Arterial Line Anatomy
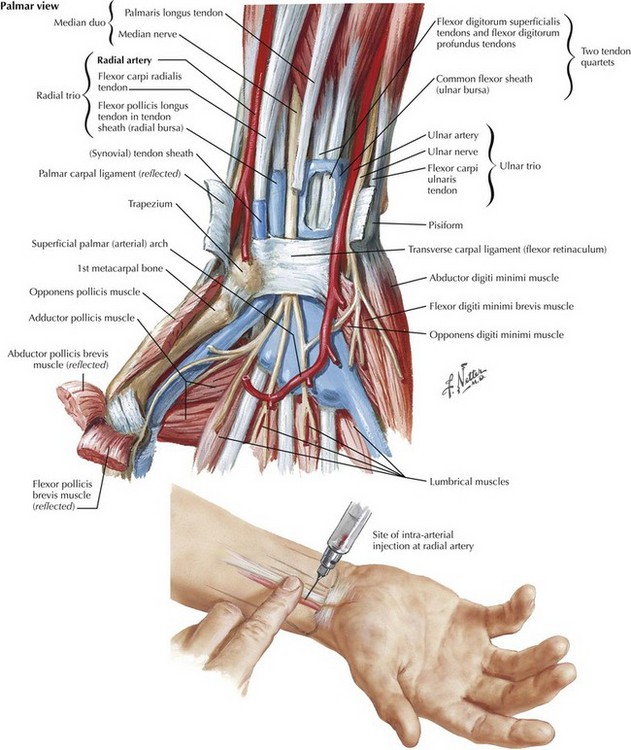
Radial Artery
The radial artery is chosen most frequently for arterial cannulation because it is readily accessible, relatively easy to cannulate, easily tested for collateral circulation, and associated with few long-term complications (Fig. 41-1). The radial artery is palpated between the distal radius and the flexor carpi radialis tendon. In this area the radial artery is covered by skin, subcutaneous tissue, and fascia only.
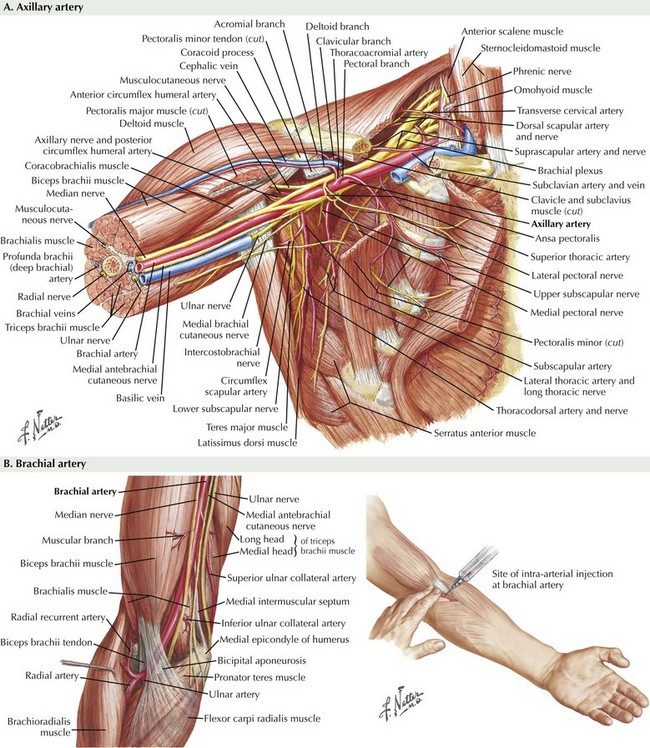
Axillary Artery
The axillary artery can be palpated in the axilla with the patient’s arm elevated over the head (Fig. 41-2, A). The axillary artery lies lateral to the axillary vein throughout its course, and it is divided into three parts on the basis of its relationship to the pectoralis minor muscle. The third or most distal segment is located lateral to the pectoralis minor muscle and is available for cannulation. The close relationship between the brachial plexus and the axillary artery should be recognized because of the risk of nerve injury with axillary artery cannulation.
Brachial Artery
At the lower border of the teres major muscle, the axillary artery becomes the brachial artery (Fig. 41-2, B). It then traverses the flexor compartment of the arm, eventually bifurcating into the radial and ulnar arteries. The brachial artery is superficial throughout its course, covered only by skin, subcutaneous tissue, and fascia, and is palpable between the biceps and triceps muscles proximal to the antecubital fossa. The brachial artery gives off numerous muscular branches and a nutrient artery to the humerus. Some of these vessels take part in the arterial anastomosis at the elbow joint. The largest branch is the profunda brachii artery. The brachial artery is accompanied by a pair of brachial veins. Although limb ischemia is a feared complication of brachial arterial lines, little evidence supports this concern.
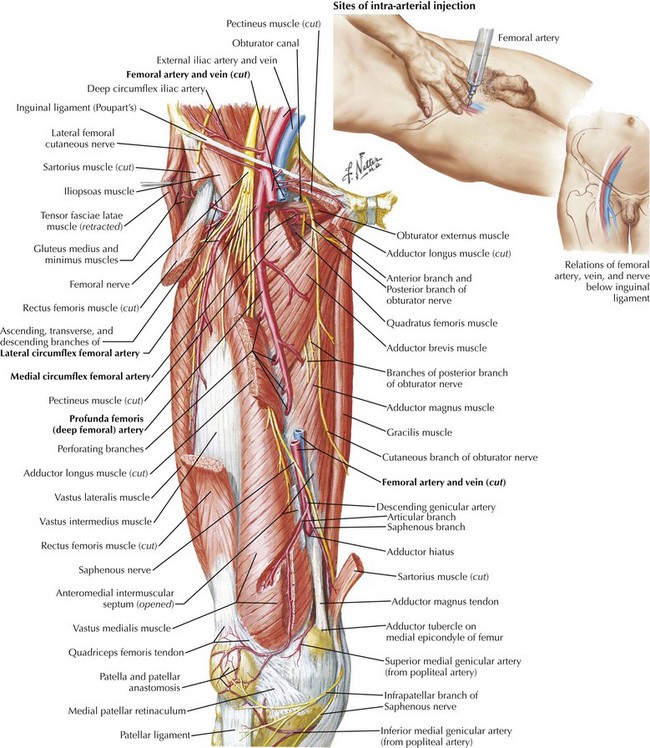
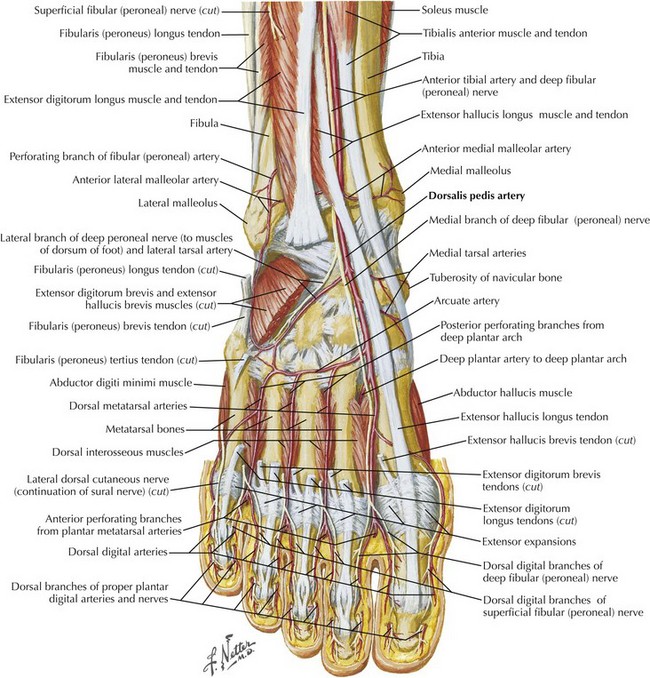
Femoral and Dorsalis Pedis Arteries
The femoral artery is a continuation of the external iliac artery below the inguinal ligament (Fig. 41-3). It is palpable at this level at the midinguinal point, that is, halfway between the anterior superior iliac spine and the pubic symphysis. The artery courses lateral to the femoral vein and medial to the femoral nerve.
As it enters the foot, the anterior tibial artery becomes the dorsalis pedis artery (Fig. 41-4). It runs superficial to other structures over the dorsum of the foot until it passes through the first intermetatarsal space to anastomose with the plantar arch on the sole of the foot. The dorsalis pedis artery is palpable over the dorsum of the foot between the first and second metatarsal bones.
Gordon, LH, Brown, M, Brown, OW, Brown, EM. Alternative sites for continuous arterial monitoring. South Med J. 1984;77:1498–1500.
Hall-Craggs, ECB. Anatomy as a basis for clinical medicine, 2nd ed. New York: Urban & Schwarzenberg; 1990.
Okeson, GC, Wulbrecht, PH. The safety of brachial artery puncture for arterial blood sampling. Chest. 1998;114:748–751.
Slogoff, S, Keats, AS, Arlund, C. On the safety of radial artery cannulation. Anesthesiology. 1983;59:42–47.
Tegtmeyer, K, Brady, G, Lai, S, Hodo, R, Braner, D, Videos in clinical medicine: placement of an arterial line. N Engl J Med 2006;354:e13. http://www.nejm.org/doi/full/10.1056/NEJMvcm071974#figure=preview.gif.