CHAPTER 29 Arthroscopic Debridement for Isolated Scaphotrapeziotrapezoid Arthritis
Introduction
Degenerative changes of the scaphotrapeziotrapezoid (STT) joint are seen in almost 40% of cadaveric wrists.1 Clinical involvement of the triscaphe joint occurs in 15 to 30% of wrists.2 Concomitant trapeziometacarpal arthritis occurs in the majority of patients, but isolated pathology is present in up to 20% of the population3,4—particularly in postmenopausal women.5 Symptomatically isolated STT disease leads to tenderness over the palmar aspect of the thenar eminence and is an important differential diagnosis in radial wrist pain. Frequently, flexor carpi radialis tendinitis and radiopalmar ganglia are also noted upon examination.6
Previous reports of treatment for STT osteoarthritis (OA) following failed conservative treatment include excisional arthroplasty (with7 or without4 a silicone spacer) and limited wrist fusion, including STT fusion.6 Pain relief is not uniform in these series, and morbidity due to postoperative complications has been noted. Wrist arthroscopy is a useful tool for visualizing articular damage, which can be a source of chronic wrist pain.8 Arthroscopic debridement has proven to be an effective method of achieving pain relief in the knee in two-thirds of patients for up to two to five years and carries a low morbidity.9,10 The authors have successfully used arthroscopic debridement of isolated STT arthritis to improve symptoms in selected patients.
The pain associated with STT arthritis can be surprisingly debilitating and leads to disability when axially loading the thumb during strong pinch and key turning. There are, however, other patients who have minimal symptoms. For example, the patient with a distal radius fracture will often have advanced STT joint arthritis on radiographs but will deny any symptoms. Watson and Ottoni11 suggested rotatory subluxation of the scaphoid as a possible cause of isolated STT arthritis. They noted that early degenerative changes of the STT joint occurred when abnormal unilateral hypermobility of the scaphoid was present. STT arthrodesis has been the traditionally recommended procedure and is noted to give good function and excellent pain relief.6 STT fusion, however, disturbs the usual wrist mechanics—which results in a high incidence of STT nonunion and secondary radial styloid arthritis due to impingement.
Arthroscopy in the Treatment of Arthritis
Arthroscopic debridement and washout remains a popular treatment method for degenerative arthritis in the knee.9,10 Considerable pain relief is noted in a third of patients, lasting into the medium term. Further surgical intervention is required in only a small proportion of those treated. The use of arthroscopy allows for joint assessment and therapeutic interventions.
We had previously treated patients with STT OA with either an excisional arthroplasty consisting of a distal scaphoid pole resection as described by Garcia-Elias et al.4 or STT joint arthrodesis using the technique reported by Watson and Hempton.12 Two of the excisional arthroplasty patients complained of persistent symptoms, and plain radiographs demonstrated increased extension of the scaphoid and the lunate. Some of the patients treated with an STT joint arthrodesis had continuing pain at sites of nonunion. We therefore searched for alternative methods of achieving good pain relief and function without the potential morbidity ensuing from the traditional techniques used to treat STT arthritis. It was felt that the arthroscopy had potential use for joint debridement and joint excision.
It is the authors’ experience that the degenerative changes noted at the time of arthroscopy are more advanced than those reported in recent cadaveric studies.13 This is probably because all patients who require therapeutic intervention have significant pain associated with advanced degenerative osteoarthritis. Moritomo et al. have noted that the most common site of degenerative changes is on the ulnar side of the distal scaphoid and centrally on the trapezoid and trapezium.1 Half of cases have involvement of the trapezoid alone, with the trapezium being involved in only a third.
Patient Selection
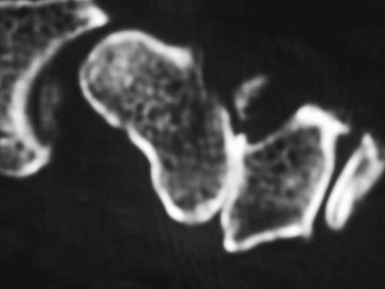
Radiographs showed joint narrowing and osteophyte formation isolated to the STT joint (Figure 29.1). Longitudinal computer tomography (CT) scans were performed, particularly if thumb carpometacarpal (CMC) joint arthritis was suspected (Figure 29.2).14 The thumb CMC joint pain can also be isolated with a diagnostic injection. Typically, the CT scans demonstrated complete loss of the joint space—which was often associated with osteophytes and degenerative cysts within the distal scaphoid. The scaphoid was always extended and the plain radiograph often showed dorsal instability of the lunate.
Surgical Technique
A standardized approach to the arthroscopic debridement is used. The arm is suspended on Chinese finger traps with 5 kilograms of traction.15 No extra or special equipment is required to view the STT joint. Routine arthroscopy was performed with a 2.7-, 2.4-, or 1.9-mm arthroscope. The radial midcarpal arthroscopy (MCR) portal was used to evaluate the midcarpal joint—including the STT joint, which is just the radial extension of the midcarpal joints.15
STT Dorsal
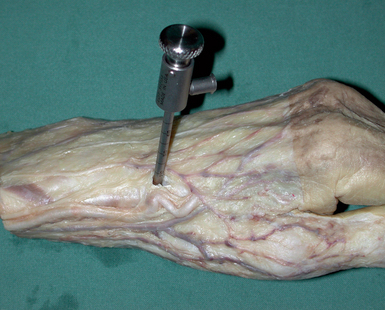
This is the portal radial to the EPL tendon. The authors undertook a cadaveric study to assess the safe positioning of the STT joint portal.13 Placement to the ulnar side of the extensor pollicis longus (EPL) tendon is safer for the radial artery, but the superficial branch of the radial nerve and the extensor carpi radialis longus (ECRL) tendon are still at risk. If the surgeon goes to the radial side of the EPL tendon, the radial artery and superficial branch of the radial nerve are both at risk (Figure 29.3). The radial artery is often tortuous within the “anatomical snuffbox.” The authors recommend a “mini-open” approach with a 1.5-cm incision made in the skin to enable safe blunt dissection. This mini-open approach minimizes the risk to the neurovascular structures. The portal to the radial side of the EPL tendon provides a wider span from the radial midcarpal portal, facilitating triangulation.
STT Volar Portal
This is the volar to abductor pollicis longus.16 Bare describes an alternative palmar portal to facilitate the visualization of the dorsal rim of the STT joint.16 This portal is located 3 mm ulnar to the abductor pollicis tendon, 6 mm radial to the scaphoid tubercle, and midway between the radial styloid and the base of the thumb metacarpal.
STT Ulnar Portal
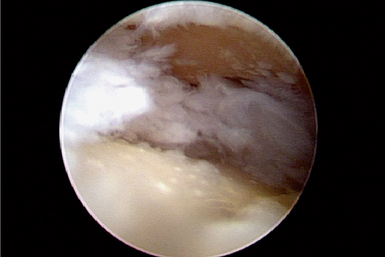
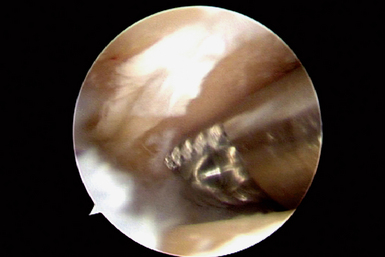
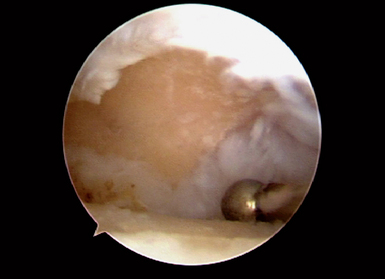
This accessory portal is just ulnar to the EPL tendon.17 In difficult cases, portable operative fluoroscopy can assist in identifying the joint. The presence of eburnated bone on the distal scaphoid and proximal trapezium and trapezoid was recorded (Figure 29.4). Synovitis in the joint is usually present (Figure 29.5). The eburnated bone was not removed, but any synovitis, chondral flaps, or rim osteophytes were debrided with an arthroscopic bur and resector. Any synovitis on the volar aspect of the joint was removed.
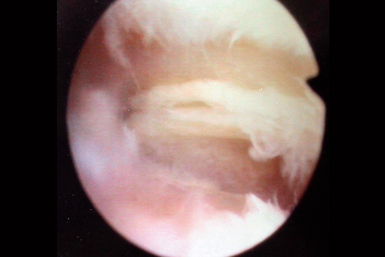
FIGURE 29.4 Arthroscopic view of the trapezium (foreground) and the trapezoid (background) with eburnated bone.
A 3- to 5-mm resector (Figure 29.6) can be introduced in most patients to perform the synovectomy. Monopolar cautery can be of assistance (Figure 29.7). The scope and resector are moved among the three portals to provide adequate debridement. Care is taken not to disturb the main ligaments connecting the scaphoid, trapezium, and trapezoid.
Patients with crystalline deposition should be biopsied. The STT joint is a not an uncommon site for CPPD deposition. It is common to have synovitis and chondral changes on the dorsal aspect of the lunate in the midcarpal row. This is a secondary area of degeneration that can also be debrided. The joint was then thoroughly irrigated and the wounds were sutured using an absorbable suture. A light bandage was applied. Following surgery, gentle mobilization was permitted within the patient’s pain tolerance. Return to light duties was recommended from six weeks, and heavy manual labor was avoided for a minimum of three months.
Results
We have previously reported our results in a series of 12 consecutive patients with symptomatic isolated STT arthritis who underwent an arthroscopic debridement.13 Prior to surgery, four patients could be categorized as having fair wrist function (and six poor) based on the modified Green and O’Brien18 wrist scores. All patients had a minimum follow-up of one year, with an average of 36 (range 12 to 80) months. The results are summarized in Table 29.1. The average wrist score following surgery increased by 28 points at the one-year review, with patients now fitting into good4 or excellent6 categories.
Table 29.1 Summary of Results Used to Calculate Wrist Scores13
| Preoperative Score | Most Recent Postoperative Score | |
|---|---|---|
| Pain (visual analog score) | 90 (65–95) | 12 (0–25) |
| Grip strength (kilograms) | 20 (18–36) | 45 (24–52) |
| Green + O’Brien scores (points) | 63 (45–75) | 93 (80–95) |
Summary
Typically, arthroscopic debridement of the STT joint is a minimally invasive procedure with low morbidity. It does not require immobilization and allows early return to work. Our cadaveric studies have demonstrated that caution should be exercised when placing the STT portals because of the risk to branches of the radial artery and the superficial branch of the radial nerve. Using a mini-open approach, with soft-tissue dissection to the capsule, minimizes the risk of neurovascular complication. We continue to use this procedure, which carries a low morbidity and has generally good results. In the authors’ opinion it avoids the high complication rate associated with an STT fusion.
Results for excisional arthroplasty have been less satisfactory in our hands because of synovitis and dorsal instability of the proximal carpal row. Carro et al. reported their results with STT joint debridement, including distal scaphoid excision.19 We have not included the distal scaphoid excision, as it is likely to produce further carpal collapse (as occurs in open distal scaphoid excision).
1 Moritomo H, Viegas SF, Nakamura K, et al. The scaphotrapezio-trapezoidal joint. Part 1: An anatomic and radiographic study. JHS. 2000;25A:899-910.
2 Rogers WD, Watson KH. Degenerative arthritis at the triscaphe joint. JHS. 1990;15A:232-235.
3 Chamay A, Piaget-Morerod F. Arthrodesis of the trapeziometacarpal joint. JHS. 1994;19A:489-497.
4 Garcia-Elias M, Lluch AL, Farreres A, Castillo F, Saffar P. Resection of the distal scaphoid for scaphotrapeziotrapezoid osteoarthritis. JHS. 1999;24A:448-452.
5 Armstrong AL, Hunter JB, Davis TRC. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. JHS. 1994;19A:340-341.
6 Srinivasan VB, Matthews JP. Results of scaphotrapeziotrapezoid fusion for isolated idiopathic arthritis. JHS. 1996;21B:378-380.
7 Eiken O. Implant arthroplasty of the scapho-trapezial joint. Scandinavian Journal of Plastic and Reconstructive Surgery. 1979;13:461-468.
8 Poehling GG, Roth JH. Articular cartilage lesions of the wrist. In: McGinty RN, editor. Operative Arthroscopy. New York: Raven Press; 1991:635-639.
9 Bert JM, Maschka K. The arthroscopic treatment of unicompartmental gonarthrosis: A five year follow-up study of abrasion arthroplasty plus arthroscopic debridement and arthroscopic debridement alone. Arthroscopy. 1989;5:25-32.
10 Dandy DJ. Arthroscopic debridement of the knee. JBJS. 1991;73:877-878.
11 Watson HK, Ottoni L, Pitts EC, Handal AG. Rotatory subluxation of scaphoid: A spectrum of instability. Journal of Hand Surgery [Br]. 1993;18:62-68.
12 Watson HK, Hempton RF. Limited wrist arthrodeses. I. The triscaphoid joint. J Hand Surg. 1980;5(4):320-327.
13 Ashwood N, Bain GI, Fogg Q. Results of arthroscopic debridement for isolated scaphotrapeziotrapezoid arthritis. J Hand Surg [Am]. 2003;28(5):729-732.
14 Bain GI, Bennett JD, Richards RS, Slethaug GP, Roth JH. Longitudinal computed tomography of the scaphoid: A new technique. Skeletal Radiology. 1995;24:271-273.
15 Bain GI, Richards RS, Roth JH. Wrist arthroscopy. In: McGinty DM, Alexander AH, editors. The Wrist and Its Disorders. Second Edition. Philadelphia: W.B. Saunders; 1997:151-168.
16 Carro LP, Golano P, Farinas O, Cerezal L, Hidalgo C. The radial portal for scaphotrapeziotrapezoid arthroscopy. Arthroscopy. 2003;19(5):547-553.
17 Bare J, Graham AJ, Tham SK. Scaphotrapezial joint arthroscopy: A palmar portal. J Hand Surg. 2003;28(4):605-609.
18 Green DP, O’Brien ET. Open reduction of carpal dislocations: Indications and operative technique. Hand. 1978;3A:250-256.
19 Whipple TL. The Wrist. In Arthroscopic Surgery. Philadelphia: Lippincott; 1992.