CHAPTER 31 Ankle block
Clinical anatomy
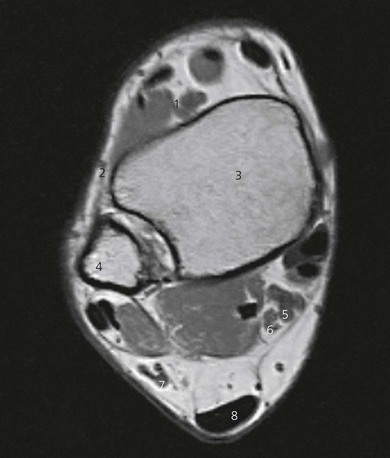
The tibial nerve runs deep to the flexor retinaculum and posterior to the posterior tibial vein and artery, between the Achilles’ tendon and medial malleolus (Figs 31.1 and 31.2). It divides into medial and lateral plantar nerves providing sensory innervation to the medial side of the sole of the foot and heel. The tibial nerve provides motor supply to the intrinsic muscles of the foot. It is the largest nerve at the ankle, requiring the longest block onset, and thus should be blocked first.
The superficial peroneal nerve travels distally with the peroneus brevis muscle, becoming superficial above the lateral malleolus, and runs over the dorsum of the foot, to which it provides sensory innervation (Figs 31.2 and 31.3).
The sural nerve runs superficially with the small saphenous vein and lies subcutaneously between the lateral malleolus and Achilles, tendon (Figs 31.2 and 31.4). It provides sensory innervation to the lateral aspect of the ankle and foot.
Surface anatomy
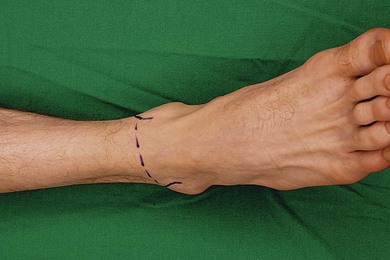
Important bony structures for the ankle block include the medial and lateral malleoli and the calcaneum. Other landmarks include the Achilles’ tendon, and on the ventral aspect of the ankle, the anterior tibial artery pulse and extensor hallucis longus tendon (Fig. 31.5). These tendons can be accentuated if the patient dorsiflexes the foot against resistance. A single needle insertion site at the midpoint of the intermalleolar line on the ventral aspect of the ankle is used for block of the superficial and deep peroneal nerves and saphenous nerve. Needle insertion for sural and tibial block is adjacent to the Achilles tendon, at the level of the superior aspect of the medial and lateral malleoli, respectively.
Sonoanatomy
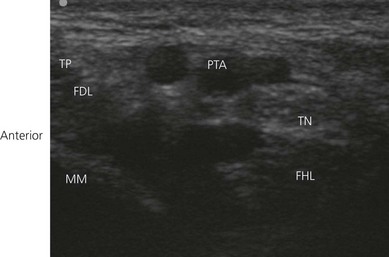
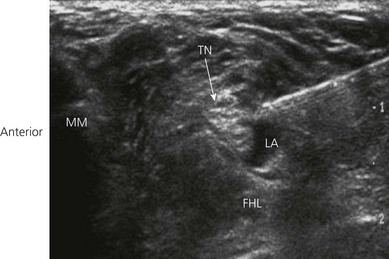
Tibial nerve
Position the patient supine and bolster the foot with a pillow to expose the anterior and medial portion of the lower leg and foot. The lower limb is externally rotated. Place a 10–15 MHz transducer immediately above the medial malleolus to locate the tibial nerve in the transverse (short axis) view (Fig. 31.6). Perform a systematic anatomical survey in the medial aspect of the ankle. The bony medial malleolus is easily identified (bony shadow). Move the transducer slightly posteriorly to identify the tibialis posterior and flexor digitorum longus tendons. Both tendons are found within the flexor retinaculum of the ankle. They display a sliding movement with ankle flexion and are often hyperechoic. Then identify the pulsatile posterior tibial artery (Doppler use is optional). The tibial nerve at the ankle is often round to oval with a honeycomb appearance (Fig. 31.7). It is expected to lie posterior to the posterior tibial artery. Trace the tibial nerve proximally. The nerve is larger and is easier to identify more cephalad in the leg. It is also easy to image the nerve longitudinally by rotating the transducer 90°.
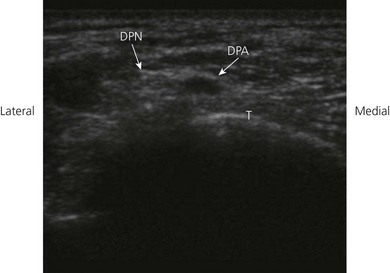
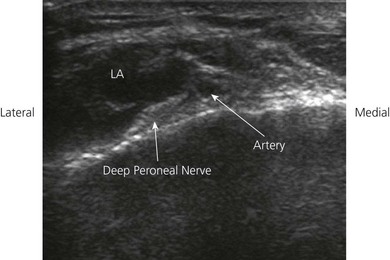
Deep peroneal nerve
Position the patient supine and bolster the foot with a pillow to expose the anterior and medial portion of the lower leg and foot. The lower limb is in the neutral position. The small deep peroneal nerve may be difficult to locate. This nerve lies adjacent to the anterior tibial vessels (above the ankle) and the dorsalis pedis at the ankle region. A 10–15 MHz transducer is placed on the dorsum of the foot along the intermalleolar line to locate the dorsalis pedis artery in the transverse view (Fig. 31.8) The predominantly hypoechoic deep peroneal nerve is found lateral to the dorsalis pedis artery and the extensor hallucis longus tendon (Fig. 31.9).
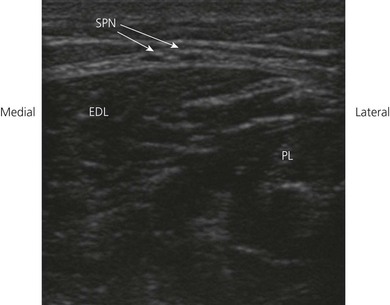
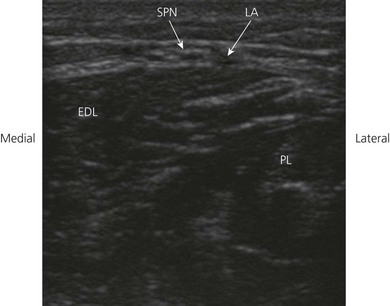
Superficial peroneal nerve
Position the patient supine and bolster the foot with a pillow to expose the anterior and lateral portion of the lower leg and foot. The lower limb is internally rotated for examination (Fig. 31.10). The superficial peroneal nerve can be identified sonographically between the peroneus longus and extensor digitorum longus muscles separated by the anterior crural intermuscular septum, using a 10–15 MHz transducer (Fig. 31.11). Distal to this, the nerve is superficial. The nerve pierces the fascia at a variable distance above the intermalleolar line (6–16 cm). The nerve typically divides below the level it pierces the fascia. Its detection is facilitated by the presence of fat around it.
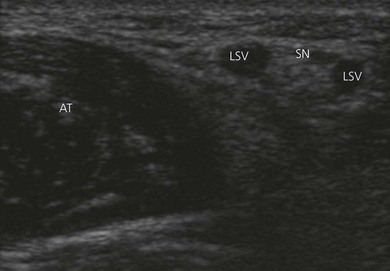
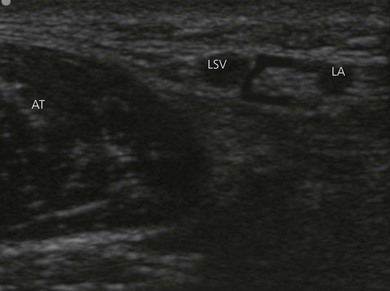
Sural nerve
Position the patient supine and bolster the foot with a pillow to expose the anterior and lateral portion of the lower leg and foot. The lower limb is internally rotated for examination. A tourniquet is placed around the proximal tibia to distend the lesser saphenous vein. A transverse image of the lesser saphenous vein with a 10–15 MHz transducer above the lateral malleolus is obtained (Fig. 31.12). The sural nerve is usually only identified after injection of local anesthetic around the lesser saphenous vein (Fig. 31.13).
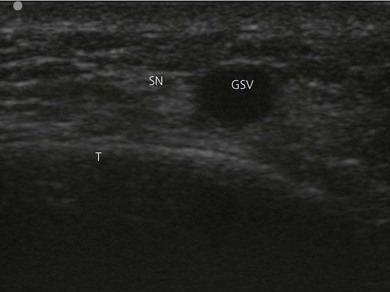
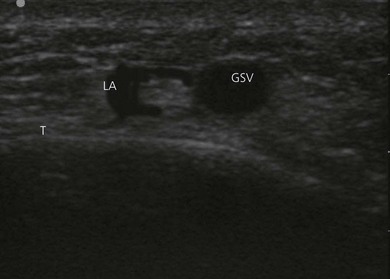
Saphenous nerve
Position the patient supine and bolster the foot with a pillow to expose the anterior and medial portion of the lower leg and foot. The lower limb is externally rotated for examination. A tourniquet is placed around the proximal tibia to distend the greater saphenous vein. A transverse image of the greater saphenous vein with a 10–15 MHz transducer above the medial malleolus is obtained (Fig. 31.14). The saphenous nerve is usually only identified after injection of local anesthetic around the greater saphenous vein (Fig. 31.15).
Technique
Landmark-based approach
Tibial nerve block
The block is performed by needle insertion on a line between the medial malleolus and Achilles’ tendon (Fig. 31.16), just posterior to the tibial artery. If paresthesia is elicited, the needle should be withdrawn slightly and 5 mL of local anesthetic be injected. If paresthesia is not reported, the needle is advanced to the bone and withdrawn slightly, and 10 mL of local anesthetic injected.
Deep peroneal nerve block
To block the deep peroneal nerve, a needle is inserted lateral to the extensor hallucis longus tendon and artery at the level of the intermalleolar line (Fig. 31.17). The needle is introduced perpendicular to the skin until bony contact is made, withdrawn slightly, and 4–5 mL of local anesthetic injected.
Saphenous nerve block
Saphenous nerve is blocked by subcutaneous injection passing medially from the insertion point of the deep peroneal nerve block toward the medial malleolus (Fig. 31.18), avoiding the saphenous vein. For this block, 4–5 mL of local anesthetic is adequate.
Superficial peroneal nerve block
The superficial peroneal nerve is blocked by a subcutaneous injection passing laterally from the insertion point of the deep peroneal nerve block toward the lateral malleolus (Fig. 31.19). For this block, 4–5 mL of local anesthetic is sufficient.
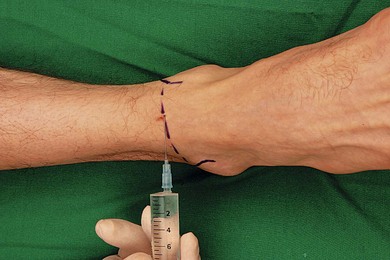
Sural nerve block
The sural nerve block is performed by needle insertion on a line between the lateral malleolus and the Achilles’ tendon (Fig. 31.20). If paresthesia is reported, the needle is withdrawn slightly and injection made. Otherwise, the needle is advanced until bony contact is made, withdrawn slightly, and the injection made.
Ultrasound-guided approach
The operator stands at the patient’s feet, with the ultrasound machine on the side to be blocked, (Fig 31.21). The skin is disinfected with antiseptic solution and draped. A sterile sheath (CIVCO Medical Instruments, Kalona, IA, USA) is applied over the ultrasound transducer with sterile ultrasound gel (Aquasonic, Parker Laboratories, Fairfield, NJ, USA). Another layer of sterile gel is placed between the sterile sheath and the skin. The ultrasound screen should be made to look like the scanning field. That is, the right side of the screen represents the right side of the field. Adjustable ultrasound variables such as scanning mode, depth of field, and gain are optimized.
Tibial nerve block
Both In Plane (IP) and Out of Plane (OOP) approaches can be used. The IP approach is commonly used for single-shot injection. Insert a 4–5 cm 22–25 G needle in-line with the ultrasound transducer (Fig. 31.22). Aim to place the needle tip on each side of the tibial nerve without puncturing the posterior tibial artery. Once satisfied with the needle position, inject 5–8 mL of local anesthetic. Observe local anesthetic injection in real time to judge adequacy of spread. Aim to see circumferential spread of hypoechoic local anesthetic solution around the nerve ‘donut sign’ (Fig. 31.23).
Deep peroneal nerve block
A 25-G 2.5-cm needle can be inserted using the OOP approach (Fig. 31.24). If the deep peroneal nerve is clearly visualized, inject 2–3 mL of local anesthetic on each side of the nerve. If the nerve is not clearly visualized, inject 2–3 mL of local anesthetic on each side of the artery in the subcutaneous plane. Observe local anesthetic spread around the nerve circumferentially in the subcutaneous plane above bone and at approximately the same level as the artery (Fig. 31.25).
Superficial peroneal nerve block
The superficial peroneal nerve can be identified sonographically between the peroneus longus and extensor digitorum longus muscles, separated by the anterior crural intermuscular septum proximal to the intermalleolar line. A 25-G 2.5-mm needle can be inserted using the OOP approach (Fig. 31.26). Inject 2–3 mL of local anesthetic on each side of the nerve. Observe local anesthetic spread around the nerve circumferentially (Fig. 31.27).
Saphenous nerve block
A transverse image of the greater saphenous vein above the medial malleolus is obtained. A 25-G 2.5-cm needle can be inserted using the OOP approach (Fig. 31.28). Inject local anesthetic (2–3 mL) on either side of the greater saphenous vein (Fig. 31.29).
Continuous technique
Clinical pearls
Fredrickson MJ. Ultrasound-guided ankle block. Anaesth Intensive Care. 2009;37(1):143-144.
Macaire P, Gaertner E, Capdevila X. Continuous post-operative regional analgesia at home. Minerva Anestesiol. 2001;67(9 Suppl. 1):109-116.
Redborg KE, Antonakakis JG, Beach ML, et al. Ultrasound improves the success rate of a tibial nerve block at the ankle. Reg Anesth Pain Med. 2009;34(3):256-260.
Redborg KE, Sites BD, Chinn CD, et al. Ultrasound improves the success rate of a sural nerve block at the ankle. Reg Anesth Pain Med. 2009;34(1):24-28.
Schurman DJ. Ankle-block anesthesia for foot surgery. Anesthesiology. 1976;4:348-352.