5 Aortic stenosis
Salient features
History
• Asymptomatic (many patients do not have symptoms)
• Angina (in ~70% of adults; average survival after onset of angina is 5 years)
• Syncope (in 25% of patients, during or immediately after exercise; average survival after onset of syncope is 3 years)
• Dyspnoea: common presenting symptom (suggests left ventricular dysfunction; heart failure reduces life expectancy to <2 years).
Examination
Pulse
• Low volume pulse, with a delayed upstroke (pulsus parvus et tardus). This is caused by a reduction in systolic pressure and a gradual decline in diastolic pressure.
• Normal pulse in mild aortic stenosis when the gradient is <50 mmHg.
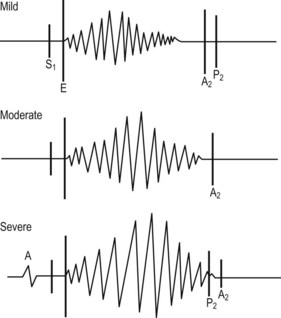
• Slow rise with diminished ‘volume’, sometimes with notch on the upstroke (‘anacrotic’): indicating severe aortic stenosis with associated aortic regurgitation, double pulse may be felt (‘bisferious’) (Fig. 5.1).
Heart
• Apex beat is heaving in nature but is not displaced. (A displaced apex beat indicates left ventricular dilatation and severe disease.)
• Palpable systolic vibrations over the primary aortic area, with the patient in the sitting position during full expiration (often correlates with a gradient of >40 mmHg)
• Systolic thrill over the aortic area and the carotids
• Ejection click heard 0.1 s after first heart sound, along the left sternal border (indicates valvular stenosis). An ejection sound that moves with respiration is not aortic in origin (Fig. 5.2)
• An atrial (S4) sound may be heard
• Ejection systolic murmur at the base of the heart conducted to the carotids and the right clavicle (Fig. 5.2). (Listen carefully for an early diastolic murmur as mild aortic regurgitation often accompanies aortic stenosis.) Remember Valsalva decreases duration of murmur of aortic stenosis and increases the murmur of hypertrophic cardiomyopathy
• Third heart sound: in patients with aortic stenosis, third heart sounds are uncommon but usually indicate the presence of systolic dysfunction and raised filling pressures.
Questions
What does the second heart sound tell us in this condition?
• A soft second heart sound indicates valvular stenosis (except in calcific stenosis of the elderly, where the margins of the leaflets usually maintain their mobility).
• A single second heart sound may be seen when there is fibrosis and fusion of the valve leaflets.
• Reversed splitting of the second sound indicates mechanical or electrical prolongation of ventricular systole.
• A perfectly normal second heart sound (i.e. normal splitting with A2 of normal intensity) is strong evidence against the presence of critical aortic stenosis.
Advanced-level questions
What is the mechanism of syncope in aortic stenosis?
• The LV is suddenly unable to contract (transient electromechanical dissociation) against the stenosed valve
• Cardiac arrhythmias (bradycardia, ventricular tachycardia or fibrillation)
• Marked peripheral vasodilatation without a concomitant increase in cardiac output, particularly after exercise.
What investigations would you do?
• ECG usually shows left ventricular hypertrophy, ST–T changes, possibly left axis deviation, later left atrial hypertrophy (negative P waves in V1), conduction abnormalities from calcification of conducting tissues (first-degree heart block, left bundle branch block).
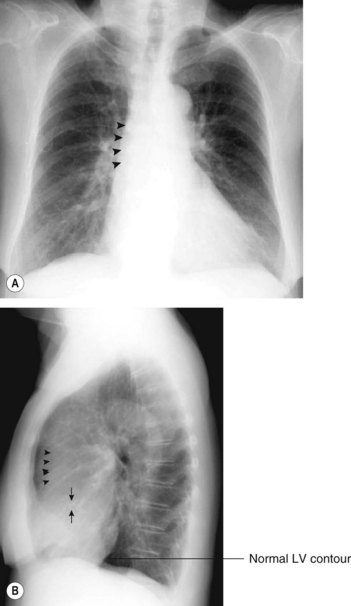
• Chest radiograph may show cardiac enlargement, post-stenotic dilatation of aorta (a bicuspid valve should be suspected if the proximal aorta is greatly enlarged), calcification of aortic valve (particularly in older patients) (Fig. 5.3).
• Echocardiography is useful in:
• Exercise testing in adults with aortic stenosis has been discouraged largely because of safety; it should not be performed in symptomatic patients as it may be fatal; in asymptomatic patients an abnormal haemodynamic response (e.g. hypotension) is sufficient to consider aortic valve replacement. In selected patients it may be useful to provide a basis for advice about physical activity.
• Cardiac catheterization is done to assess the coronary circulation and to confirm or clarify the diagnosis. When the echocardiogram is inadequate, cardiac haemodynamics using both left- and right-heart catheterization is indicated and requires:
What are the complications of aortic stenosis?
• Left ventricular failure indicates poor prognosis unless the valve is replaced.
• Sudden death occurs in 10–20% of adults and 1% of children. It has been rarely documented to occur without prior symptoms. It is an uncommon event: probably <1% per year.
• Arrhythmias and conduction abnormalities include ventricular arrhythmias (more common than supraventricular arrhythmias) and heart block (may occur because of calcification of conducting tissues).
• Systemic embolization is caused by disintegration of the aortic valve apparatus or by concomitant aortic atheroma.
• Infective endocarditis (in 10% of cases) should be considered when these patients present with unexplained illness.
How would you manage this patient?
• If the patient is asymptomatic and the valvular gradient is <50 mmHg, then observation. Surgery is not recommended in asymptomatic patients.
• Valve replacement in the following circumstances:
• Often, patients require coronary artery bypass grafts during aortic valve replacement.
• Balloon valvuloplasty should be limited to moribund patients requiring emergency intervention or those with a very poor life expectancy from other pathology. In one study, although in-hospital mortality rates were similar to those following conventional surgical replacement, there were more deaths in the valvuloplasty group in the subsequent follow-up period (J Am Coll Cardiol 1992;20:796–801).