torsion. CT has been shown to be more sensitive than axial radiography in delineating patellar malalignment2; it allows axial cuts of the patellofemoral articulation at angles less than 20 degrees of knee flexion, which enhances the detection of subluxation as the patella loses the stabilizing function of the lateral femoral condyle. Another role for CT is in identifying lateralization of the tibial tubercle, as measured by the distance between the tibial tubercle and the trochlear sulcus (Fig. 9-6). An axial CT image demonstrating the femoral trochlear groove is superimposed on an axial image of the tibial tubercle. A line is drawn on this superimposed image between the posterior margins of the femoral condyles. Two lines are drawn perpendicular to this line, one bisecting the femoral trochlear groove and the other bisecting the anterior tibial tuberosity. The distance between these two lines determines the extent of lateralization of the tibial tubercle. Values greater than 9 mm have been shown to identify patients with patellofemoral malalignment, with a specificity of 95% and a sensitivity of 85%.3
The mean tibial tuberosity-trochlear groove (TTTG) distance is 12 mm in the normal knee. However, in people with a history of patellar dislocation, it has been shown to be more than 20 mm (as measured by CT, with the knee extended) in 56% of individuals (Fig. 9-7).4 There has been an association between trochlear and patellar dysplasia and patellofemoral arthritis. Of individuals with isolated patellofemoral osteoarthritis, 42% had a Wiberg type II patella.5 The sulcus angle and TTTG distance have been shown to have the strongest correlations with patellar instability.6
A rotational CT scan is used to look at femoral anteversion and tibial torsion. Normal measurements for femoral anteversion vary widely and there is significant controversy regarding acceptable normal levels. The femoral anteversion range is 14 to 28 degrees, whereas the mean tibiofibular torsion range is 16 to 50 degrees.7
MRI is more effective at identifying articular-cartilage damage directly for large lesions or indirectly by changes in the underlying bone for smaller lesions. Sallay and associates8 have used MRI to visualize the pathoanatomic features of patellar dislocations. They identified the essential lesion of patellar dislocations as a tear of the medial patellofemoral ligament (MPFL) off the femoral insertion. The location of the injury was confirmed by surgical exploration. Although other authors have identified avulsions of the MPFL from the patella with the use of MRI alone, this is an uncommon location for injury and may be overinterpreted on MRI studies of patients.
Joint Geometry
Stability of the patellofemoral joint is dependent on the shape of the trochlear groove and the steepness of the slope of the patellar facets. The trochlear groove was first analyzed radiographically by Merchant with the skyline radiographic view performed at 45 degrees of knee flexion. This assesses the patellar position within the groove. The congruence angle of Merchant9 is used to identify lateral translation and the lateral patellar angle of Laurin is used to identify lateral tilt.10
The lateral facet of the patella is responsible for 60% of the load across the normal patellofemoral joint. As the knee flexes, the contact force on the patellofemoral joint increases. Conversely, as the knee moves toward full extension, the contact force decreases and the patella leaves the trochlear groove as it moves proximally. At this point, the patella is dependent on the soft tissues for lateral stability. Contact points on the femoral trochlea and patella change as the knee flexes more (Fig. 9-8).11 The starting point of the patella is lateral, with a catching mechanism that moves the patella medially into the trochlear groove at initial flexion. The patella then tracks in the trochlear groove moving distally, laterally, and posteriorly in line with the groove orientation.
The amount of load across the patella increases with the degree of flexion, so that at 20 degrees the load across the patellofemoral joint is more proximal in the trochlear groove and more distal on the patella. The load across the patellofemoral joint increases with larger vector forces associated with increased knee flexion. The loads are larger more distally on the trochlea and, as noted, the lateral facet translates 60% of this load. The patellar surface that articulates with the femur changes from distal to proximal on the patella. Therefore, the larger loads seen on the patella are more proximal.12 The forces have been estimated to increase to 20 times body weight with jumping, 7.6 times with deep squats, and 3.3 times with stairs.13
Therefore, abnormal loads resulting in cartilaginous damage are usually seen in the areas represented by higher flexion with chronic patellofemoral osteoarthritis (OA). Loads are also seen to be higher in knees with patella alta (Fig. 9-9). However, in cases of patellar instability and maltracking, the areas of pathologic findings represent the cause of the maltracking. A subluxating patella will be damaged with the dislocation and, more specifically, relocation of the patella, whereas a lateral tracking patella will have increased wear of the lateral facet and lateral trochlea.
Classification of Patellofemoral Disorders
A clinical classification of patellofemoral disorders was developed by Merchant14 based on cause. The five major categories are trauma, patellofemoral dysplasia, idiopathic chondromalacia patella, osteochondritis dissecans, and synovial plicae. Also, pigmented villonodular synovitis (PVNS) can present as an asymptomatic finding, but can cause patellofemoral pain.15 In this chapter, we will present examples of these different causes of patellofemoral problems and their arthroscopic presentations.
Holmes and Clancy16 have proposed a clinical classification of anterior knee pathology that has three major classification classes: patellofemoral instability, patellofemoral pain with malalignment, and patellofemoral pain without malalignment (Box 9-1).
Box 9-1 Holmes-Clancy Clinical Classification of Anterior Knee Pathology
Patellofemoral Instability
TREATMENT
Arthroscopic Assessment of the Patellofemoral Joint
Position and Setup
Once the patient is prepped and draped, marks for the portals should be made. The superomedial portal is placed 2 cm above the superomedial pole of the patella, just medial to the central quadriceps tendon. This is a portal favored by Pidoriano and Fulkerson.17
However, Grana and coworkers18 have found that viewing patellar tracking is equivalent from a superior or inferior portal. Nissen and colleagues19 have favored the use of standard arthroscopic portals. The other three standard portals include the inferior lateral, inferior medial, and superior lateral portals. All portals can be used to maximize the visualization of the patellofemoral joint, as well as the rest of the knee joint. The use of the superomedial portal has the benefit of being less impaired if a post is used during arthroscopy compared with the superolateral portal. However, the superolateral portal may provide a better view of the lateral facet of the patella and the lateral side of the trochlea.
Technique
As with any arthroscopic procedure of the knee, this is initiated with a thorough history and physical and imaging protocol. After this is carried out and determining that surgery is appropriate for an individual patient, many decisions are required. We find that the arthroscopic procedure performed for a patient with an isolated patellofemoral problem is often one of confirmation and/or exclusion of other diagnoses. By the time the patient and surgeon have decided an arthroscopic procedure should be performed, all nonoperative solutions have been exhausted. A decision to perform a specific procedure for the treatment of a problem, such as a medial patellofemoral ligament reconstruction for patellofemoral instability, has been made. Most surgeons prefer to perform a diagnostic arthroscopy prior to performing the definitive procedure that has been chosen.
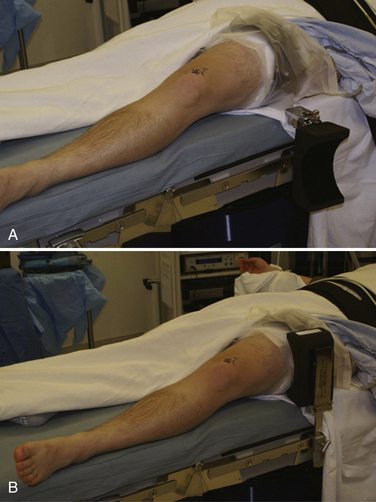
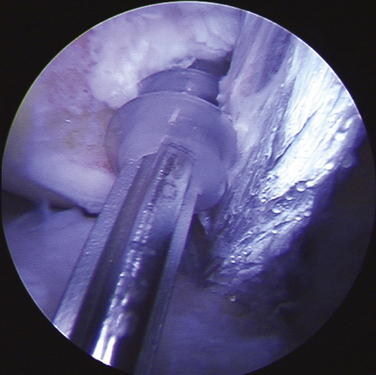
After examination, a tourniquet is applied to the leg prophylactically. We generally do not inflate the tourniquet unless necessary during the case for visualization purposes. Use of a leg holder versus a side post is left to the surgeon’s preference. We use a side post that can be flipped down to allow complete access to the superior aspect of the knee for accessory portals (Fig. 9-10).
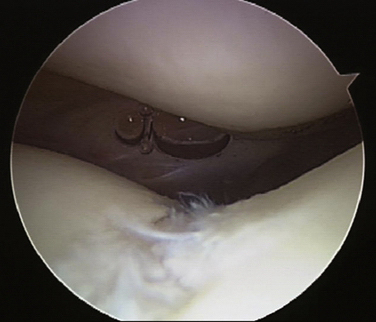
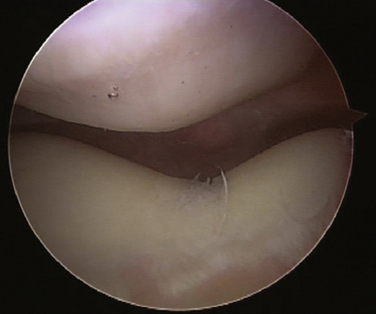
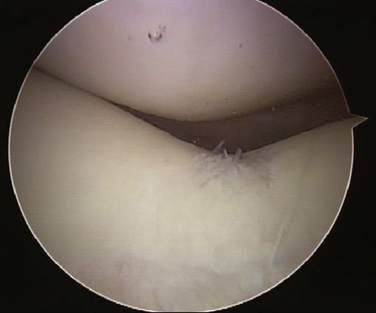
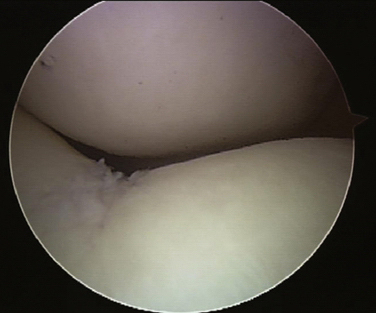
Initial evaluation after prepping and draping is performed through an inferior lateral patella portal (Fig. 9-11); care must be made to place this portal laterally enough away from the patella tendon and inferior enough from the patella so that easy manipulation up into the patellofemoral joint can be performed without injuring the articular cartilage. We prefer to perform the routine evaluation of the patellofemoral joint, medial gutter, medial compartment, lateral compartment, and intercondylar notch, perform the posterior examination, and then concentrate on the involved pathology in the patellofemoral region. It is important to understand that fluid placed under pressure with a pump or gravity will affect normal mechanics within the knee. Also, the portals used can affect the patella and put it in a less than physiologic position when evaluating the knee. The superomedial portal can be useful in visualizing patellar tracking as well as looking at the angle of tilt of the patella (Fig. 9-12). The lateral facet should align with the trochlear groove by 20 to 25 degrees of knee flexion (Fig. 9-13) and the apex of the patella by 35 to 40 degrees of knee flexion (Fig. 9-14).
Grading of all articular cartilage lesions should be performed at this time, as well as sizing them and locating them geographically on the patella and trochlear groove. This should be documented by videography or drawings at the conclusion of the procedure, which can then be used by the surgeon and patient to plan definitive treatment if none has been done during the procedure.
Evaluation of Joint Surfaces to Help Determine Treatment Options
Cartilage Lesions
The patellofemoral joint must first be assessed by the much less invasive techniques of x-ray evaluation using the sunrise view and the 30-degree bent knee lateral view and AP view of the knee. The most relevant x-ray is the sunrise view taken at 20 degrees of flexion. Kijowski and colleagues20 have found that the most sensitive radiographic findings for degeneration of articular cartilage in the patellofemoral joint are marginal osteophytes. Joint space narrowing, subchondral sclerosis, and subchondral cysts were noted to be insensitive for osteoarthritis of the patellofemoral joint. MRI has also been used to assess the patellofemoral joint. Advantages include direct visualization; it is the most sensitive and specific diagnostic test available.
The patellofemoral joint surface may be examined directly with arthroscopy. Gomes and associates21 have proposed a technique to assess the articular surface of the patella for cartilage breakdown more effectively. They used a Kirschner wire to maintain a 45-degree lateral tilt after a lateral retinacular release. However, a lateral retinacular release can be counterproductive and even devastating in some patients, specifically those with an already hypermobile patella. This technique, however, could be used to assist in some operative procedures to address chondral deficits.
If a patient has patellofemoral pain that presents as an articular type of pain, it may be treated conservatively, and often improves. However, if the pain persists for a prolonged follow-up period, it may then be necessary to assess the joint surfaces and treat the patient surgically. There has traditionally been a poor correlation between patellofemoral pain and patellofemoral cartilage lesions. Kettunen and coworkers,22 however, have found that patients who had patellofemoral pain syndrome were more likely to have severe lesions of the patella or trochlear surfaces. These patients also had more functional limitations than patients with mild or no lesions. Assessment of the articular surface is done using the modified Outerbridge classification (Table 9-3).
TABLE 9-3 Modified Outerbridge Classification of the Articular Surface
| Grade | Macroscopic Description |
|---|---|
| 0 | Normal |
| I | Softening or swelling |
| II | Fissuring or small erosions |
| III | Fragmentation, fissuring, deeper erosions, but not to subchondral bone |
| IV | Erosions down to subchondral bone |
Findings with patellofemoral arthroscopy may direct our understanding of the cause of patellofemoral pain. The location of pathologic lesions on the patella may help us determine whether the pain and lesions are secondary to malalignment, maltracking, or instability.
Synovitis is usually seen as a diffuse inflammatory response, showing a red inflamed synovium. However, a patient can also have anterior knee pain from PVNS, which, although rare, has been reported.15 In the one reported case, the PVNS was located in the patellofemoral joint (Fig. 9-15).
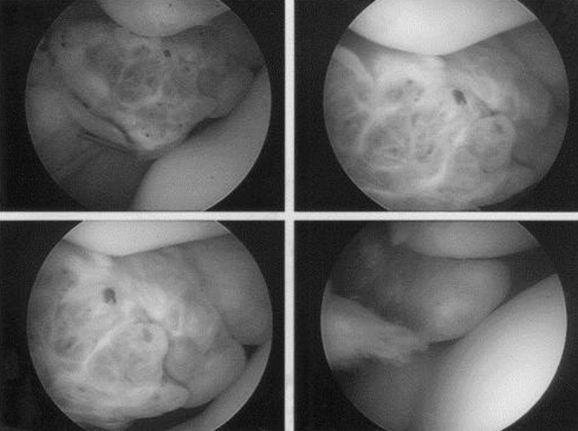
FIGURE 9-15 Example of PVNS in Patellafemoral joint.
(From Edwards MR, Tibrewal S. Patello-femoral joint pain due to unusual location of localized pigmented villonodular synovitis—a case report. Knee. 2004;11:327-329.)
Medial instability is almost always caused by iatrogenic overrelease of the lateral retinaculum. In the past, this was overused as a method of treatment of lateral tracking because of the ease and speed of the procedure. The assumption was that the release of a tight lateral retinaculum would solve the patellar tracking problems. It is now believed that an isolated lateral release is almost never the answer in the treatment of patellofemoral pathology.
1. Teitge RA, Faerber W, Des Madryl P, et al. Stress radiographs of the patellofemoral joint. J Bone Joint Surg Am. 1996;78:193-203.
2. Inoue M, Shino K, Hirose H, et al. Subluxation of the patella: computed tomography analysis of patellofemoral congruence. J Bone Joint Surg Am. 1988;70:1331-1337.
3. Jones RB, Barlett EC, Vainright JR, et al. CT determination of tibial tubercle lateralization in patients presenting with anterior knee pain. Skeletal Radiol. 1995;24:505-509.
4. Steensen RN, Dopirak RM, McDonald WG. The anatomy and isometry of the medial patellofemoral ligament: implications for reconstruction. Am J Sports Med. 2004;32:1509-1513.
5. Smirk C, Morris H. The anatomy and reconstruction of the medial patellofemoral ligament. Knee. 2003;10:221-227.
6. Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7:121-127.
7. Seber S, Hazer B,Köse N, et al. Rotational profile of the lower extremity and foot progression angle: computerized tomographic examination of 50 male adults. Arch Orthop Trauma Surg. 2000;120:255-258.
8. Sallay PI, Poggi J, Speer KP, et al. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24:52-60.
9. Merchant AC, Mercer RL, Jacobsen RH, et al. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391-1396.
10. Laurin CA, Levesque HP, Dussault R, et al. The abnormal lateral patella-femoral angle: a diagnostic roentgenographic sign of recurrent patellar subluxation. J Bone Joint Surg Am. 1978;60:55-60.
11. Goodfellow J, Hungerford DS, Zindel M. Patello-femoral joint mechanics and pathology. 1. Functional anatomy of the patello-femoral joint. J Bone Joint Surg Br. 1976;58:287-290.
12. Amis AA. Current concepts on anatomy and biomechanics of patellar stability. Sports Med Arthrosc. 2007;15:48-56.
13. Hungerford DS, Barry M. Biomechanics of the patellofemoral joint. Clin Orthop Relat Res. 1979;(144):9-15.
14. Merchant AC. Classification of patellofemoral disorders. Arthroscopy. 1988;4:235-240.
15. Edwards MR, Tibrewal S. Patello-femoral joint pain due to unusual location of localized pigmented villonodular synovitis—a case report. Knee. 2004;11:327-329.
16. Holmes SW, WG Clancy. Clinical classification of patellofemoral pain and dysfunction. J Orthop Sports Phys Ther. 1998;28:299-306.
17. Pidoriano AJ, Fulkerson JP. Arthroscopy of the patellofemoral joint. Clin Sports Med. 1997;16:17-28.
18. Grana WA, Hinkley B, Hollingsworth S. Arthroscopic evaluation and treatment of patellar malalignment. Clin Orthop Relat Res. 1984;(186):122-128.
19. Nissen CW, Cullen MC, Hewett TE, Noyes FR. Physical and arthroscopic examination techniques of the patellofemoral joint. J Orthop Sports Phys Ther. 1998;28:277-285.
20. Kijowski R, Blankenbaker D, Stanton P, et al. Correlation between radiographic findings of osteoarthritis and arthroscopic findings of articular cartilage degeneration within the patellofemoral joint. Skeletal Radiol. 2006;35:895-902.
21. Gomes JL, Marczyk LR, Ruthner RP. Arthroscopic exposure of the patellar articular surface. Arthroscopy. 2001;17:98-100.
22. Kettunen JA, Visuri T, Harilainen A, et al. Primary cartilage lesions and outcome among subjects with patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2005;13:131-134.
23. Wiberg G, Baumgartl F. Klassification der patelleformen. In: Baumgartl, editor. Das Kniegelenk. Berlin, Germany: Springer; 1964:276.