CHAPTER 10 Arthroscopic Acromioclavicular Joint Reconstruction
PREOPERATIVE CONSIDERATIONS
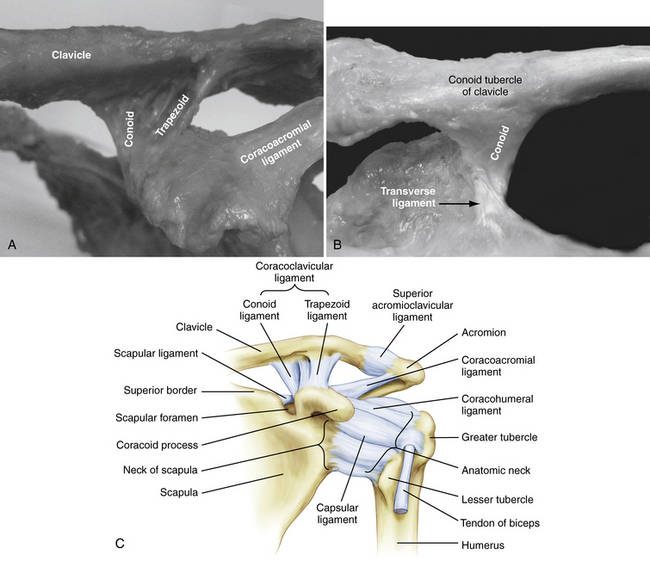
Anatomy of the Native Acromioclavicular Joint
The AC joint complex is a stout articulation anchoring the clavicle and scapula. It provides a pivot point where the clavicle and axial skeleton articulate with the complex motions of the scapula. The complex includes the AC joint proper and the coracoclavicular ligaments. The AC joint proper is a diarthrodial joint that rotates and translates in superior-inferior and anterior-posterior directions. Each side of the joint is covered by hyaline cartilage, with a meniscus-like disk of fibrocartilage interposed. The meniscus-like disk has tremendous variation in size and shape. The exact function of the intra-articular disk is unknown; it has been shown to degenerate with age and to be almost functionless beyond age 40.1–3 The capsule and stabilizing ligaments surround the joint, providing stability.
Multiple structures enhance the stability of the AC joint. Primary static stabilizers are the AC joint ligaments (anterior, posterior, superior, and inferior) and the coracoclavicular ligaments (conoid and trapezoid). Dynamic stabilizers include the deltoid and trapezius muscles. The superior AC ligament has confluence fibers with the enveloping deltotrapezial fascia, which add stability of the joint in motion.4
Horizontal translation of the distal clavicle is restricted mainly by the joint capsule and surrounding AC joint ligaments. Fukuda and colleagues5 have demonstrated that the superior and posterior ligaments contribute approximately 50% and 25% of the resistance, respectively, to posterior translation. This is an important consideration when performing an arthroscopic distal clavicle resection. To avoid the potential complication of posterior impingement of the distal end of the resected clavicle on the spine of the scapula, every effort should be made to preserve the superior and posterior capsule.
The coracoclavicular (CC) ligament complex is comprised of two ligaments.6 As the name implies, the general shape of each is cone-shaped and trapezoidal. Both ligaments are ribbon-like in dimension. The conoid ligament originates on the coracoid posterior to the pectoralis minor and inserts on the clavicle at an average of 46 mm from the distal end. This measurement is to the midportion, or mean, of the ligament insertion. The origin lies on the most posterior and medial portion of a previously unnamed tubercle of the coracoid, sometimes referred to as the knuckle. The insertion is linear and broad, fanning out along the most posterior border of the clavicle in the coronal plane. The clavicle has a small posterior protuberance called the conoid tubercle, where most of the conoid fibers attach. The trapezoid ligament originates just anterior and lateral to the conoid, again on the coracoid knuckle or tubercle. In contrast to the conoid, the trapezoid angles 45 degrees laterally to insert at an average distance of 26 mm from the distal end of the clavicle.4 Its ribbon-like form is oriented in the sagittal plane and is essentially orthogonal to the conoid. Its insertion on the clavicle is linear, spanning the entire width in the anterior to posterior direction. The conoid has been reported to have a more posteromedial origin from the coracoid whereas the trapezoid’s origin on the coracoid lies more anterior and lateral.7 The ligaments span a distance of approximately 1.1 to 1.3 cm and prevent inferior translation of the scapula relative to the clavicle.8 In the absence of AC joint ligaments, the CC ligament complex becomes an important secondary stabilizer of horizontal translation, especially to posterior displacement9 (Fig. 10-1).
Motion of the AC joint is complex and not completely understood. What has been made clear is that the scapula and clavicle have obligatory coupled motion around three axes that is guided by the AC joint and CC ligament complex. Rigid fixation of the AC joint with coracoclavicular screws prevents normal scapulathoracic motion and function.10
Biomechanics of the Acromioclavicular Joint
The biomechanics of native and numerous stabilization and/or reconstruction techniques has been extensively studied and is beyond the scope of this chapter. The native CC complex has been shown to have a biomechanical ultimate load of 500 to 725 N.11–13 The Weaver-Dunn procedure, with its various modifications, has gained much exposure. Despite its popularity, the transferred coracoacromial (CA) ligament has an ultimate load of only 145 N,13 which appears insufficient in strength and stiffness when compared with the native ligament complex.12,14 This may account for the high number of failures reported with its use.15,16
Mazzocca and associates, 17 after reviewing recent biomechanical data, reached several conclusions. First, the popular CA ligament transfer provides only 25% of the strength of the intact CC ligament complex but the biomechanical strength can be improved with synthetic augmentation. The CA ligament transfer, even with suture augmentation, has no effect on anterior-posterior displacement. Finally, the use of a free tendon graft can provide improved initial stability and equivalent strength to the native ligament complex; this represents a biomechanical improvement compared with the traditional CA ligament transfer. It is findings such as these that have prompted the development of the techniques described in the following sections, including the GraftRope (Arthrex, Naples, Fla) and ACCR.
Mechanism and Classification of Acromioclavicular Joint Separations
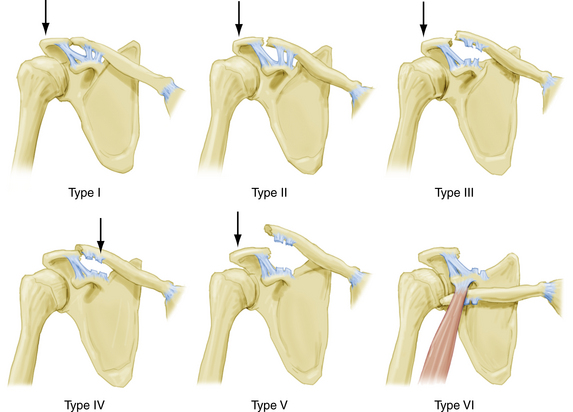
AC joint injuries were first recognized and described by Hippocrates.18 Cadnenat, in 1917, described the sequential failure of AC ligaments, coracoclavicular ligaments and, finally, the deltoid and trapezial fascia.19 Tossy and associates20 have proposed a classification system describing three grades of injury to the AC joint. Rockwood and coworkers21 later expanded the classification to include six grades, and this has become the universally accepted classification system.
Type I injuries are essentially AC joint sprains to the AC ligaments and capsular complex. There is no instability of the AC joint. Type II injuries represent rupture of the AC ligaments and joint capsule with intact CC ligaments. Significantly more force is required for this injury pattern. Generally, less than 50% superior displacement of the clavicle is common, although instability in the anterior-posterior direction is a more consistent finding. Type III injuries occur when both AC and CC ligament complexes are disrupted. There is complete loss of contact between the clavicle and acromion, with 100% displacement. With type IV injuries, there is complete disruption of the AC and CC ligaments, with posterior displacement into or through the trapezius. Type V injuries represent significantly displaced type III injuries, with 100% to 300% displacement, secondary to complete rupture of the deltotrapezial fascia. Finally, the rare type VI injury represents a complete dislocation, with the clavicle displaced inferior, locked beneath the acromion or coracoid process (Fig. 10-2).
History and Physical Examination
The most commonly observed symptom in acute AC joint disruptions is anterosuperior shoulder pain. The pain may be poorly localized at times because of the unique innervations of the AC joint. The AC joint is innervated by both the lateral pectoral nerve and branches off the suprascapular nerve. The pain is usually referred to the anterosuperior shoulder in the region of the AC joint and clavicle, anterior brachium, and anterolateral neck.
In general, the physical examination should begin with unobstructed observation of the patient in the seated position, with the arms held relaxed at the side. Inspection and comparison with the unaffected shoulder and direct palpation will reveal a variable amount of tenderness and deformity. Injury to the AC joint can be identified by localizing pain to the AC joint by direct palpation and/or provocative maneuvers. The diagnosis can be further confirmed by the relief of symptoms following AC joint injection of local anesthetic.10
Physical Findings by Rockwood’s Classification
Type I Injuries.
No deformity would be expected with type I injuries, and often the only positive examination finding is pain with palpation. The AC ligaments have sustained a traction injury but, along with the CC ligament complex, they remain intact. Patients may also complain of pain with the cross-arm adduction maneuver. This test is performed in the seated position with the elbow elevated and flexed to 90 degrees. The arm is brought across the chest compressing the AC joint and will cause discomfort, specifically over the AC joint when positive. O’Brien and colleagues22 have described a useful test to help distinguish pain originating from the AC joint and pain caused by superior labral pathology. The test is performed by adducting the arm in 90 degrees of forward elevation and providing a downward force while resisted by the patient. Reproducible superior shoulder pain while the patient’s arm is in full external rotation implies AC joint pathology, whereas pain or painful clicking described as inside the shoulder with the arm in internal rotation is considered indicative of labral abnormality. Radiographs will be normal.
Type III Injuries.
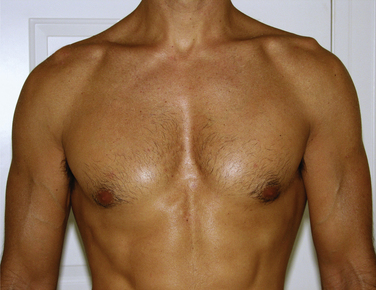
These injuries represent a complete disruption of both AC and CC ligament complexes. The clavicle remains in its relatively normal position because the deltoid and trapezial fascia remains intact but the acromion, scapula, and upper extremity displace inferiorly. The clavicle is unstable in both the horizontal and vertical planes and deformity is obvious on inspection. Range of motion is painful and may elicit palpable crepitus. The palpable bump of the AC joint may reduce by asking the patients to shrug their shoulders. There is usually a 100% displacement of the clavicle relative to the acromion on radiographic evaluation (Fig. 10-3).
Type VI Injuries.
These injuries are rare injuries that are thought to result from severe trauma.23 The clavicle can become wedged beneath the acromion or coracoid. Deformity of the shoulder shows a prominent acromion, with loss of the normal rounded contour of the shoulder. Patients often have paresthesias of the affected arm. Although radiographs confirm the diagnosis, close attention to associated injuries may necessitate further imaging. Treatment is surgical reduction and stabilization. Most paresthesias will resolve with reduction of the clavicle.
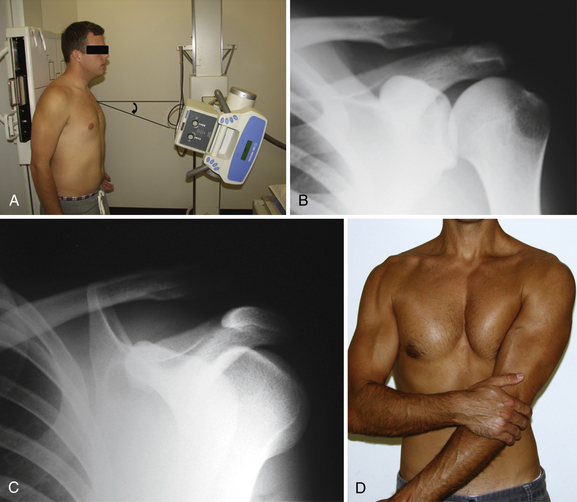
Diagnostic Imaging
The Zanca view provides the most accurate assessment of the AC joint. This view is obtained by positioning the x-ray beam for a true AP of the shoulder, with an additional 10 degrees cephalad angulation.24 This eliminates the overlap of the scapular spine usually seen on standard AP films. Because the soft tissue overlying the AC joint is minimal compared with the glenohumeral joint, the x-ray penetration should be reduced by 30% to 50%. A properly performed Zanca view helps determine superior displacement, if any, of the clavicle. Taking bilateral simultaneous Zanca views provides easy and accurate comparison with the patient’s contralateral side. For subtle injuries, types I and II, bilateral measurements of the CC distance can be calculated (Fig. 10-4).
Bearden and associates8 have shown that the normal distance between the inferior aspect of the clavicle and superior aspect of the coracoid is 1.1 to 1.3 mm. This measurement will vary with changes in distance from the x-ray beam and cassette—hence the need for side to side comparisons. A difference of over 40% is considered diagnostic for a complete CC ligament disruption. It has also been reported that an elevation of just 25% to 50% compared with the unaffected side is indicative of a complete disruption.21
TREATMENT OPTIONS
Conservative Treatment
It is generally accepted that types I (AC joint sprain) and II (AC ligament disruption with CC ligaments intact) are best managed conservatively. Treatment regimens range from sling use to immobilization to unrestricted use. For the most part, pain is managed with ice, anti-inflammatory medication, and a brief period of sling immobilization, generally for no more than 1 week. In competitive athletes, consideration of a corticosteroid or anesthetic injection directly into the AC joint may shorten the duration before return to play. The management for complete AC joint complex disruptions, types IV to VI, is surgical intervention. Significant morbidity is associated with persistently dislocated joints with extensive soft tissue disruption.10 There is no controversy with respect to the management of these significant injuries, and generally surgical reduction with reconstruction is recommended.
Grade III Acromioclavicular Joint Reconstruction
The management of type III AC separations remains controversial. Historically, pertinent literature has supported the use of nonsurgical treatment for the management of type III dislocations.26–33 Patients who fail conservative management are then considered for surgical intervention.
Phillips and coworkers conducted a meta-analysis of 1172 patients with type III injuries.34 Satisfactory outcomes were reported in 88% of operative and 87% of nonoperative cases. Moreover, there was a 59% reoperation rate in the surgical group compared with 6% in the nonoperative group. It was concluded that there was no evidence to support one method of treatment and surgery was not recommended for younger patients. More recently, Spencer35 systematically reviewed the literature regarding type III injuries. Despite acknowledging the inconclusive nature of the evidence, it was concluded that nonoperative treatment of type III AC injuries was superior to operative intervention. The results of operative treatment were not clearly better and operative management seemed to be associated with more complications, longer recovery, and more time missed from work and sport.
Schlegel and associates36,37 have presented prospective and retrospective studies showing equivalent outcomes for surgical and nonsurgical treatment of type III AC joint disruptions. Press and coworkers38 have described advantages and disadvantages of both treatments. Their operative group of 16 AC joint reconstruction patients returned to pain-free status more quickly and had better subjective impressions of pain, range of motion, functional limitations, cosmesis, and long-term satisfaction, whereas the 10 nonoperative patients returned to work and athletics faster and spent less time immobilized.
Despite the general acceptance of nonoperative treatment for initial management of type III injuries, some may conclude that a subset of throwing athletes, who place a high demand on their shoulders, would benefit from acute stabilization and repair of the AC joint. McFarland and colleagues39 surveyed 42 physicians for major league baseball teams and found that 69% would treat a hypothetical pitcher conservatively. Furthermore, of the 32 throwing athletes in the study who sustained type III AC injuries and were treated by these physicians, 80% were managed conservatively; 91% who were managed surgically achieved pain-free motion and normal function.
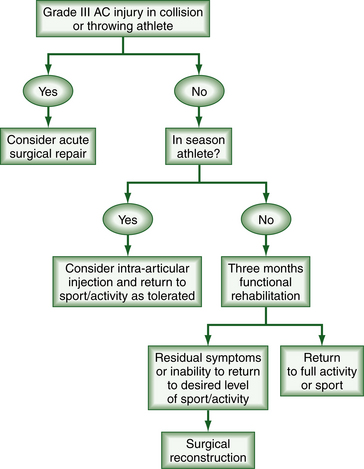
It is clear that many factors are involved when determining the most appropriate management of acute type III AC injuries. Each case must be evaluated individually, taking into consideration the sport, position, demand, risk of reinjury, and time left in the season. Because of the considerable controversy and lack of definitive evidence, it is our opinion that most type III AC separations should initially be managed conservatively with 12 weeks of nonoperative treatment. Patients who fail conservative care, defined by the persistence of symptoms or inability to return to their desired level of activity or sport, are considered potential candidates for AC joint reconstruction49 (Fig. 10-5).
Surgical Reconstruction
The literature abounds with many varieties of open and arthroscopic surgical techniques for the management of AC joint dislocations. Contemporary treatment of acute dislocations usually involves reduction and fixation with heavy suture or tape cerclage, with or without CC ligament repair; reconstruction of the CC ligaments is recommended for chronic injuries. The well-accepted Weaver-Dunn technique has been traditionally recommended. However, several studies using modern techniques have shown radiographic failures as high as 50%.12,14,40
Arthroscopic Acromioclavicular Reconstruction:
Recent reports have detailed the use of the TightRope system (Arthrex, Naples, Fla) for the anatomic reduction of the AC joint.41,42 Originally designed to maintain reduction of the ankle syndesmosis, its application to AC joint injuries was a natural extension, allowing for secure, nonrigid fixation. Consisting of four strands of no. 5 ultrastrong braided suture looped into a double-pulley system and button fixation above and below the clavicle and coracoid, respectively, this construct permits normal movement of the clavicle at the AC joint while maintaining the anatomic distance between the coracoid and clavicle.
Biomechanical testing suggests strengths that approximate native ligament strength. However, because no biologic graft is used, the construct relies on the presumption of healing of the native ligaments to afford a lasting reduction of the AC joint. Therefore, it would seem best suited for acute AC dislocations. Reconstruction techniques include single and more anatomic double TightRope constructs11,41,42 (Fig. 10-6). The approach and principles of application of the TightRope are the same as for the GraftRope described here.
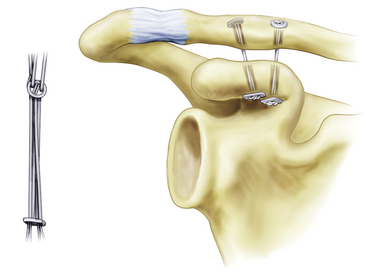
FIGURE 10-6 Double-suture pulley AC reconstruction.
(From Walz L, Salzmann GM, Fabbro T, et al. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J Sports Med. 2008; 36:2398-2406.)
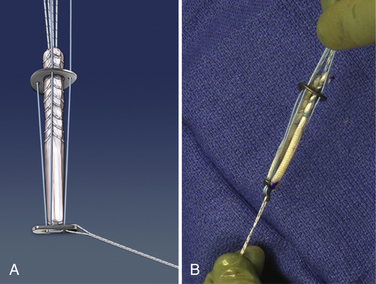
The GraftRope system, a combination of synthetic and biologic fixation, is a second-generation AC fixation device intended for use in acute and chronic AC joint separations. It uses the strength of the double-pulley system while incorporating a biologic graft that is placed through bone tunnels in the coracoid and clavicle. After adequate reduction of the AC joint, the joint is maintained by the double-pulley–button system, consisting of four strands of the ultrastrong no. 5 braided suture. The biologic graft tails are then appropriately tensioned and secured with an interference screw in the clavicle.
Graft Preparation.
The GraftRope requires the use of a biologic graft. A variety of graft options are available. Autogenous options include the semitendinosus or gracilis, which have been shown to be biomechanically equivalent to the CC ligament complex.12,13,40 Allograft options include the semitendinosus, gracilis, and tibialis anterior, and commercially presized allografts are available as well. The graft is harvested, cleaned, and cut down to approximately 12 to 15 cm in length. Each end is whip-stitched with a no. 2 ultrastrong braided suture starting 30 mm from the folded center. The folded graft must pass through a 5-mm sizing block so that the entire construct will pass easily through a 6-mm spacer. The folded graft is then secured to the coracoid button with a no. 2 ultrastrong braided suture while the whip-stitched ends are passed through the clavicle washer (Fig. 10-7).
Arthroscopic Anatomy.
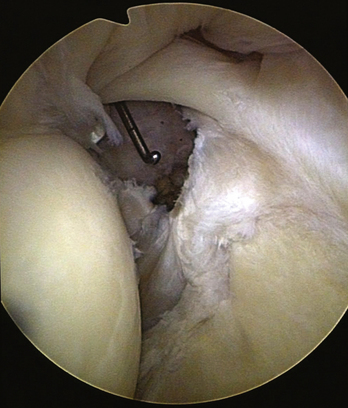
Access to the coracoid base can be achieved through the glenohumeral joint via the rotator interval or by a subacromial approach. The most direct access to the inferior medial base of the coracoid is through the rotator interval. The rotator interval is defined as the space between the superior glenohumeral ligament and subscapularis tendon. The inferior border of the coracoid can be identified by splitting the rotator interval just superior to the subscapularis. The tip of the coracoid can be visualized and palpated laterally toward the humerus, whereas the inferior medial base is exposed by its bony projection off the scapula, near the glenoid (Fig. 10-8).
Arthroscopic Technique.
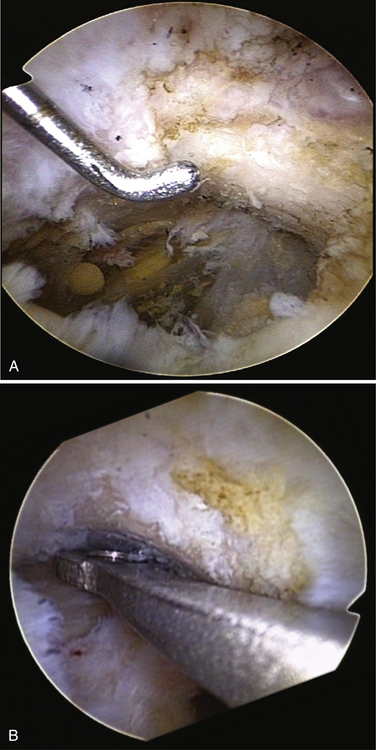
After positioning the patient and marking the osseous anatomy, a 2-cm longitudinal incision is made over the distal clavicle approximately 3.5 cm proximal to the AC joint. The deltotrapezial fascia is split longitudinally and the clavicle is exposed. The incision may be extended to perform an open distal clavicle resection based on the surgeon’s preference. It should be noted that we do not perform a distal clavicle resection on routine reconstructions and only consider it in the chronic setting. Measure approximately 35 mm from the distal end of the clavicle and place a 2.4-mm guide pin centered in the AP direction. This will locate the clavicle hole between the insertion points of the conoid and trapezoid ligaments, respectively. Overdrill the guide pin with a 6-mm cannulated reamer, creating a unicortical hole. This hole will serve as a drill guide rest by allowing the bullet-nosed drill sleeve of the guide to rest in the correct location so that the surgeon can now concentrate on placing the coracoid-aiming device below the coracoid, in the ideal anatomic location (Fig. 10-9).
Placing the guide in the correct location under the coracoid is the most critical aspect of the procedure. It is imperative to place the coracoid aiming guide as close to the base of the coracoid as possible. It should be located at the base of the coracoid at its projection off the scapula, where it is widest, in the anteroposterior direction. Having identified the correct location under the coracoid, the superior drill sleeve of the guide can now be placed in the unicortical drill rest hole in the clavicle. It should be noted that it is unnecessary at this point to have the AC joint anatomically reduced.
Superiorly, the limbs of the graft are separated and a 1.1-mm Nitinol wire is placed in the center and through both cortices of the clavicle. The free ends of the graft are tensioned, and a 5.5-mm cannulated tenodesis screw is placed. The graft ends can be cut flush or used to augment additional reconstruction of the AC ligaments (Fig. 10-10).
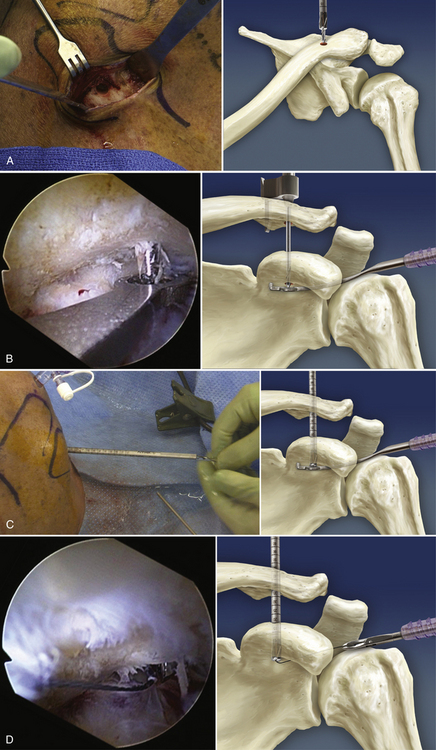
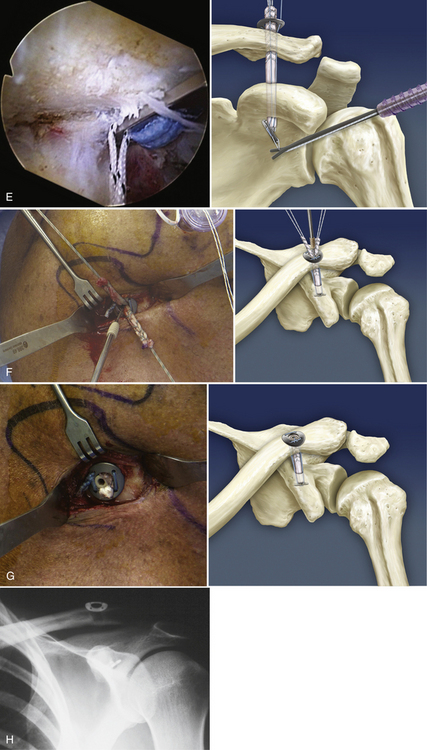
FIGURE 10-10 GraftRope surgical procedure (left shoulder)—Arthroscopic views and illustrations. A, Drill a 6-mm unicortical hole at approximately 35 mm from the lateral clavicular border. B, Advance the guide pin through the clavicle and coracoid. Confirm correct placement. C, Advance a 6-mm drill over the guidewire, creating 6-mm holes in both clavicle and coracoid. Remove the guidepin and advance a passing wire. D, Retrieve the passing wire through the anterior working portal. E, Use the passing wire to shuttle the traction suture; then pull the button and graft construct through the clavicle and coracoid. Use a forked probe to change the vector of the suture until the button passes and is postioned correctly. F, Manually reduce the clavicle and tie the no. 5 suture with alternating half-hitches. Next, place a Nitinol wire between the graft tails and advance a 5.5-mm interference screw to secure the graft. Trim the graft excess. G, Final construct. H, Postoperative x-ray image showing correct position of the buttons and reduction of the clavicle.
Biomechanical Rationale of the GraftRope.
Biomechanical data has been acquired that compared this construct favorably with the native AC joint complex. In an in vitro cadaver model, combined double-pulley with biologic grafts reconstructions were performed after sacrificing the AC and CC ligaments and compared with their matched paired, intact other side. Testing of the native AC joint revealed an ultimate load to failure of the AC joint complex to superior displacement of 664 N, which is consistent with the literature, where it has been reported between 500 and 725 N.11,43,44 Testing of the construct revealed an average ultimate load to failure of 644 N, which was statistically equivalent to the native controls. In addition, the classic Weaver-Dunn and ACCR procedures were tested and found to have an ultimate load of 354 and 364 N, respectively. Currently, the double-pulley with biologic graft configuration has one of the highest ultimate load strengths of all the different reconstructive techniques in the literature. This construct was also cyclically loaded and tested for gap formation as an indicator of potential creep. A 70-N cyclic load was applied in the anterior, posterior, and superior directions. Gap formation for this configuration was found to be statistically equivalent to the intact matched controls.
Arthroscopically Assisted Miniopen Technique: Augmented Anatomic Coraco-clavicular Reconstruction
The ACCR technique appears to provide a substantial improvement in initial stability and represents a biomechanical improvement compared with CA ligament transfer in an in vitro cadaver model. Biomechanical testing supports the importance of the CC and AC ligaments in controlling vertical and horizontal translation of the clavicle.5,9,14,17,45 Closely approximating the native anatomy may improve long-term functional outcomes.
Next, the anterior deltoid is subperiosteally reflected from the anterior clavicle, providing access to the coracoid. A passing instrument (e.g., curved clamp, Hewson suture passer) is used to place a shuttle suture around the coracoid in a medial to lateral fashion and posterior to the conjoined tendon. The previously prepared graft is then passed around the coracoid and through the corresponding clavicle hole. The AC joint is reduced anatomically and the GraftRope is tensioned and tied. Having reduced and secured the AC joint, each end of the graft is then tensioned and secured with a bicortical interference screw (Fig. 10-11).
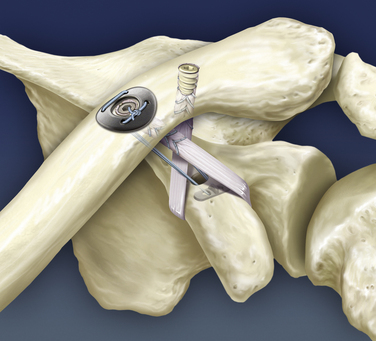
FIGURE 10-11 Anatomic coracoclavicular reconstruction augmented with a four-strand, no. 5 suture pulley system.
The ACCR technique using a free tendon graft appears to provide a substantial improvement in initial stability and represents a biomechanical improvement compared with coracoacromial ligament transfer in an in vitro cadaver model.17 Augmentation with ultrastrong synthetic suture provides additional strength to the construct, especially during the critical graft maturation phase.
An all-arthroscopic version of this technique has been developed and performed reproducibly in a cadaveric model. Although this technique is relatively new in conception, it offers the advantages of a near-anatomic reconstruction, minimal additional soft tissue damage, and theoretically increased strength by the use of a hybrid construct. Evaluation of this technique is ongoing.
PEARLS& PITFALLS
TECHNICAL PEARLS
SUMMARY
Although AC joint injuries are common, the surgical management of these injuries continues to be a challenging and, at times, vexing problem. Motion at the AC joint is extremely complex and not entirely understood. Classically, the Weaver-Dunn procedure and its modifications have been recommended. However, the procedure has had unpredictable long-term results, and the ideal reconstructive technique has not been clearly defined. This has prompted a recent renewed interest in the anatomy and biomechanics of the AC joint. The most recent generation of AC reconstructions has been developed according to sound, scientifically based anatomic and biomechanical principles. By acknowledging current data and newer biomechanical standards, it appears that the hybrid reconstructive technique of ultrastrong synthetic fixation in conjunction with a free biologic graft holds the most promise for a stable and long-lasting reconstruction. This conclusion has been supported indirectly by recent literature detailing a variety of hybrid constructs.11,46–48
The double-pulley with biologic graft procedure, indicated for acute and chronic reconstructions, provides secure hybrid fixation of the AC joint while minimizing additional trauma by using an all-arthroscopic approach. It has been shown to have biomechanically equivalent strength in controlling vertical and horizontal displacement as compared with the native ligaments. The miniopen, arthroscopically assisted technique of coupling the anatomic CC reconstruction (ACCR) with a GraftRope “skeleton” or Tightrope is another suitable option for generating an anatomically and biomechanically sound construct. Arthroscopic AC reconstruction is clearly in its nascence, and it is anticipated that as more experience is gained, arthroscopic AC reconstructive techniques will continue to evolve.
1. Petersson C Degeneration of the acromioclavicular joint: a morphological study. Acta Orthop Scand, 54; 1983:434-438.
2. DePalma A, Callery G, Bennett G. Variational anatomy and degenerative lesions of the shoulder joint. Instr Course Lect. 1949;6:255-281.
3. Salter EJ, Nasca R, Shelley B. Anatomical observations on the acromioclavicular joint and supporting ligaments. Am J Sports Med. 1987;15:199-206.
4. Rios CG, Arciero RA, Mazzocca AD. Anatomy of the clavicle and coracoid process for reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2007;35:811-817.
5. Fukuda K, Craig EV, An KN, et al. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68:434-440.
6. Harris RI, Vu DH, Sonnabend DH, et al. Anatomic variance of the coracoclavicular ligaments. J Shoulder Elbow Surg. 2001;10:585-588.
7. Salzmann GM, Paul J, Sandmann GH, et al The coracoidal insertion of the coracoclavicular ligaments: an anatomic study. Am J Sports Med, 36; 2008:2392-2397.
8. Bearden J, Hughston J, Whatley G Acromioclavicular dislocation: method of treatment. Am J Sports Med, 1; 1973:5-17.
9. Debski RE, Parsons IM, Woo SL, et al. Effect of capsular injury on acromioclavicular mechanics. J Bone Joint Surg Am. 2001;83:1344-1351.
10. Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35:316-329.
11. Walz L, Salzmann GM, Fabbro T, et al The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J Sports Med, 36; 2008:2398-2406.
12. Harris RI, Wallace AL, Harper GD, et al. Structural properties of the intact and the reconstructed coracoclavicular ligament complex. Am J Sports Med. 2000;28:103-108.
13. Motamedi AR, Blevins FT, Willis MC, et al. Biomechanics of the coracoclavicular ligament complex and augmentations used in its repair and reconstruction. Am J Sports Med. 2000;28:380-384.
14. Jari R, Costic RS, Rodosky MW, Debski RE. Biomechanical function of surgical procedures for acromioclavicular joint dislocations. Arthroscopy. 2004;20:237-245.
15. Weaver JK, Dunn HK. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. J Bone Joint Surg Am. 1972;54:1187-1194.
16. Weinstein DM, McCann PD, McIlveen SJ, et al. Surgical treatment of complete acromioclavicular dislocations. Am J Sports Med. 1995;23:324-331.
17. Mazzocca A, Santangelo S, Johnson S, et al. A Biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34:236-246.
18. Adams FL. The Genuine Works of Hippocrates. New York: William Wood; 1886. Vols 1 and 2
19. Cadenat F. The treatment of dislocations and fractures of the outerend of the clavicle. Int Clin. 1917;1:145-169.
20. Tossy J, Mead N, Sigmond H Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res, 38; 1963:111-119.
21. Rockwood CJ, Williams G, Young D. Disorders of the acromioclavicular joint. In: Rockwood CJ, Matsen FAIII, editors. The Shoulder. 2nd ed. Philadelphia: WB Saunders; 1998:483-553.
22. O’Brien SJ, Pagnani MJ, Fealy S, et al The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med, 26; 1998:610-613.
23. Gerber C, Rockwood CJ Subcoracoid dislocation of the lateral end of the clavicle: a report of three cases. J Bone Joint Surg Am, 69; 1987:924-927.
24. Zanca P Shoulder pain: involvement of the acromioclavicular joint (analysis of 1,000 cases). Am J Roentgenol Radium Ther Nucl Med, 112; 1971:493-506.
25. Trainer G, Arciero RA, Mazzocca AD. Practical management of grade III acromioclavicular separations. Clin J Sport Med. 2003;18:162-166.
26. Galpin RD, Hawkins RJ, Grainger RW. A comparative analysis of operative versus nonoperative treatment of grade III acromioclavicular separations. Clin Orthop Relat Res. 1985;193:150-155.
27. Press J, Zuckerman JD, Gallagher M, Cuomo F Treatment of grade III acromioclavicular separations: operative versus nonoperative management. Bull Hosp Jt Dis, 56; 1997:77-783.
28. Taft TN, Wilson FC, Oglesby W. Dislocation of the acromioclavicular joint. J Bone Joint Surg Am. 1987;69:1045-1051.
29. Rosenom M, Pedersen EB. A comparison between conservative and operative treatment of acute acromioclavicular dislocation. Acta Orthop Scand. 1974;45:50-59.
30. Powers JA, Bach PJ Acromioclavicular separations: closed or open treatment. Clin Orthop Related Res, 104; 1974:213-223.
31. MacDonald PB, Alexander MJ, Frejuk J, Johnson GE. Comprehensive functional analysis of shoulders following complete acromioclavicular separation. Am J Sports Med. 1988;16:475-480.
32. Calvo E, Lopez-Franco M, Arribas I. Clinical and radiologic outcomes of surgical and conservative treatment of type III acromioclavicular joint injury. J Shoulder Elbow Surg. 2006;15:300-305.
33. Nissen CW, Chatterjee A Type III acromioclavicular separation: results of a recent survey on its management. Am J Orthop, 36; 2007:89-93.
34. Phillips A, Smart C, Groom A. Acromioclavicular dislocation. Clin Orthop Relat Res. 1998;353:10-17.
35. Spencer E. Treatment of grade iii acromioclavicular joint injuries. Clin Orthop Relat Res. 2007;455:38-44.
36. Schlegel TF, Burks RT, Marcus RL, Dunn HK. A prospective evaluation of untreated acute grade III acromioclavicular separations. Am J Sports Med. 2001;29:699-703.
37. Schlegel TF, Boublik M, Hawkins RJ. Paper presented at Grade III acromioclavicular separations in NFL quarterbacks. Keystone, Colo: American Orthopaedic Society of Sports Medicine Annual Meeting; 2005 July 14-17, 2005.
38. Press J, Zuckerman JD, Gallagher M, Cuomo F Treatment of grade III acromioclavicular separations: operative versus nonoperative management. Bull Hosp Jt Dis, 56; 1997:77-83.
39. McFarland EG, Bilvin SJ, Doehring CB, et al Treatment of grade III acromioclavicular separations in professional throwing athletes: results of a survey. Am J Orthop, 16; 1997:771-774.
40. Lee SJ, Nicholas SJ, Akizuki KH, et al Reconstruction of the coracoclavicular ligaments with tendon grafts: a comparative biomechanical study. Am J Sports Med, 31; 2003:648-654.
41. Richards A, Tennent TD. Arthroscopic stabilization of acute acromioclavicular joint dislocation using the tightrope system. Tech Shoulder Elbow Surg. 2008;9:51-54.
42. Lim YW, Sood A, van Riet RP, et al. Acromioclavicular joint reduction, repair and reconstruction using metallic buttons—early results and complications. Tech Shoulder Elbow Surg. 2007;8:213-221.
43. Grutter PW, Petersen SA Anatomical coracoclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med, 33; 2005:1723-1728.
44. Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coraco-clavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32:1929-1936.
45. Klimkiewicz JJ, Williams GR, Sher JS, et al The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg, 8; 1999:119-124.
46. Pennington WT, Hergan DJ, Bartz BA. Arthroscopic coracoclavicular ligament reconstruction using biologic and suture fixation. Arthroscopy. 2007;23:785.
47. Scheibel M, Ifesanya A, Pauly S, Haas NP. Arthroscopically assisted coracoclavicular ligament reconstruction for chronic acromioclavicular joint instability. Arch Orthop Trauma Surg. 2008;128:1327-1333.
48. Hosseini H, Friedmann S, Tröger M, et al Arthroscopic reconstruction of chronic AC joint dislocations by transposition of the coracoacromial ligament augmented by the Tight Rope device: a technical note. Knee Surg Sports Traumatol Arthrosc, 17; 2009:92-97.
49. Trainer G, Arciero RA, Mazzocca AugD. Practical management of grade III acromioclavicular separations. Clin J Sports Med. 2008;18:162-166.