CHAPTER 10 Ankle Fractures
Ankle fractures are common, and although joint stability can be regained by adequate reduction and internal fixation of the fracture, some patients have disabling, persistent pain even after joint congruity is completely restored.1,2 Persistent pain may be associated with exercise or change in the weather, and there may be radiographic evidence of osteoarthritic changes. These features suggest that an articular cartilage lesion or another radiographically nondetectable lesion might have occurred at the time of injury and may be the cause of the pain.
Ankle injuries result from abnormal motion of the talus within the ankle mortise. Fractures of the malleoli can result from impact of the talus on the malleoli caused by rotational or translational forces. Fractures can also occur in tension, and the malleoli can be avulsed because of pull exerted by the intact collateral ligaments to the talus.3,4
Hintermann and coworkers prospectively evaluated the arthroscopic findings in 288 consecutive patients with acute ankle fracture (148 male and 140 female patients; mean age, 45.6 years).5 They found that, independent of fracture type, cartilage lesions were most frequently present on the talus and to a lesser extent on the tibia, fibula, and medial malleolus. The frequency and severity of cartilage lesions increased from type B to type C fractures, and there was an increase observed from subgroup 1 to subgroup 3 in both type B and type C fractures. These findings support the belief that the severity of injury directly depends on the height of the fibula fracture. The fact that there was an unexpectedly high incidence of cartilage lesions in all fracture types may explain the observation from daily practice that the final results do not always correlate with the reduction and stability achieved. It seems that the fate of the fractured ankle (i.e., prognosis) may be determined to a significant extent during the accident itself, when the cartilage and other intra-articular and periarticular structures are injured.
Cartilage lesions apparently occur when the talus is rotated or translated in the loaded ankle mortise until the fracture occurs. This is especially true for type C fractures, and it is true to a lesser extent for type B fractures as long as the underlying mechanism is a pronation or rotation movement. Supination trauma, as typically seen in type A fractures, may critically stress the medial half of the joint, but the load forces may not be as high as in pronation or rotation trauma. Taga and colleaues6 found cartilage lesions in the medial joint in 89% of 9 patients evaluated after an acute ankle sprain and in 95% of 22 patients with chronic ankle sprain. They found more cartilage lesions on the distal tibia than on the medial talus. They concluded that these injuries were mainly caused by local stress concentration. They found no correlation between the severity of the cartilage lesion and the degree of instability. This may support the belief that cartilage lesions occur to a significant extent at the time of the acute injury.
A higher incidence of cartilage lesions occurs in female patients than in male patients, and this can be explained by several factors. First, the cartilage may be less resistant to mechanical stress in females.1 Second, the cartilage may have become more vulnerable with increasing age (because the age of the female patients was significantly higher).5 Third, overall muscular and bony strength are lower in females, so that fracture probably occurs during an earlier phase of the injury, and with a higher incidence, exposing the articular surfaces to a higher risk of possible damage. This may be especially true for elderly patients.
Arthroscopy performed directly after ankle fracture can be used to visualize intra-articular lesions that cannot be detected on plain radiographs.5,7 Cartilage lesions were found in 79.2% to 90.0% of patients examined arthroscopically.5,8 The ligaments could not be identified by arthroscopy in all cases, and there were significant differences among the four ligaments; overall, more injuries to the ligaments were found than expected.5 Although its role has not been established in the acute treatment of ankle fractures,9 arthroscopy has proved to be valuable for providing detailed knowledge of the fractured ankle.5,10 It has also been helpful in the treatment of symptomatic osteophytes after ankle fracture.2
MANAGEMENT
Indications and Contraindications
Conservative or Operative Management
It is generally accepted that ORIF is the best treatment for unstable or dislocated ankle fractures.11–15 Few investigators suggest that perfect reduction is required to achieve good long-term results. Bauer and associates studied 143 patients 30 years after they sustained an ankle fracture that was treated by closed methods and found that 82% were free of arthritis and 83% were free of symptoms.11 In contrast, in a series by Beris and colleagues of 23 patients who had an ankle fracture with poor reduction, 78.3% developed osteoarthritis.16 Accordingly, I limit nonoperative treatment to older or polymorbid patients with ankle fractures without dislocation.
Arthroscopic Technique
The patient is placed supine on the operating table. The knee is flexed to about 90 degrees using a knee holder; this allows the leg to assume a hanging position with the foot and ankle touching the table (Fig. 10-1). No ankle distraction device is used. To avoid iatrogenic lesions of the articular cartilage and soft tissue, the joint is first inflated with saline, and portals are created by blunt dissection. A 4.5-mm, 30-degree arthroscope is introduced into the ankle joint through a standard central anterior portal (Fig. 10-2). The liquid is evacuated, and the cavity is filled with saline. If necessary, accessory anteromedial or anterolateral portals, or both, are also used for insertion of instruments. Systematic arthroscopic examination, as described by Ferkel and Orwin,1 is performed to visualize the internal structures.
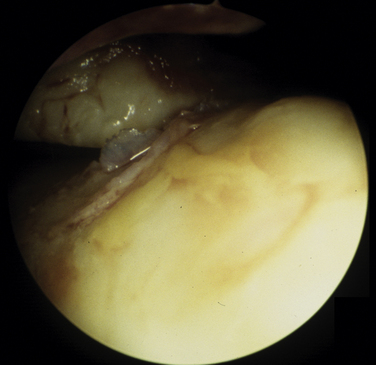
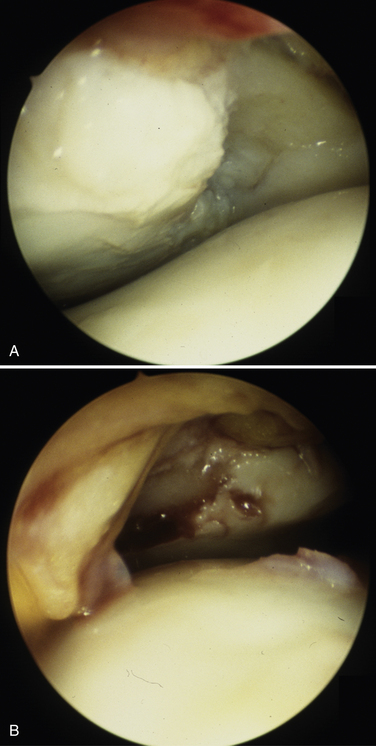
 Grade 2: fissuring or degeneration of less than one half of the thickness of the articular cartilage (Fig. 10-3)
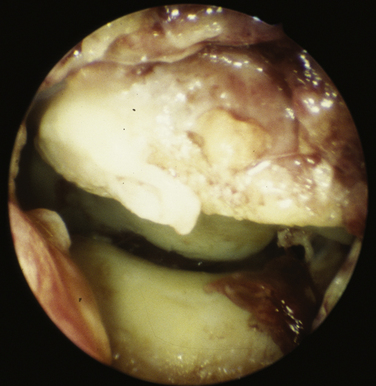
Grade 2: fissuring or degeneration of less than one half of the thickness of the articular cartilage (Fig. 10-3) Grade 3: fasciculation or degeneration of greater than one half of the thickness of the articular cartilage (Fig. 10-4)
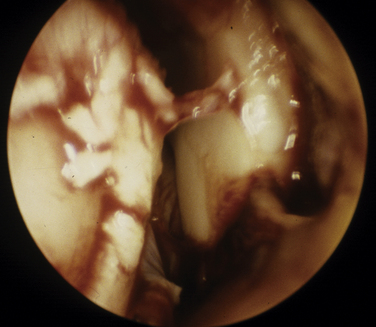
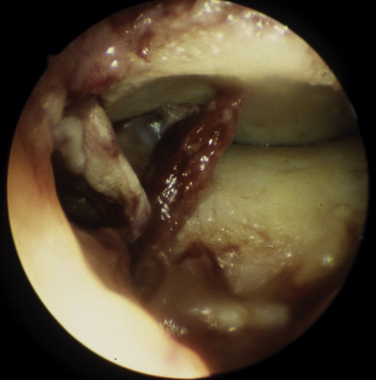
Grade 3: fasciculation or degeneration of greater than one half of the thickness of the articular cartilage (Fig. 10-4)The anterior talofibular ligament (Fig. 10-6), calcaneofibular ligament, deltoid ligament (Fig. 10-7), and anterior (Fig. 10-8) and posterior (Fig. 10-9) tibiofibular ligaments (syndesmosis) are assessed by inspection and probing. Ligament injuries are graded according to the severity of the fiber tear and the degree of instability present: A partial lesion involves a tear of less than one half of the ligament without complete instability, whereas a complete lesion implies a tear of the complete ligament or bony avulsion of the ligament with instability.
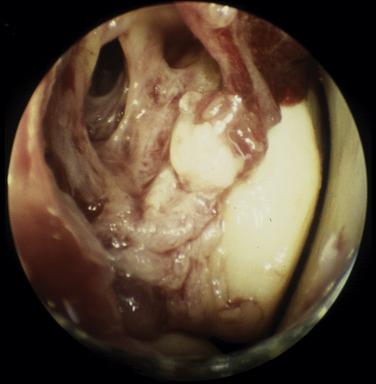
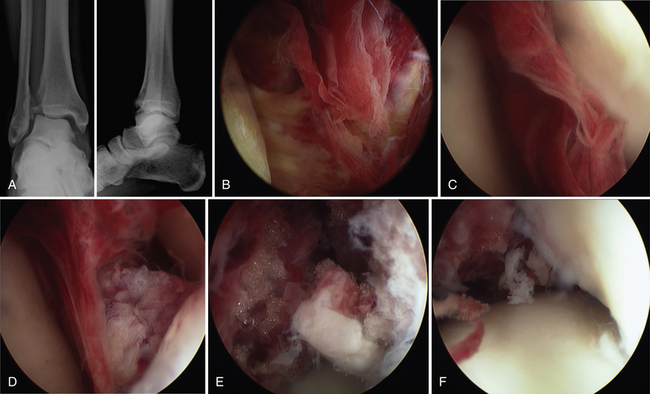
FIGURE 10-6 Avulsion of the anterior talofibular ligament together with the periosteum of external aspect of the fibula.
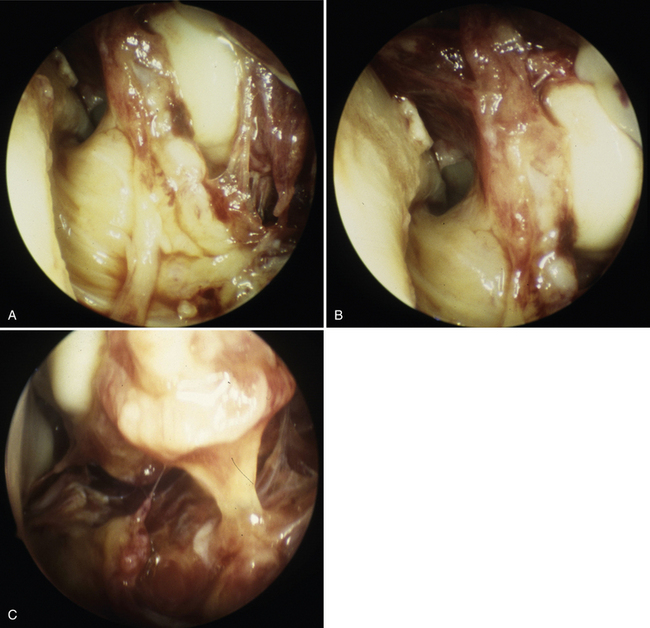
FIGURE 10-7 Deltoid ligament injury. A, There is complete rupture of anterior superficial bundles, but the deep tibiotalar bundles are intact. B, Interposition of ruptured anterior deltoid ligament between the medial malleolus and the talus. The medial joint space is markedly widened. C, Avulsion of the whole deltoid ligament from the medial malleolus.
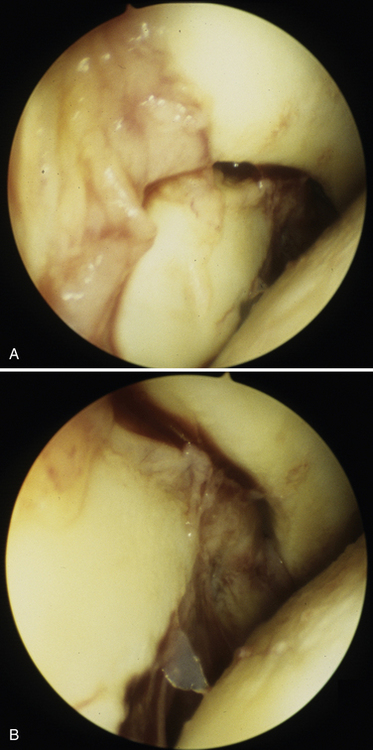
FIGURE 10-9 Rupture of the posterior tibiotalar ligament (syndesmosis). A, The fibula is subluxated in the anterior direction. B, Closer inspection shows the rupture of the posterior syndesmotic ligament.
Arthroscopy is also used to visualize the fracture pattern (Fig. 10-10) and to detect unexpected injuries to articular surfaces, such as impression (Fig. 10-11).
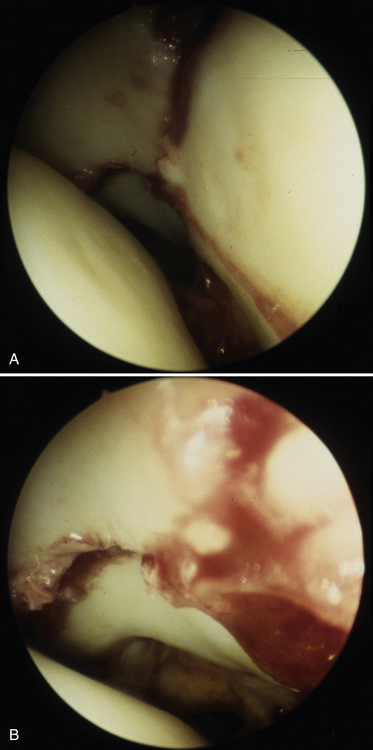
FIGURE 10-10 Fractures of tibial plafond. A, A third fragment is seen posteriorly between the fracture of medial malleolus and the tibial plafond. B, A posterior tibial fragment (i.e., Volkman fragment) is minimally displaced.
Figure 10-12 shows a case in which arthroscopy was beneficial for understanding of the injury pattern, removal of a loose fragment, and reduction of the deltoid ligament that was interposed between the medial malleolus and the talus.
PEARLS& PITFALLS
Postoperative Rehabilitation Protocol
The postoperative rehabilitation is dictated by the type of fracture and the degree of stability achieved with ORIF. If the arthroscopic evaluation has detected damages to the articular cartilage, non–weight bearing may be advised up to 6 to 8 weeks after ORIF. In the case of detected injuries to the ligamentous structures, external stabilization may be advised.
CONCLUSIONS
It appears that, even in ankle fractures that require conventional ORIF, arthroscopy may be useful to rule out occult intra-articular pathology. The added time and morbidity is minimal, and the procedure can be done with only manual distraction. Arthroscopy aids in the evaluation and treatment of chondral and osteochondral pathology as well as ligamentous injuries. It enables the surgeon to minimize the open approach and secondary damages to the surrounding tissues while performing ORIF. It is suspected, although not yet proved, that the postoperative range of motion improves more quickly after lavage and débridement of an acute ankle fracture.
1. Ferkel RD, Orwin JF. Arthroscopic treatment of acute ankle fractures and postfracture defect. In: Ferkel RD, editor. Arthroscopic Surgery. New York, NY: Lippincott-Raven; 1996:185-200.
2. Van Dijk CN, Tol JL, Verheyen CC. A prospective study of prognostic factors concerning the outcome of arthroscopic surgery for anterior ankle impingement. Am J Sports Med. 1997;25:737-745.
3. Geissler WB, Tsao AK, Hughes JL. Fractures of the ankle. In: Rockwood C, Green DP, Bucholz RW, Heckman JD, editors. Fractures in Adults. New York, NY: Lippincott-Raven; 1996:2201-2266.
4. Tile M. Fractures of the ankle. In: Schatzker J, Tile M, editors. The Rationale of Operative Fracture Care. New York, NY: Springer; 1996:523-561.
5. Hintermann B, Regazzoni P, Lampert C, et al. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br. 2000;82:345-351.
6. Taga I, ShinoK, Inoue M, et al. Articular cartilage lesions in ankles with lateral ligament injury. an arthroscopic study, Am J Sports Med. 211993 120-127.
7. Yoshimura I, Naito M, Kanazawa K, et al. Arthroscopic findings in Maisonneuve fractures. J Orthop Sci. 2008;13:3-6.
8. Thomas B, Yeo JM, Slater GL. Chronic pain after ankle fracture. an arthroscopic assessment case series, Foot Ankle Int. 262005 1012-1016.
9. Thordarson DB, Bains R, Shepherd LE. The role of ankle arthroscopy on the surgical management of ankle fractures. Foot Ankle Int. 2001;22:123-125.
10. Loren GJ, Ferkel RD. Arthroscopic assessment of occult intra-articular injury in acute ankle fractures. Arthroscopy. 2002;18:412-421.
11. Bauer M, Bergstrom B, Hemborg A, et al. Malleolar fractures. nonoperative versus operative treatmenta controlled study, Clin Orthop Relat Res. 1991985 17-27.
12. Yde J, Kristensen KD. Ankle fractures. Supination-eversion fractures stage II. primary and late results of operative and non-operative treatment, Acta Orthop Scand. 511980 695-702.
13. Phillips WA, Schwartz HS, Keller CS, et al. A prospective, randomized study of the management of severe ankle fractures. J Bone Joint Surg Am. 1985;67:67-78.
14. Makwana NK, Bhowal B, Harper WM, Hui AW. Conservative versus operative treatment for displaced ankle fractures in patients over 55 years of age. a prospective, randomised study, J Bone Joint Surg Br. 832001 525-529.
15. Rammelt S, Grass R, Zwipp H. Ankle fractures. Unfallchirurg. 2008;111:421-437.
16. Beris AE, Kabbani KT, Xenakis TA, et al. Surgical treatment of malleolar fractures. a review of 144 patients, Clin Orthop Relat Res. 3411997 90-98.