1. Sonomura, T, et al. N-butyl cyanoacrylate embolization with blood flow control of an arterioportal shunt that developed after radiofrequency ablation of hepatocellular carcinoma. Korean J Radiol. 2014; 15(2):250–253.
2. Kim, TK, et al. Hepatocellular nodules in liver cirrhosis: contrast-enhanced ultrasound. Abdom Imaging. 2011; 36(3):244–263.
3. Nakamura, Y, et al. Clinical significance of the transitional phase at gadoxetate disodium-enhanced hepatic MRI for the diagnosis of hepatocellular carcinoma: preliminary results. J Comput Assist Tomogr. 2011; 35(6):723–727.
4. Vogl, TJ, et al. Portal vein thrombosis and arterioportal shunts: effects on tumor response after chemoembolization of hepatocellular carcinoma. World J Gastroenterol. 2011; 17(10):1267–1275.
5. Ahn, JH, et al. Nontumorous arterioportal shunts in the liver: CT and MRI findings considering mechanisms and fate. Eur Radiol. 2010; 20(2):385–394.
6. Mita, K, et al. Diagnostic sensitivity of imaging modalities for hepatocellular carcinoma smaller than 2 cm. World J Gastroenterol. 2010; 16(33):4187–4192.
7. Yoo, HJ, et al. Hepatocellular carcinoma in cirrhotic liver: double-contrast-enhanced, high-resolution 3.0T-MR imaging with pathologic correlation. Invest Radiol. 2008; 43(7):538–546.
8. Goto, T, et al. Osler-Weber-Rendu disease with esophageal varices and hepatic nodular change. Intern Med. 2007; 46(12):849–854.
9. Kitade, M, et al. Intrahepatic cholangiocarcinoma associated with central calcification and arterio-portal shunt. Intern Med. 2005; 44(8):825–828.
10. Sakata, H, et al. Prognostic factors for hepatocellular carcinoma presenting with macroscopic portal vein tumor thrombus. Hepatogastroenterology. 2004; 51(60):1575–1580.
11. Yoshimitsu, K, et al. Pitfalls in the imaging diagnosis of hepatocellular nodules in the cirrhotic and noncirrhotic liver. Intervirology. 2004; 47(3–5):238–251.
12. Yoshimitsu, K, et al, Unusual hemodynamics and pseudolesions of the noncirrhotic liver at CT. Radiographics. 2001;(21 Spec No):S81–S96.
13. Koizumi, J, et al. Computed tomography during arterial portography under temporary balloon occlusion of the hepatic artery: evaluation of pseudolesions caused by arterio-portal venous shunts. Abdom Imaging. 2000; 25(6):583–586.
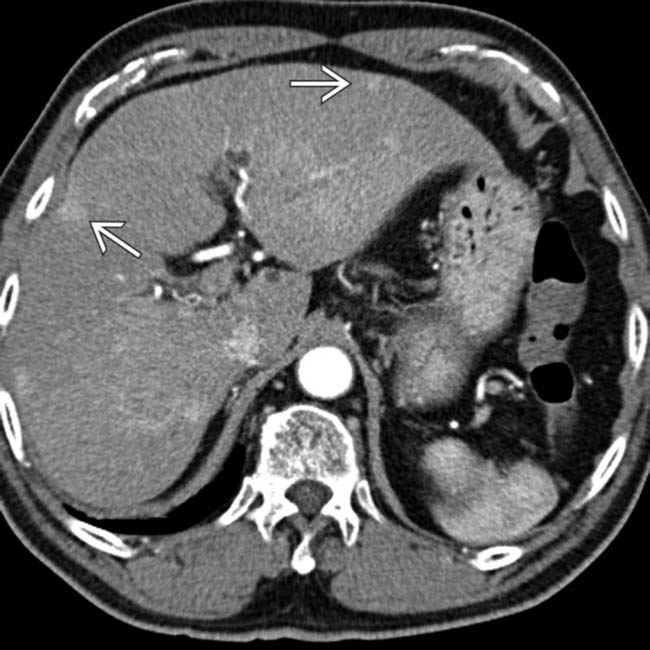
 in this 60-year-old man with cirrhosis due to chronic viral hepatitis.
in this 60-year-old man with cirrhosis due to chronic viral hepatitis.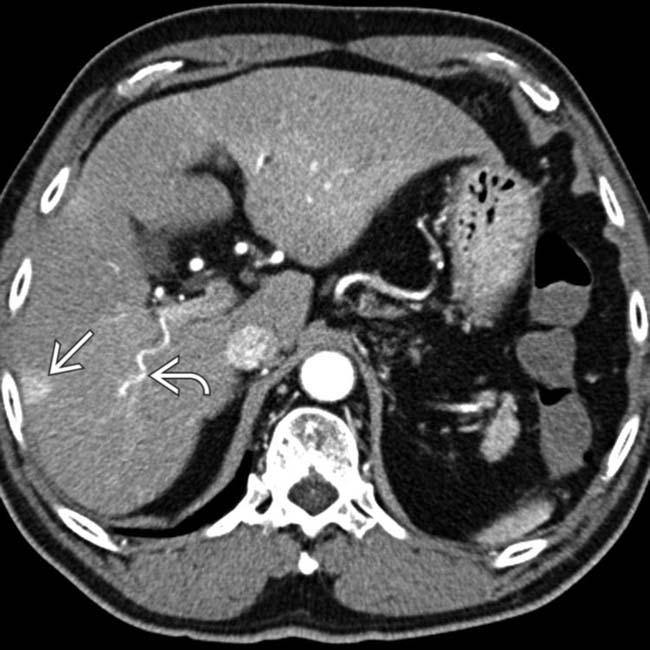
 . Also note the large, “corkscrew” hepatic arterial branch
. Also note the large, “corkscrew” hepatic arterial branch  , a typical feature of cirrhosis. The liver has a cirrhotic morphology with wide fissures.
, a typical feature of cirrhosis. The liver has a cirrhotic morphology with wide fissures.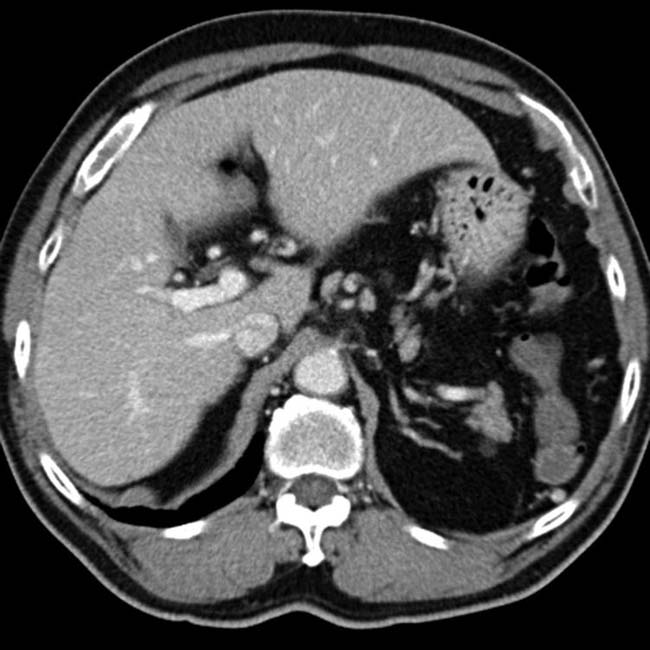


 .
.
 and early enhancement of the portal vein branch that drains this segment
and early enhancement of the portal vein branch that drains this segment  , representing an arterioportal shunt, probably due to the prior liver biopsy at this site.
, representing an arterioportal shunt, probably due to the prior liver biopsy at this site.
 but otherwise appears normal.
but otherwise appears normal.




































































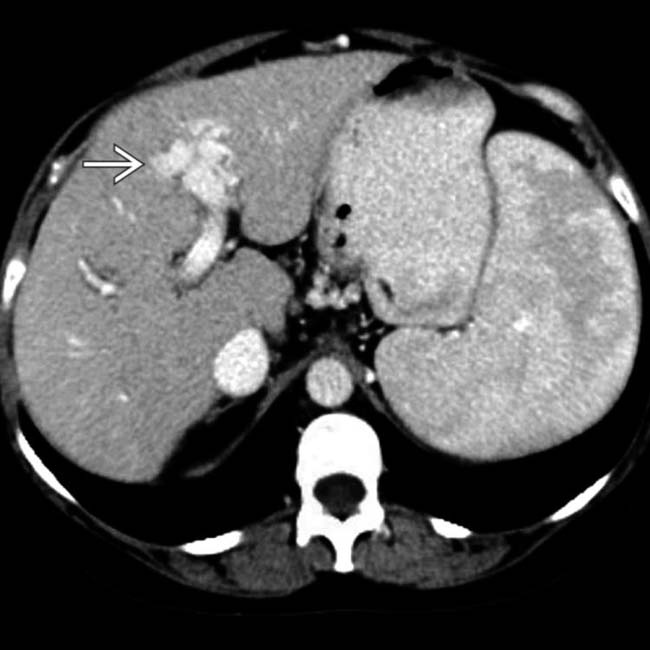
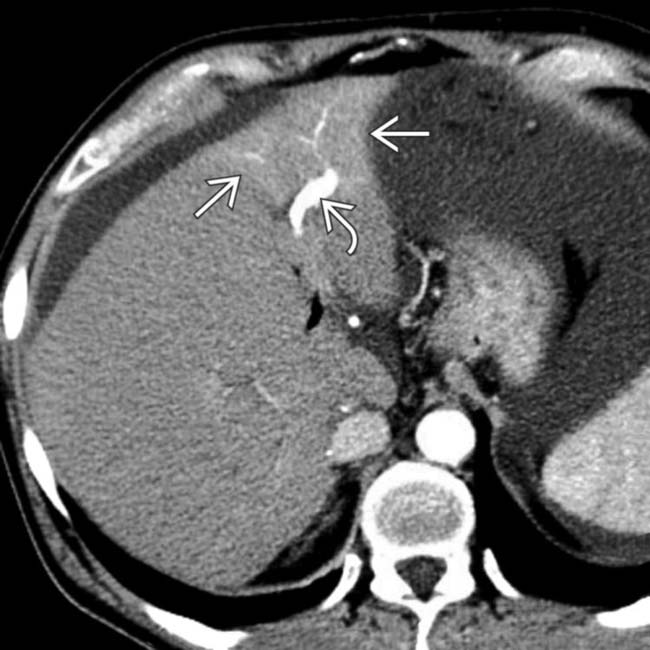
 in the left lobe, most likely the result of a prior liver biopsy at this site.
in the left lobe, most likely the result of a prior liver biopsy at this site.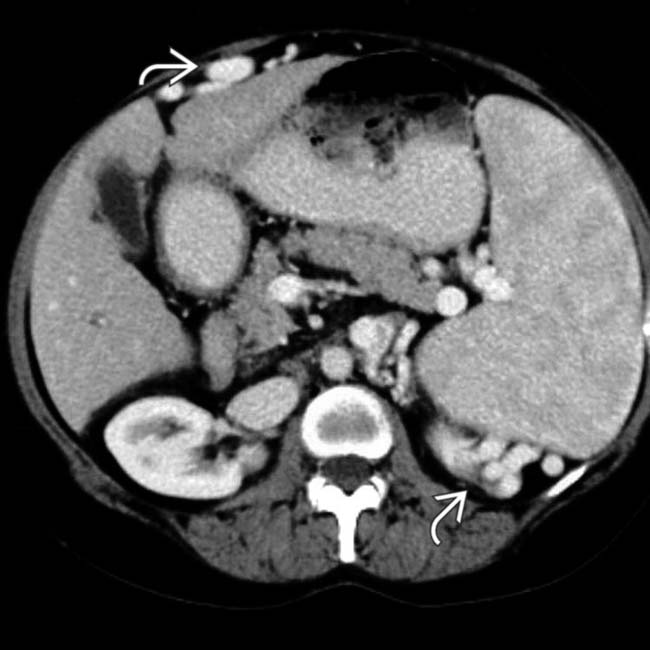
 .
.
