Ankle and Foot
Ankle
Anatomy
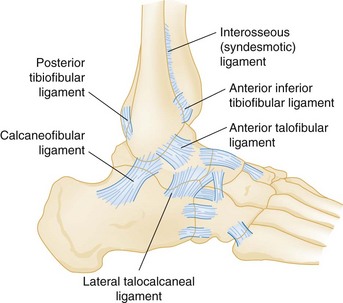
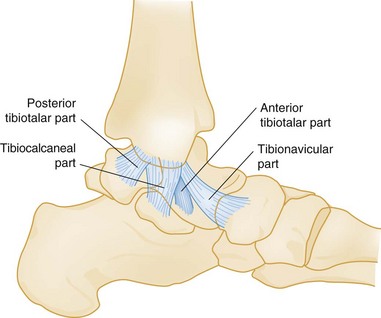
Three sets of ligaments—the syndesmotic ligaments, the lateral collateral ligaments, and the medial collateral ligaments—support the ankle joint and are essential to its stability (Figs. 58-1 and 58-2).
Pathophysiology
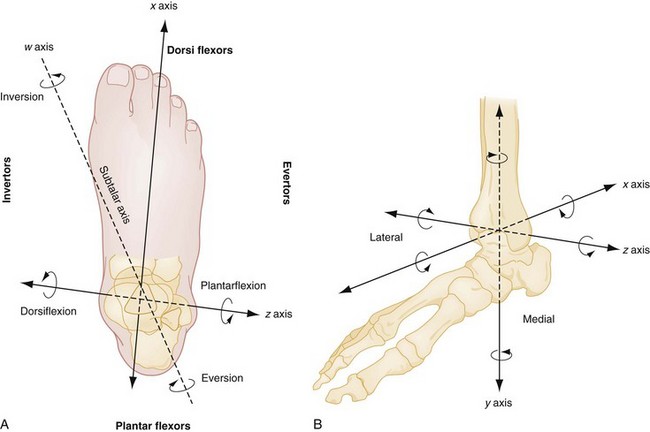
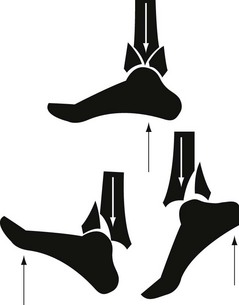
Ankle movements are complex and often involve more than one joint. It is best to consider the group of joints about the ankle as one unit, the ankle joint complex. This complex, which is made up of the talocrural joints and the talocalcaneal (subtalar) joints, allows movements along several axes of motion.1 Dorsiflexion and plantar flexion of the ankle joint complex occur primarily at the talocrural joints, rotating about the horizontal axis that passes through the medial and lateral malleoli (Fig. 58-3; see also Fig. 58-5). Motions of the ankle joint complex in conjunction with the midtarsal joints include inversion and eversion, which are rotational movements about the oblique subtalar axis involving the subtalar joint (see Fig. 58-3A), and abduction (external rotation) and adduction (internal rotation), which are rotational movements about the longitudinal axis of the tibia (see Fig. 58-3B).
The components providing stability to the ankle are best conceptualized as a ringlike structure surrounding the talus2 (Fig. 58-4). Disruption of one element of this ring does not, by itself, induce instability. Injury to one ring element, however, should prompt careful scrutiny for a second injury. Any disruption of two or more elements causes ankle instability and can significantly affect joint function.2
Clinical Features
The presence of immediate swelling and severe pain in the ankle region suggests serious ligament disruption, hemarthrosis, or fracture, and rapid progression of symptoms may represent more severe injury. Inability to bear weight immediately after an injury often implies a significant pathologic condition.3 Patient recollection of a “pop” sound should prompt consideration of ligament, tendon, or retinacular rupture but does not necessarily increase the probability of a fracture. Finally, the inciting event causing the ankle injury should be determined and, when necessary, further investigated.
Physical Examination
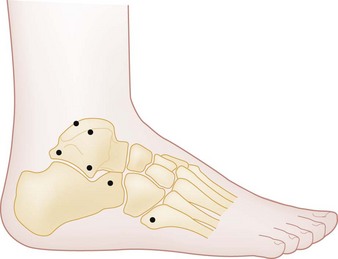
The examination of the ankle starts with an assessment of deformity, ecchymosis, edema, and perfusion, followed by active and passive range of motion. Assessment of point tenderness may localize ligament, bone, or tendon injuries, particularly when the patient is seen early. Palpation should include the medial and lateral collateral ligaments, the syndesmotic ligaments, the inferior and posterior edges of the medial and lateral malleoli, the entire length of the fibula and tibia, the anterior plafond, the medial and lateral dome of the talus (palpable with the ankle in plantar flexion), the base of the fifth metatarsal, the calcaneus, the Achilles tendon, and the peroneal tendons behind the lateral malleolus. Stress testing of the ankle joint, which is discussed later, should not be performed until a fracture has been excluded. An evaluation of weight-bearing ability should proceed only if clinical suspicion of a fracture is low, the location of tenderness does not indicate the need for plain radiography, or radiographs have ruled out a fracture.3 Specific clinical examination tests are discussed elsewhere in the appropriate sections.
Diagnostic Strategies
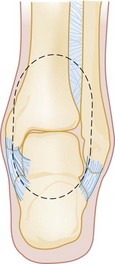
The anteroposterior, lateral, and mortise views make up the standard three-view radiographic series of the ankle. Although two-view ankle series have been studied, the likelihood of missing a subtle fracture is reduced with three views.4 Subtle fractures can be easily missed on ankle radiographs,5 and a standardized approach to radiograph interpretation can reduce the likelihood of missing low-energy ankle fractures6 (Fig. 58-5). The anteroposterior view identifies fractures of the medial and lateral malleoli, anterior tibial tubercle, distal tibia or fibula, talar dome, body and lateral and posterior process of the talus, and calcaneus. The lateral view identifies fractures of the anterior and posterior tibial margins, talar neck, posterior talar process, calcaneus, and any anterior or posterior displacement of the talus or pathology involving the talonavicular joint. On this view, any incongruity of the articular space between the talar dome and the distal tibia suggests ankle instability, particularly if narrowing of the anterior joint space is present. The lateral view is also useful in identifying an ankle effusion, which appears as a teardrop-shaped density displacing the normal fat adjacent to the anterior or posterior margin of the joint capsule. The presence of an effusion suggests the possibility of a subtle intra-articular injury, such as an osteochondral lesion of the talar dome.7
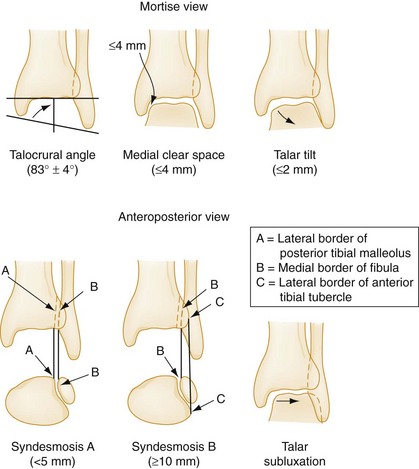
The mortise view, which is taken with the ankle in 15 to 25 degrees of internal rotation, is most important for evaluating the congruity of the articular surface between the dome of the talus and the mortise. The lines formed between the articular surfaces should be parallel, the joint space should appear uniform throughout the tibiotalar and talofibular components of the joint, and the medial clear space should not exceed 4 mm8 (Fig. 58-6).
In most cases of isolated blunt ankle trauma evaluated within 48 hours of injury, the Ottawa Ankle Rules (OAR) should be used to determine whether ankle or foot radiographs are necessary.3,9 The OAR state that an ankle radiographic series is required if there is pain in the malleolar region with any of the following findings:
• Bone tenderness at the posterior edge of the distal 6 cm or the tip of the lateral malleolus, or
• Bone tenderness at the posterior edge of the distal 6 cm or the tip of the medial malleolus, or
• Inability to bear weight (defined as the ability to transfer weight onto each leg regardless of limping) for at least four steps both immediately after the injury and at the time of evaluation
• Bone tenderness at the navicular bone, or
• Bone tenderness at the base of the fifth metatarsal, or
• Inability to bear weight for at least four steps both immediately after the injury and at the time of evaluation
The OAR have a sensitivity approaching 100% in detecting malleolar zone ankle fractures and midfoot zone fractures.3,9 The OAR were derived in an adult population and are not applicable in subacute or chronic injuries. The OAR appear to perform well in pediatric patients older than 5 years; however, results have varied, leading some researchers to propose alternative rules to address the unique aspects of this population.10–18
The decision rules for foot radiography, although applicable to blunt ankle trauma, apply only to the midfoot zone. The OAR were not designed to be general guidelines for foot radiography and certainly do not apply to the hindfoot or forefoot. Finally, the OAR are not applicable to intoxicated patients or those who are difficult to assess because of head injuries, multiple injuries, or diminished sensation related to neurologic deficits. Use of the OAR by specialized emergency and triage nurses has been found to have efficacy in application comparable to that for use by physicians.19–21 Although the OAR are well validated, their adoption and clinical impact remains variable.22,23
Other Imaging Techniques
Although plain radiography is the initial imaging modality of choice for ankle injuries, it can miss subtle ankle fractures, osteochondral lesions, stress fractures, or ligamentous injuries. When unexplained symptoms persist after negative or inconclusive findings on plain radiography, other imaging modalities or orthopedic consultation may be advisable.24
Radionuclide imaging (bone scanning) can detect soft tissue injuries, such as distal syndesmotic disruptions, stress fractures, and osteochondral lesions.25 Bone scan abnormalities are present once a patient is symptomatic and typically appear 1 to 2 weeks before radiographic evidence of a stress fracture. Because of its high sensitivity, a negative bone scan effectively rules out the diagnosis. Bone scan abnormalities are nonspecific, however, because infections and tumors also can lead to positive results (see further discussion on stress fracture imaging in the “Foot” section of this chapter), and bone scanning is not useful for follow-up because abnormalities can persist for up to 1 year after recovery.25 Radionuclide imaging is virtually always ordered on an outpatient basis and has been largely supplanted by computed tomography (CT) and magnetic resonance imaging (MRI). CT scanning provides superior bone imaging and is an excellent modality to delineate abnormalities not identified or incompletely characterized by other imaging techniques.24,25 CT can detect small fractures, subtle stress fractures, and ligamentous injuries and can facilitate surgical planning.24,25 Newer CT image reformatting techniques can be extremely helpful, including two-dimensional multiplanar reformatting to identify small fractures, three-dimensional volume rendering to show relationships between tendons and underlying bones, and shaded surface display to provide disarticulated views of joint surfaces and enhance diagnostic accuracy.26,27 MRI, although not typically performed emergently, provides unprecedented clarity in depicting soft tissue structures such as ligaments and tendons and can also delineate bone marrow changes associated with stress fractures before radiographic abnormalities appear.25 MRI can be helpful both in guiding management decisions and in following the patient’s response to therapy.28
Additional imaging techniques such as magnetic resonance or CT arthrography can be useful in the evaluation of chronic ankle pain to detect loose bodies, ligamentous injuries, cartilaginous abnormalities, impingements, or osteochondral lesions.29 CT/SPECT, which combines CT and radionuclide scanning with single photon emission computed tomography (SPECT), has been shown to significantly increase the diagnostic ability of imaging in osteochondral lesions, stress fractures, impingement syndromes, and osteomyelitis.30 The decision to perform specialized imaging of this nature is typically made through orthopedic or radiologic consultation; such studies are not performed in the emergency department (ED).
Specific Pathologic Conditions
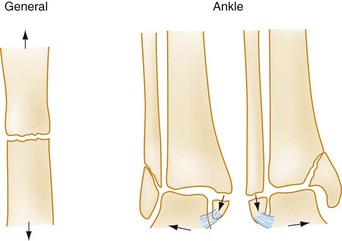
Pathophysiology: Fractures occur when a deforming force is sufficient to overcome the structural strength of a bone. A bone under tension breaks transversely along the axis of the deforming force31 (Fig. 58-7). Alternatively, ligamentous rupture or an avulsion fracture can occur at either end of a stressed ligament or tendon.
Management: The management of ankle fractures consists of identification and classification, assessment of stability, immediate reduction of fracture-dislocations that threaten soft tissues or neurovascular status, and specific treatment and disposition.
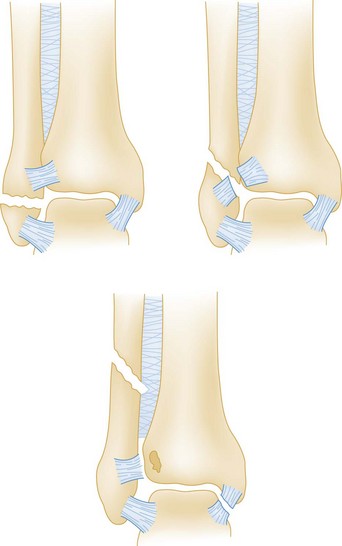
To date, no ideal system has been developed for the classification of ankle fractures. The classic Danis-Weber (Fig. 58-8) and Lauge-Hansen classification systems are based on fracture location and mechanism of injury, respectively.32 The Danis-Weber classification has predictive value for operative repair in isolated lateral malleolar fractures, as the location of the fibular fracture is related to the integrity of the syndesmosis, and is thus more useful to emergency physicians than the more complex Lauge-Hansen classification. Both systems have limitations, however, and neither accurately predicts management or clinical outcome in all situations. The Danis-Weber system does not adequately classify isolated medial malleolar fractures, bimalleolar, trimalleolar, or pilon fractures.33 By contrast, the Lauge-Hansen classification was intended to characterize ligamentous injury patterns based on the radiographic appearance of ankle fractures.34 According to a recent MRI study of 49 ankle fractures, however, this system was unable to predict patterns of ligamentous injuries in 53% of cases, and 17% of cases were unclassifiable.35 This study also found that more than 65% of cases had a complete ligamentous disruption associated with a related malleolar fracture, calling into question the stability of the fractures. It is clear that the Lauge-Hansen system in isolation is inadequate for classifying all fractures and has particular limitations in predicting soft tissue injuries. Modifications to these two classification schemes have been proposed to better describe ankle fractures and, more important, to predict outcome; however, because of their complex nature, most modified classification schemes are relegated to research applications and trauma registries.33–35
The injured ankle should be promptly immobilized, elevated, and iced to minimize swelling and further soft tissue damage. The presence of gross deformity with neurovascular compromise or skin tenting necessitates immediate intervention.36,37 Plain radiography before reduction can be helpful but should not delay reduction in injuries with obvious vascular compromise.
Disposition: In general, all displaced or potentially unstable ankle fractures require orthopedic consultation in the ED (Box 58-1). These injuries include all bimalleolar and trimalleolar fractures and unimalleolar fractures with contralateral ligamentous injuries (e.g., a lateral malleolar fracture with deltoid ligament disruption or a medial malleolar fracture with lateral collateral ligament disruption).38 In addition, all intra-articular fractures, especially those with step deformity of the articular surface, require early orthopedic involvement.
Extra-articular fractures that disrupt only one ring element generally can be treated with casting for 6 to 8 weeks. Orthopedic follow-up on an outpatient basis within 1 to 2 weeks of the injury is ideal in case operative intervention is required. The presence of any abnormal measurement on the mortise view (see Fig. 58-6) suggests instability and the need for orthopedic consultation in the ED. Avulsion fractures, in which the avulsed fragment is less than 3 mm in diameter and minimally displaced, can be treated in an identical manner to an ankle sprain.
The outcome of ankle fractures depends on the extent of injuries, the number of malleoli fractured, ankle stability, and patient age.32,33 For ankle fractures that require surgery, outcome is better in unimalleolar fractures over trimalleolar fractures, in isolated lateral malleolar fracture over isolated medial malleolar fractures, in multimalleolar fractures without medial malleolar fracture over those with malleolar fractures, and in cases with posterior fragments involving less than one third of the articular surface over larger fragments.39
Lateral Malleolar Fractures.: The stability of an isolated lateral malleolar fracture depends on the location of the fracture in relation to the level of the tibiotalar joint, which defines the distal portion of the syndesmotic ligament and the stability it provides to the ankle joint. The Danis-Weber classification (see Fig. 58-8) is useful and predictive of outcome in these types of unimalleolar fractures.33 This classification groups fractures into three groups (A, B, and C), each of which has three subgroups. Lateral malleolar fractures below the tibiotalar joint (Danis-Weber type A) rarely disrupt other bony or ligamentous structures, and in the absence of injury to the medial structures such fractures are unlikely to affect the dynamic congruity of the ankle joint.38 The management of uncomplicated lateral malleolar fractures involves casting for 6 to 8 weeks, with no weightbearing for at least the first 3 weeks, and ongoing follow-up to ensure proper union. Concomitant tenderness over the deltoid ligament may suggest a biomechanical disruption of both malleoli, an associated fracture of the medial malleolus, or an associated fracture of the posterior malleolus and warrants orthopedic consultation in the ED, especially if the medial clear space on the mortise view is widened (see Fig. 58-6).38 CT imaging can be useful in such situations as it may identify occult medial or posterior malleolar fractures.
Fibular fractures proximal to the tibiotalar joint line (a Danis-Weber type C injury; see Fig. 58-8) frequently, but not always, disrupt the distal tibiotalar syndesmosis and the medial structures and commonly require orthopedic consultation in the ED and operative intervention. Treatment of an isolated fracture at the level of the tibiotalar joint (a Danis-Weber type B injury; see Fig. 58-8) is controversial because 50% of these injuries are accompanied by an injury to the distal tibiofibular syndesmosis that may require operative intervention.40 Distal tibiofibular space measurements on plain radiography have a sensitivity of only 31% and a specificity of 83%, compared with CT scan, in detecting tibiofibular syndesmosis injuries.41 Tenderness on palpation of the syndesmotic ligament or a widening of the medial joint space on the mortise view adds further support to the need for emergency consultation.
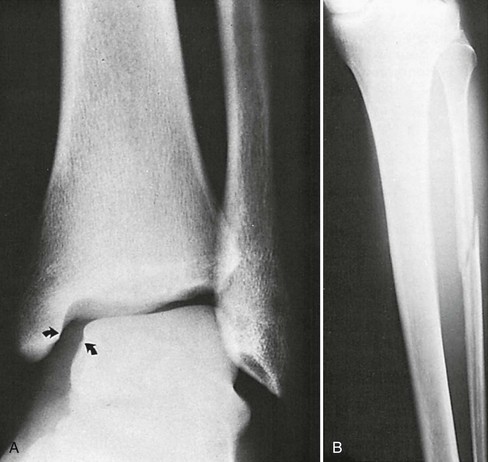
Medial Malleolar Fractures.: Medial malleolar fractures are usually the result of eversion or external rotation. These two forces exert tension on the deltoid ligament, causing an avulsion of the tip of the medial malleolus or a rupture of the deltoid ligament. Although they can occur in isolation, medial malleolar fractures are commonly associated with lateral or posterior malleolar disruption. Because of this, the identification of a medial malleolar fracture warrants a careful examination of the entire length of the fibula for tenderness, the presence of which warrants radiographic evaluation to rule out a proximal fibular fracture (Fig. 58-9).
An isolated nondisplaced medial malleolar fracture can be treated with casting for 6 to 8 weeks, with no weightbearing for at least the first 3 weeks and close orthopedic follow-up. Any displacement or concomitant disruption of the lateral components of the ankle warrants orthopedic consultation in the ED for consideration of operative management.38
Posterior Malleolar Fractures.: Isolated fractures of the posterior malleolus are rare and imply an avulsion of the posterior tibiofibular ligament. These injuries can be associated with proximal fibular fractures and medial and lateral collateral ligament sprains. Treatment usually consists of casting for 6 weeks, provided that no associated injury or ankle instability is present.42 Fractures involving more than 25% of the tibial surface usually require open reduction and internal fixation.38
Bimalleolar Fractures: Bimalleolar fractures involve the disruption of at least two elements of the ankle ring and are therefore unstable. These fractures result from adduction or abduction forces, the latter being more common.31 Rotational injuries also can cause bimalleolar fractures, as well as trimalleolar fractures if the posterior malleolus is involved.
The mechanism of injury often can be deduced from the appearance of the fractures.31 An abduction injury exerts tension on the medial malleolus, causing a horizontal fracture, and compresses the lateral malleolus, causing an oblique shear or a comminuted fracture (see Fig. 58-7). An adduction injury causes the reverse, leading to a horizontal fracture of the fibula and an oblique shear fracture of the medial malleolus. A rotational injury causes oblique or spiral fractures of the fibula or medial malleolus. Associated damage to other soft tissue structures (e.g., the syndesmosis) is common with bimalleolar fractures.
Controversy exists about whether such injuries should be treated closed or surgically.31,43 Unstable bimalleolar fractures require surgical intervention, however, and one study found that outcomes at 1 year after surgery were worse with bimalleolar fractures than with lateral malleolar fractures with deltoid ligament disruption.44
Rarely, stress fractures of the medial malleolus or distal fibula can be seen, particularly in athletes and runners. Plain radiographs may be nondiagnostic, but radionuclide bone scanning, CT, or MRI—the choice of which is often influenced by local availability—can establish the diagnosis.45 Most such injuries can be treated nonoperatively, but orthopedic consultation and follow-up are prudent.
Open Fractures
Open ankle fractures usually occur from severe isolated ankle injuries or multiple trauma and require immediate orthopedic consultation. After documentation of the neurovascular status and the extent of soft tissue trauma, gross contaminants should be removed from the wound, saline-soaked sterile gauze should be applied, and the injured leg should be splinted.36 Swabbing an open wound for bacterial culture and sensitivity testing is unnecessary. If significant deformity is present, immediate reduction before splinting is indicated.36 Tetanus immunoprophylaxis should be administered as appropriate. Because open fractures are invariably contaminated with bacteria, patients with these injuries should receive intravenous antibiotics.47,48 For low-energy injuries with mild to moderate contamination, a first-generation cephalosporin is usually sufficient.36,47,48 Heavily contaminated wounds require the addition of gram-negative bacterial coverage, typically an aminoglycoside.47,48 Adding either penicillin G or clindamycin (if penicillin allergic) as a third antibiotic is necessary for farm- or soil-related crush injuries, in which contamination with Clostridium perfringens can be present.47,48 In addition to the ankle radiographs, radiographs of the foot, tibia, and fibula should be obtained.
All open fractures benefit from early surgical intervention for débridement and irrigation.36 Therefore identification is crucial, and emergency orthopedic consultation must be sought for such injuries.
Complications: Early operative complications of closed and open ankle fractures include pin site infection, delayed skin necrosis, skin graft rejection, and osteomyelitis. Delayed complications of both operative and nonoperative treatment include malunion, nonunion, osteopenia, traumatic arthritis, chronic instability, ossification of the interosseous membrane, avascular necrosis, and complex regional pain syndrome.2,49
Pilon Fractures
Pilon fractures involve the distal tibial metaphysis and usually are the result of high-energy mechanisms, such as falls from a significant height. These injuries often are comminuted and associated with significant soft tissue trauma, devastation of joint architecture, and leg shortening (Fig. 58-10). Other, higher-priority injuries can be present in such situations.
Pathophysiology: Destot first coined the term hammer fracture to describe the way the head of the talus drives itself into the tibial plafond and causes a pilon fracture. The primary deforming force is one of axial compression, and the position of the foot at the time of injury determines the fracture location and pattern50 (Fig. 58-11). Secondary rotational or shear forces may cause increased comminution and fragment displacement with more extensive soft tissue injuries. One fourth of pilon fractures are open, and associated injuries include fractures of the calcaneus, tibial plateau, femoral neck, acetabulum, or lumbar vertebrae, as well as trauma to other major systems.
Management: Radiographic examination should include the entire tibia and fibula, as well as the ankle. The emergency management principles for open fractures, as outlined previously, should be applied. Treatment involves restoration of the articular surface and fibular length, combined with meticulous management of soft tissue injuries.50,51 Because surgical management is required, orthopedic consultation in the ED is necessary. Pilon fractures with low-grade soft tissue damage are managed with primary open reduction and internal fixation.51,52 In severe pilon fractures with extensive soft tissue damage, however, results are better with a two-stage approach involving initial length restoration and external fixation followed by anatomic reduction and internal fixation after soft tissue swelling has subsided.52–54
Complications: Complications of pilon fractures are common, particularly in more severe cases.51 Early complications include wound infection, skin sloughing, pin site infection, and wound dehiscence. Delayed and late complications include malunion, nonunion, leg shortening, post-traumatic arthritis, avascular necrosis, and protracted pain. Some patients with severe pilon fractures ultimately require arthrodesis.
Soft Tissue Injuries
Ligament Injuries: Ankle sprains are commonly seen in EDs, with a recent series estimating an annual incidence of 52.7 to 60.9 cases per 10,000 population.55 Ankle sprains also are one of the most common injuries in young athletes, and 40% of patients experience dysfunction for up to 6 months postinjury.56,57 The term ankle sprain refers to a potpourri of ligamentous and nonligamentous injuries.58 Even when ligamentous injury is certain, the ideal treatment approach remains controversial, and significant variation in clinical practice exists.55,59,60
Pathophysiology.: Most ankle sprains occur from extreme inversion and plantar flexion causing symptoms on the lateral aspect of the ankle. Usually the anterior talofibular ligament is injured first, followed by the calcaneofibular ligament if the deforming forces are sufficiently strong (see Fig. 58-1). Approximately two thirds of ankle sprains are isolated anterior talofibular ligament injuries, whereas 20% involve both anterior talofibular and calcaneofibular ligament injuries. In addition, the lateral talocalcaneal ligament may be stressed with an inversion injury, leading to avulsion fractures at either end of the attachment sites.61 Isolated calcaneofibular or posterior talofibular ligament injuries are rare.
Injuries of the distal tibiofibular syndesmotic ligaments are uncommon in the general population but may represent 10 to 20% of injuries in competitive athletes.62 Dorsiflexion and external rotation forces are usually responsible for this injury, the presence of which may significantly prolong the recovery time from lateral collateral ligament sprains.62
Ligamentous injuries are classified into three grades based on functional and presumed pathologic findings. A grade I injury involves ligamentous stretching without grossly evident tearing or joint instability. A grade II injury involves a partial tear of the ligament with moderate joint instability, often accompanied by significant localized swelling and pain. A grade III injury involves a complete tear of the ligament with marked joint instability, severe edema, and ecchymosis. This classification system, although commonly used, fails to characterize ankle injuries involving two or more ligaments, and it does not consider nonligamentous injuries. Although more comprehensive classification systems have been proposed,61 there is a strong association with increased gradation of ankle sprain and long-term risk of chronic instability, early osteoarthritis, chronic pain, and permanent disability.63,64
Clinical Features.: Although desirable, an accurate history of ankle position and injury mechanism is often unavailable. Inversion followed by external rotation of the ankle suggests the potential for deltoid or syndesmotic injury. Forced dorsiflexion with snapping may indicate peroneal tendon displacement. Previous injuries to the same ankle or symptoms of recurrent ankle instability or pain suggest the presence of a subacute or chronic pathologic process.
On physical examination, the presence of edema, ecchymosis, and point tenderness over the medial or lateral collateral ligaments or the syndesmotic ligaments suggests a ligamentous injury. Inability to bear weight in the absence of a fracture suggests the presence of a grade II or III ankle sprain.65 With inversion injuries, point tenderness may also be present along the distal fibula, the lateral aspect of the talus, the lateral aspect or anterior process of the calcaneus, or the base of the fifth metatarsal. Deltoid ligament tenderness necessitates palpation of the full length of the fibula to rule out a proximal fibular fracture (a type C Danis-Weber or Maisonneuve fracture; see Figs. 58-8 and 58-9) and a low threshold for imaging the entire tibia and fibula should exist. The fibular compression test, also known as the squeeze test, reveals fibular and syndesmotic injuries.62 To perform this test, the examiner places the fingers over the fibula and the thumb over the tibia at midcalf and squeezes the two bones. Pain anywhere along the length of the fibula suggests a fibular fracture or an interosseous membrane or syndesmotic ligament disruption at that location.62 Finally, the Achilles tendon should be assessed.
Diagnostic Strategies: Radiology.: Standard ankle radiographic views are useful to exclude fractures and to detect instability by the measurement of joint spaces (see earlier discussion and Fig. 58-6).8 Presence of avulsion fractures, which can be located at the bases of the malleoli, the lateral process of the talus, the lateral aspect of the calcaneus, the posterior malleolus, the lateral aspect of the distal tibia, or the base of the fifth metatarsal, constitute an important clue to the location of ligamentous injuries.
In addition to the standard mortise measurements previously discussed, two measurements on the anteroposterior radiograph further evaluate the distal tibiofibular syndesmosis (see Fig. 58-6).8 At the distal overlap between the fibula and the tibia, the distance between the posterior edge of the lateral tibial groove and the medial fibular cortex (syndesmosis A) should not exceed 5 mm.8 Furthermore, the amount of tibiofibular bony overlap (syndesmosis B) should be at least 10 mm.8 Measurements outside of these values suggest a syndesmotic diastasis. Stress radiographs, accomplished by taking radiographs during stress testing of the ankle, generally do not influence the emergency management of ankle sprains and are not recommended.66
Many injuries can masquerade as ankle sprains.58 Box 58-2 lists conditions to be considered in the differential diagnosis; Figure 58-12 shows locations of common fractures in or near the ankle that can be misdiagnosed as an ankle sprain.
Management.: Most ligament sprains, regardless of severity, heal well and result in a satisfactory outcome. To date, compelling evidence for a significant difference in outcomes between surgical and functional (nonsurgical) treatment is lacking. Limited data suggest that recovery times may be longer and complications more frequent with surgical treatment.67 Most patients with acute sprains of the ankle should start with functional treatment.68 For the minority who fail to respond, delayed operative repair of ruptured ligaments, sometimes years after the injury, has been shown to yield results equivalent to those with primary repair.68,69
Functional treatment, which is defined as a form of therapy in which the ankle is not fully immobilized, allowing either complete or partial joint function, starts in the ED with RICE therapy (rest, ice, compression, and elevation); however, significant variability exists in how this combination is applied, and the optimal methods remain unclear.60,61,70 The evidence to date suggests that lace-up ankle support is more effective in short-term edema reduction than semirigid ankle support, elastic bandaging, and taping. Elastic bandaging causes fewer complications than taping but appears to correlate with slower return to work and sports.60 One study suggests that compared with elastic bandaging, ankle bracing with a lace-up brace such as the Air-Stirrup Ankle Brace (Aircast, DJO Inc., Vista, Calif.) leads to improved functioning at both 10 days and 1 month.71
For grade I or II injuries, short-term protection with a tensor bandage, taping, a laced-up support, or a commercial walking boot or brace, with the optional use of crutches for a few days, is appropriate.68,70 For patients with first-time ankle sprains, treatment with a lace-up stirrup brace combined with elastic wrapping results in an earlier return to function compared with use of a brace alone, elastic wrap alone, or a walking cast.72 For severe grade II or grade III injuries, there is currently equipoise regarding the merit of immobilization compared with functional rehabilitation, with little high-quality evidence to guide therapy.73,74 A recent study supports a 10-day period of immobilization with a below-knee cast or Aircast ankle brace to speed recovery from ankle sprains, with immobilization leading to reduced symptoms and faster recovery compared with tubular compression bandages.75 However, a weakness in this study was the lack of a control group incorporating an active ankle physiotherapy program, known to be important for improved recovery. An accelerated functional rehabilitation program carried out over the first week of injury has also recently been shown to improve function in grade I and II ankle sprains in the short term.76
Because there is little evidence for a more favorable outcome with complete immobilization over functional treatment incorporating a removable brace, the use of a lace-up support or air cast that permits some ankle motion is generally preferable.68,74,77 Such patients should also use crutches to avoid weightbearing until they can stand and walk a few steps on the injured ankle without pain. How long crutches will be required varies significantly, ranging from a few days to 2 or 3 weeks. Follow-up care with the patient’s primary physician within the first 2 weeks is appropriate for minor sprains, whereas orthopedic or sports medicine referral on an outpatient basis is prudent for severe sprains.
Analgesics are often necessary for pain management in ankle injuries, and studies suggest that nonsteroidal anti-inflammatory agents, acetaminophen, or oral opioids for severe cases are efficacious.78–80 Topical diclofenac gel also has been shown to have efficacy in pain reduction and allowing early mobilization.67,81,82
After the acute management phase, the next two phases of functional treatment involve appropriate early rehabilitation and occur outside the ED.83 Phase two, which begins after swelling has subsided and the patient is able to bear weight easily, involves strengthening the peroneal and dorsiflexor muscles by isometric, concentric, and eccentric exercises. The final phase begins when full range of motion has been reestablished and the patient can exercise painlessly. This starts with exercises to rebuild motor coordination and proprioception, recondition the muscles, and increase endurance. The patient uses an ankle tilt board or disk to develop coordination and performs increasingly demanding functional activities (e.g., brisk walking, running, and figure-of-eight running to hopping, jumping, and cutting) to build up the muscle groups.83,84 With severe sprains the patient may benefit from the use of air casts, braces, or taping during the latter two phases of functional treatment and in the initial period of return to sports.83 The entire treatment program usually lasts 4 to 6 weeks, depending on the injury’s severity.61,70,85
Disposition.: Rarely, orthopedic consultation in the ED is indicated for an acute ligament sprain. Primary surgical repair of acute ligament rupture is controversial, and possible indications include sprains with displaced osteochondral lesions, complete tears of both the anterior talofibular and calcaneofibular ligaments in a young athlete, a ligament sprain associated with a fracture causing instability (e.g., a deltoid ligament rupture with a lateral malleolar fracture), and an acute severe sprain in a patient with a history of recurrent and severe sprains.61 Failure of nonoperative treatment also constitutes an indication for surgical repair; however, an orthopedic referral on an outpatient basis is adequate ED management.69
Despite appropriate treatment, chronic problems develop in 10 to 30% of patients with ankle sprains.70 These include functional instability, mechanical instability, chronic pain, stiffness, and recurrent swelling and occur more often in grade III ankle sprains.
Functional instability refers to the patient’s subjective sensation that the ankle gives way during activity. Although this may be a minor nuisance for some people, it can be devastating and debilitating for persons whose activities demand a high degree of ankle stability. Mechanical instability results from ligamentous laxity, which allows ankle joint movements beyond the physiologic range. In contrast to functional instability, mechanical instability can often be demonstrated clinically by the anterior drawer or talar tilt test and stress radiographs.61
Soft tissue abnormalities that cause chronic pain include synovial impingement, peroneal tendon subluxation or dislocation, intra-articular loose bodies, anterior tibiofibular syndesmotic ligament injuries, and degenerative arthritis. Bone-related causes of chronic pain include osteochondral lesions, fractures of the anterior process of the calcaneus, fractures of the lateral process of the talus, and anterior and posterior impingement.58,86
Achilles Tendon Rupture.: Achilles tendon rupture is most common in middle-aged men, and its causes are multifactorial. This condition is easily misdiagnosed, leading to a delay in therapy, a worse prognosis, and increased morbidity, including chronic weakness and loss of function. In the great majority of cases, a complete transection of the tendon is present; however, partial tears of the Achilles tendon can occur and may be more prone to misdiagnosis.
Achilles tendon rupture results from direct trauma or indirectly transmitted forces, including sudden unexpected dorsiflexion, forced dorsiflexion of a plantar-flexed foot, and strong push-off of the foot with simultaneous knee extension and calf contraction (as in a runner accelerating from the starting position). Factors predisposing to Achilles tendon rupture include preexisting disease such as rheumatoid arthritis, systemic lupus erythematosus, gout, hyperparathyroidism, or chronic renal failure, steroid use or injection, fluoroquinolone antibiotic therapy, and previous Achilles tendon rupture.87
The diagnosis of Achilles tendon rupture is primarily clinical. Patients usually describe a sudden onset of pain at the back of the ankle associated with an audible “pop” or “snap.” Although the pain can resolve rapidly, weakness in plantar flexion persists. On examination, a visible and palpable tendon defect may be noted 2 to 6 cm proximal to the calcaneal insertion in acute presentations but will be less apparent in delayed presentations because of hematoma or edema. Even in cases of complete Achilles tendon rupture, weak plantar flexion may still be possible because of the actions of the tibialis posterior, toe flexors, and peroneal muscles. This retained ability for plantar flexion often leads to the misdiagnosis of complete ruptures as ankle strains or partial tears in as many as 25% of cases.88 The classic maneuver to assess the integrity of the Achilles tendon is the Thompson test.89 This is performed with the patient prone and the knee flexed at 90 degrees or the feet hanging over the end of the stretcher. Alternatively, the patient kneels on a chair with both knees flexed at 90 degrees and the feet hanging over the edge. Squeezing the calf muscles in these two positions should cause passive plantar flexion of the foot. Absence of this motion, or a markedly weakened response compared with the uninjured side, suggests complete rupture. Another recently described diagnostic test, the reverse Silfverskiöld test, compares dorsiflexion of the injured ankle with that in the uninjured ankle while the patient is in the supine position. Achilles tendon rupture results in a notably increased degree of dorsiflexion compared with the uninjured side.90
Lateral radiographic views of the ankle may suggest rupture by showing opacification of the fatty tissue–filled space anterior to the Achilles tendon (Kager’s triangle) or an irregular contour and thickening of the tendon.88 Ultrasonography or MRI can demonstrate partial or complete tendon ruptures, but these studies are indicated only in cases in which diagnostic uncertainty exists.88
A lack of consensus exists regarding the choice between operative and nonoperative management in the treatment of Achilles tendon rupture.91–93 Surgical repair is routinely performed in active individuals owing to its lower incidence of rerupture. However, surgery carries higher rates of other complications, such as superficial or deep wound infections, in comparison with nonoperative management.91,94 In both types of management, early mobilization improves functional recovery without increasing rerupture rates.91,93 Minimally invasive surgery combined with early rehabilitation with postoperative functional bracing may further improve outcome.95,96 Achilles tendon rerupture after initial nonoperative treatment usually necessitates surgical repair, with substandard results compared with primary repair.97 ED orthopedic referral of patients with Achilles tendon rupture is necessary to determine the appropriate management.
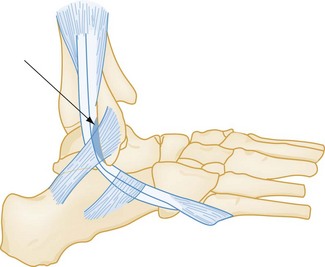
Peroneal Tendon Dislocation or Tear.: The peroneal muscles are the primary evertors and pronators of the foot and also participate in plantar flexion. The peroneus longus and brevis tendons use the posterior peroneal sulcus (the fibular groove), located behind and underneath the lateral malleolus, as a pulley for their midfoot insertions. The peroneus brevis tendon inserts onto the tuberosity of the fifth metatarsal, and the peroneus longus tendon courses beneath the cuboid to insert onto the medial cuneiform and base of the first metatarsal. The superior peroneal retinaculum (Fig. 58-13), a fibrous structure running from the distal fibula to the posterolateral aspect of the calcaneus, maintains the peroneal tendons against the fibular groove.
Anterior subluxation or dislocation of the peroneal tendons occurs as a result of a tear of the superior peroneal retinaculum attachment from the fibula.98,99 This infrequent injury is commonly misdiagnosed as an ankle sprain and can occur in isolation or concomitant with other sprains or fractures. The mechanism of injury usually is forced dorsiflexion with reflex contraction of the peroneal muscles, resulting in avulsion of the retinaculum and anterior displacement of the peroneal tendons.98
Patients with a peroneal tendon dislocation complain of sudden pain and a snapping sensation over the posterolateral ankle associated with weakness of eversion. Tenderness and swelling over the lateral retromalleolar area (a location not typically involved in ankle sprains) are characteristic. When accurate examination is not precluded by swelling, the dislocated tendons also may be palpable near the inferior tip of the lateral malleolus. Inability to actively evert the foot when it is held in dorsiflexion or frank subluxation of the tendons with this maneuver confirms the diagnosis. Findings on plain radiography are often normal; however, 15 to 50% of patients will be found to have an associated avulsion fracture of the lateral ridge of the distal fibula. An MRI study or ultrasound can be helpful in confirming the diagnosis. All patients with a suspected or confirmed peroneal tendon dislocation should be referred for orthopedic follow-up because these injuries require surgical repair.99,100 Spontaneous healing is rare in untreated cases, and chronic ankle instability and pain are common sequelae. Peroneal tendons also can tear longitudinally; such injuries manifest either acutely or subacutely with recurrent pain and swelling during activities.100,101
Tibialis Posterior Tendon Rupture.: The tibialis posterior is primarily responsible for plantar flexion and inversion along the subtalar joint. Its tendon uses the posteroinferior surface of the medial malleolus as a pulley and inserts onto the navicular, the medial cuneiforms, and the bases of the second through the fifth metatarsals. The peroneus brevis opposes the action of the tibialis posterior. With rupture of the tibialis posterior tendon, the peroneus brevis becomes unopposed and the medial longitudinal arch loses its muscular support, leading to valgus deformity of the hindfoot and a unilateral flatfoot.102
The mechanism of traumatic tibialis posterior rupture involves forced eversion.102 In addition to a unilateral flatfoot, pain and swelling on the medial aspect of the ankle are seen. Tenderness is present over the navicular, and the patient cannot perform a toe raise on the affected side. In addition, the patient with a tibialis posterior tendon rupture is unable to invert the foot when it is in plantar flexion and eversion. With a unilateral flatfoot, an observer standing behind the patient can see “more toes” on the lateral aspect of the affected side—a classic sign.102 Plain radiography can exclude other bone abnormalities. Ultrasonography and MRI are useful imaging modalities to diagnose this condition.102 Orthopedic consultation is indicated for tibialis posterior tendon ruptures, because surgical repair often is necessary.
Other Tendon Injuries.: The tibialis anterior is the primary dorsiflexor of the foot. Its tendon courses under the superior extensor retinaculum and inserts onto the navicular, the medial cuneiform, and the base of the first metatarsal. Tenosynovitis of the tibialis anterior tendon is associated with overuse and characterized by swelling, tenderness, and crepitus along the tendon. Treatment involves RICE therapy, analgesia, and close follow-up. Rupture of the tibialis anterior is rare and often is misdiagnosed as lumbosacral radiculopathy or peroneal nerve palsy because of the footdrop it produces. This condition requires orthopedic consultation in the ED because surgical repair is usually necessary.
The flexor hallucis longus is responsible for flexion of the great toe and participates in plantar flexion of the foot. Its tendon courses behind the medial malleolus through a fibro-osseous canal and inserts onto the distal phalanx of the great toe. Flexor hallucis longus tendinitis, also called dancer‘s tendinitis, most often occurs at the fibro-osseous canal.103 On examination, tenderness and edema posterior to the medial malleolus are noted, and passive extension of the first metatarsophalangeal (MTP) joint causes significant pain when the foot is in neutral position. Initial treatment involves rest, nonsteroidal anti-inflammatory drugs, and a short course of immobilization. Orthopedic follow-up on an outpatient basis should be arranged to ensure proper resolution. Rarely, surgical intervention may be necessary.103
Ankle Dislocations: Ankle dislocations are described according to the direction of displacement of the talus and foot in relation to the tibia. Thus dislocation may be upward, posterior, medial, lateral, posteromedial, or anterior. Medial dislocation is the most common. Most dislocations involve associated ankle fractures; rarely, however, dislocations can occur without fracture. The mechanism in all dislocations begins with axial loading of a plantar-flexed foot, which forces the talus either anteriorly or posteriorly from the ankle mortise. The eventual position of the dislocation depends on the position of the foot at the time of injury and the direction of the displacing force. Ankle dislocations can be closed or open and most commonly result from significant falls, motor vehicle collisions (MVCs), or high-speed sports.37 The neurovascular supply to the foot usually is intact but may be compromised in open dislocations.104
ED management involves the assessment of neurovascular status and tendon function, followed by rapid reduction. Radiographs are helpful but should not delay reduction in cases when vascular compromise or skin tenting is present.37 After appropriate procedural sedation and analgesia, the patient is placed supine and the knee is flexed to 90 degrees. Distraction of the foot, followed by a gentle force to reverse the direction of the dislocation, usually accomplishes the reduction.105 Reassessment of the neurovascular status, splint immobilization, ankle elevation, and postreduction radiography should follow. Open dislocations require the same management as previously discussed for open fractures. The prognosis with an ankle dislocation is usually good, although open fractures are associated with an increased incidence of complications.104,105
Foot
Anatomy
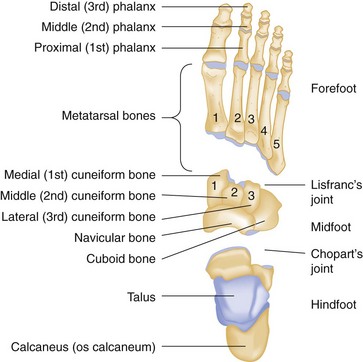
The foot is composed of 28 bones and 57 articulations (Fig. 58-14). It can be divided into three anatomic and functional regions: the hindfoot, which contains the talus and calcaneus; the midfoot, which contains the navicular, cuboid, and cuneiforms; and the forefoot, which contains the metatarsals, phalanges, and sesamoids. The midtarsal joints (Chopart’s joint) join the hindfoot and midfoot, and the tarsometatarsal joints (Lisfranc’s joint) join the midfoot and forefoot. The inferior aspect of the talus has three articulations with the calcaneus that are collectively known as the subtalar joint.
The foot is capable of numerous weight-bearing and non–weight-bearing motions (see Fig. 58-3), which vary at each articulation. Inversion and eversion of the hindfoot occur primarily through the subtalar joint, adduction and abduction of the forefoot through the midtarsal joints, and flexion and extension through the MTP and interphalangeal (IP) joints. The relative importance of specific bones in supporting the body’s weight varies with changes from the static to the mobile state. The biomechanics of walking and running are extremely complex, and significant forces are imparted to the foot’s structures during these precisely coordinated activities.106
Clinical Features
The structures of the foot are uniquely accessible to palpation and assessment. A directed examination, specific for the patient’s complaint, is most useful in the ED.107
If the patient is ambulatory, observation of the gait provides information on the degree of disability and pain and the potential for serious injury. Formal examination begins with observation of the foot in its position of rest, normally one of slight plantar flexion and inversion. Swelling, deformity, ecchymosis, open wounds, color, and temperature should be noted. The use of ecchymosis to localize injuries can be misleading because of pooling of blood in dependent areas after tracking through tissue planes. All patients should have a neurovascular examination with assessment of the dorsalis pedis and posterior tibial pulses, sensation, and motor function. Precise localization of pain or crepitus, when not precluded by swelling, is extremely valuable and facilitates appropriate use of further diagnostic tools. An awareness of anatomic landmarks, which some research suggests may be suboptimal among clinicians,108 is important in this process. The entire foot should be gently palpated over both the dorsal and the plantar surfaces, methodically progressing from the heel to the toes. Particular attention should be paid to areas in which injuries commonly occur, such as the base of the fifth metatarsal.
Diagnostic Strategies: Radiology
Plain radiography of the foot may be indicated by history, physical examination, or both. Standard three-view radiographs of the foot consist of anteroposterior, lateral, and 45-degree internal oblique projections.109 The lateral projection gives the best imaging of the hindfoot and soft tissues, whereas the anteroposterior and oblique projections give the best imaging of the midfoot and forefoot. The numerous overlapping bones of the foot demand this complete radiographic series in all patients for whom radiographic examination is indicated.110 Injuries to the hindfoot also warrant the addition of standard ankle projections and, when indicated, calcaneus views.
Foot radiographs can be difficult to interpret.111 Moreover, foot fractures are often minimally displaced or nondisplaced, increasing the challenge of radiographic diagnosis. Several additional views improve the imaging of specific areas of the foot. Coned views, weight-bearing radiographs, or a 45-degree external oblique projection can be useful, particularly for detection of midfoot and forefoot pathology. The most commonly obtained atypical view is the Harris (axial) view for visualizing the calcaneus and subtalar joints. Special magnification radiographs or stress radiographs also may be useful in selected cases.
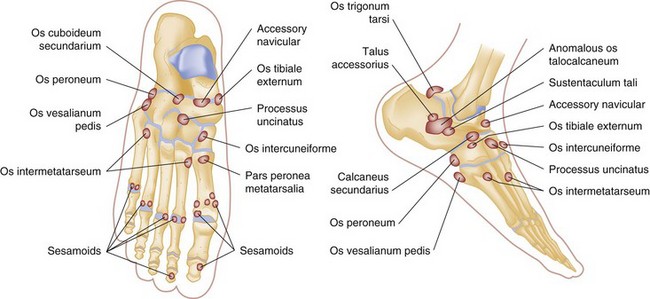
Interpretation of plain radiographs can be complicated by the numerous accessory centers of ossification and the presence of sesamoid bones (unipartite and multipartite) that exist as normal variants in up to 30% of the population (Fig. 58-15). The most commonly seen accessory bones are the os trigonum, os tibiale externum (also called an accessory navicular bone), os peroneum, and os vesalianum.112 These can be differentiated from fractures by their smooth corticated surfaces. Comparison radiographs of the opposite foot may be helpful, although such variants are not inevitably bilateral. Accessory bones themselves can also fracture or cause pain syndromes.113
Because of the limitations of plain radiography, other imaging techniques have gained importance for specific foot injuries. Radionuclide imaging (bone scanning) can be useful for evaluating unexplained foot pain or pain in athletic injuries.114 In the setting of acute foot trauma, this modality often can demonstrate subtle fractures not visible with plain radiography. Historically, bone scanning has been the standard modality for the diagnosis of stress fractures; however, MRI has comparable sensitivity and better specificity and has emerged as the imaging modality of choice for this diagnosis.25,115
The CT scan can be valuable when complex articulations and overlapping bones make standard radiographs difficult to interpret, particularly in the midfoot and hindfoot.116,117 As a result of the wide availability and superiority of CT scanning, plain film tomography is now virtually obsolete. CT is an excellent modality for imaging complex anatomy, including the subtalar joint, the calcaneus, and the tarsometatarsal (Lisfranc) joint complex. Three-dimensional CT images provide unprecedented clarity and detail.27
MRI has been used to investigate many of the same fractures and dislocations imaged by CT, and the two modalities can be used in a complementary manner.24,28,118,119 As in the ankle, the most significant role of MRI is in the delineation of soft tissue conditions, such as athletic injuries and tendon ruptures, where it has become the imaging modality of choice. In some conditions involving the ankle joint, magnetic resonance arthrography on an outpatient basis can be useful.120
Specific Pathologic Conditions
Hindfoot Injuries
Principles of Disease: Anatomy.: The word talus is related to the Latin taxillus, meaning “a small die or cube,” and dates back to the time of the Roman Empire, when soldiers made dice out of the ankle bones of horses. An appreciation of the unique anatomy of the talus is crucial to an understanding of the pathophysiology and treatment of talar fractures and dislocations. The talus is the second largest tarsal bone and has seven articulations making up 60% of its surface. It is divided into three regions: the head, which articulates with the navicular and calcaneus; the body, which articulates with the tibia, fibula, and calcaneus; and the neck, which joins the head and body and is the only portion of the talus that is predominantly extra-articular. The talus is the only bone in the lower extremity with no muscular attachments and is held in position by the malleoli and ligamentous attachments. The anterior width of the talus is greater than the posterior, causing it to be less stable and more prone to dislocation when the foot is plantar-flexed.
Pathophysiology.: Talar fractures are the second most common tarsal fracture after fractures of the calcaneus. They are best grouped into minor and major fractures, with minor fractures being the more common.121 Stress fractures of the talus also can occur. Minor talar fractures include avulsion fractures of the superior neck and head, and the lateral, medial, and posterior aspects of the body.122 These fractures often involve the same mechanism as that for ankle sprains (see Fig. 58-12 and Box 58-2): a combination of plantar flexion or dorsiflexion and an inversion force. Lateral process fractures, previously uncommon, have been described with snowboarding and can be occult on plain radiographs.123 Osteochondral lesions of the talar dome also fall into the minor fracture category.
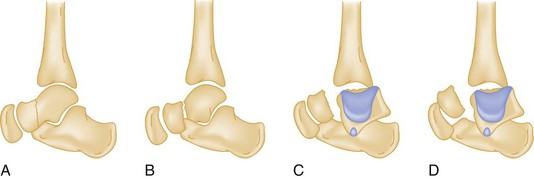
Hawkins classified talar neck fractures into three categories (Fig. 58-16): Type 1 fractures are nondisplaced; type 2 fractures show subtalar subluxation; and type 3 fractures, 50% of which are open, involve a dislocation of the talar body from the ankle and subtalar joint. A fourth type that has been added to this classification involves the additional distraction of the talonavicular joint. This classification is important descriptively and because the type of fracture influences both treatment and outcome. Long-term complications, including avascular necrosis and arthritis, are common with talar neck fractures and more likely with increasing displacement.124
Talar body fractures include many of the minor talar fractures previously listed.125 Major talar body fractures are uncommon and usually result from falls with axial compression of the talus between the tibial plafond and the calcaneus.
Clinical Features.: Talar fractures range from obvious open fractures to subtle fractures requiring special imaging techniques to diagnose. Typically, a history of a twisting injury, fall, or high-energy impact can be elicited. Dorsal swelling and tenderness over the talus are characteristic findings. Although ankle motion may be preserved, inversion and eversion of the hindfoot often are painful.
Diagnostic Strategies: Radiology.: With minor talar fractures, radiographs can be misinterpreted as normal in appearance. Even when supplemental views are obtained, CT or MRI may be required for visualization. Standard foot and ankle radiographic views usually demonstrate major talar fractures (Figs. 58-17 and 58-18), with the anterior and oblique projections showing talar alignment within the mortise and the lateral projection showing the talar neck and alignment of the posterior aspect of the subtalar joint. Normal variants, such as an os trigonum or os supratalare (see Fig. 58-15), are occasionally encountered and should be differentiated from fractures. Specialized imaging by CT or MRI is often required for complete assessment of talar fractures.
Management.: Major talar fractures require precise reduction because more weight per unit area is borne by the superior surface of the talus than by any other bone. Most talar fractures involve multiple articular surfaces, and adequate repair often necessitates open reduction and internal fixation. Many minor talar fractures heal with casting, and the initial treatment should be with a non–weight-bearing below-knee cast or posterior plaster slab. Fragments larger than 5 mm in diameter may require excision. Other minor fractures, such as displaced lateral process fractures, require operative fixation because of their articular involvement.
Disposition.: All patients with talar fractures require orthopedic consultation in the ED or referral for early orthopedic follow-up on an outpatient basis. Most minor talar fractures are suitable for outpatient follow-up and heal well, although some result in post-traumatic arthritis. Major talar fractures have a high incidence of complications, the most significant of which is avascular necrosis.126 Outcome depends on the degree of anatomic reduction attained and preservation of the vascular supply. The risk of avascular necrosis increases with delay to reduction and with increasing talar displacement, ranging from 10% for type 1 neck fractures to 70% or more for type 3 neck fractures. Major fractures of the talar body are also prone to avascular necrosis, the risk of which doubles if an associated dislocation is present. Other potential complications include skin infection, skin necrosis, post-traumatic arthritis, malunion, delayed union, nonunion, and predisposition to peroneal tendon dislocation. The incidence of each complication varies with the type of fracture and the aggressiveness of ED and operative management.
Osteochondral Lesions: Osteochondral fractures of the talar dome account for 1% of talar fractures and are usually diagnosed late in the clinical course after ankle trauma.127 The broader term “osteochondral lesion” is preferable, as it describes injuries of any origin involving the articular surface and/or subchondral region of the talus or tibial plafond and can thus involve cartilage, subchondral bone, or both.128 These injuries are now thought to be more common than previously appreciated.128–130 Many synonyms for this entity, including transchondral fracture and dome fracture of the talus, exist. Mechanisms identical to those causing ankle sprains are the most common cause; however, a significant number of these injuries cannot be ascribed to an acute traumatic event.
An osteochondral lesion should be considered in any patient with ligamentous ankle injury accompanied by gross edema and an effusion on plain radiographs.7 The diagnosis is often missed initially and not made until the patient returns with chronic ankle pain.131 Physical findings usually are nonspecific, although localized tenderness over the posteromedial aspect of the talus and increasing pain with exertion, weightbearing, or passive plantar flexion may be noted. Standard-view radiographs are commonly normal in appearance or show subtle and easily overlooked abnormalities, although specialized views may be helpful to assess the subchondral surfaces.128 Bone scanning has been advocated as a nonspecific screening modality129; however, its role is becoming increasingly historic as CT or MRI studies are often required for identification and classification (Fig. 58-19). MRI is emerging as the imaging modality of choice for osteochondral lesions, owing to its ability to detect bone marrow edema and cartilage, and MRI classification schemes exist.128–131
When an osteochondral lesion is diagnosed or suspected, outpatient orthopedic referral is advised. The natural history of osteochondral lesions is poorly defined and variable132; however, chronic ankle discomfort and osteoarthritis are potential sequelae. Osteochondritis dissecans, a subacute or chronic defect, may develop in the talar dome after inadequate treatment of an osteochondral lesion. In general, however, with appropriate care, either by cast immobilization for up to 6 weeks or operative management, the prognosis is good, particularly if treatment begins within 12 months of symptom onset. The benefit of operative management, often done arthroscopically, varies with the type of lesion and its anatomic location.133 The previous discussion underscores the necessity for orthopedic evaluation when a patient has persistent unexplained ankle pain after a previous “sprain.”
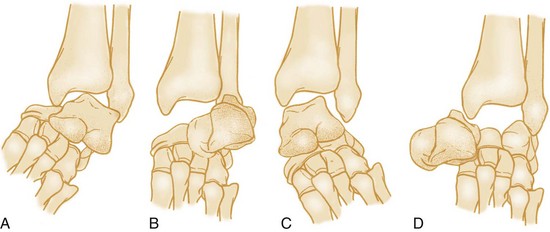
Principles of Disease: Pathophysiology.: Subtalar dislocation, also called peritalar dislocation, is the simultaneous disruption of both the talocalcaneal and talonavicular joints without disruption of the tibiotalar joint (Fig. 58-20). This occurs when the talonavicular and talocalcaneal ligaments rupture while the stronger calcaneonavicular ligament remains intact. Subtalar dislocations are rare and are classified by the direction the foot takes in relation to the talus.134 Anterior and posterior dislocations occasionally occur; however, most subtalar dislocations are either medial or lateral, with medial dislocations accounting for a majority of cases. Dislocation of the calcaneus is an exceptionally rare event that is distinct from subtalar dislocation and involves disruption of the talocalcaneal and calcaneocuboid articulations.
Clinical Features.: Obvious deformity typically is present, often with tension of the skin on the side opposite the direction of dislocation. Neurovascular status should be carefully assessed, although it is rarely compromised. Swelling can mask the extent of the injury, thus diagnosis can be delayed or missed if only ankle radiographs are obtained.
Diagnostic Strategies: Radiology.: Although standard foot radiographic views are diagnostic, properly positioning the patient for these may be difficult. Inadequate films can delay diagnosis and treatment. The single most helpful radiograph is an anteroposterior view of the foot, which will demonstrate the talonavicular dislocation.
Management.: Subtalar dislocations require expeditious reduction.135 More than 80% of closed subtalar dislocations can be treated with closed reduction, either with procedural sedation and analgesia in the ED or with general anesthesia. Closed reduction is performed by flexing the knee and applying longitudinal traction to the foot with initial accentuation, followed by reversal of the deformity (with use of eversion for medial dislocations and inversion for lateral dislocations). Sometimes direct pressure over the head of the talus aids in reduction. Closed reduction may be impossible because of buttonholing of the talus through the extensor retinaculum, entrapment in the peroneal tendons, or associated fractures. After reduction, immobilization in a below-knee cast for 4 to 6 weeks is indicated.
Total Talar Dislocation: Total talar dislocation is an extremely rare and devastating injury requiring orthopedic consultation in the ED. In these injuries, which are the end result of the same forces that produce subtalar dislocation, the entire talus is distracted from all of its articulations (see Fig. 58-20). Most are open, and infection and avascular necrosis are common complications.136
Principles of Disease: Anatomy.: The calcaneus is the largest bone in the foot and the most commonly fractured tarsal bone.137 It articulates with the talus superiorly (forming the subtalar joint) and with the cuboid anterolaterally.
Pathophysiology.: Falls with direct axial compression cause most calcaneal fractures. Because of this high-energy mechanism, associated injuries are common: 7% of calcaneal fractures are bilateral, 25% are associated with other lower extremity injuries, and 10% are associated with spinal injuries, typically vertebral compression fractures.
Numerous classification schemes have been developed for calcaneal fractures. Perhaps the most intuitive is simple categorization of the fracture as either extra-articular or intra-articular. Extra-articular fractures usually involve the addition of a rotatory mechanism and include fractures of the sustentaculum tali and the calcaneal tuberosity and oblique fractures of the calcaneal body. Avulsion fractures of the anterior process by the bifurcate ligament (which joins the calcaneus, navicular, and cuboid) also are included in this category. Isolated calcaneal tuberosity fractures are rare but may require more expeditious treatment when displaced owing to compromise of the skin overlying the Achilles tendon.138 Up to 75% of calcaneal fractures are intra-articular, ranging in severity from nondisplaced single fractures to severely crushed, comminuted fractures. Because of the cancellous nature of the calcaneus, fractures are frequently comminuted. Calcaneal stress fractures may also occur.
Clinical Features.: The typical history is one of a fall resulting in a direct impact on the heel or heels. Physical examination reveals pain, swelling, and tenderness over the affected heel, and weightbearing on the hindfoot is usually impossible. In cases of significant fracture, the heel may be deformed when viewed from behind, appearing short, wide, and tilted. Ecchymoses may extend over the entire sole, a finding not seen in isolated malleolar fractures. The presence of compartment syndrome or associated injuries such as vertebral compression fractures should be considered.
Diagnostic Strategies: Radiology.: Standard radiographic views of the foot and ankle should be obtained. The anteroposterior view of the foot shows the calcaneocuboid joint and the anterosuperior calcaneus, whereas the lateral view shows the posterior facet and can demonstrate compression of the calcaneal body (Fig. 58-21). In addition, a Harris (axial) view, when not precluded by pain, should be obtained to image the calcaneal tuberosity, subtalar joint, and sustentaculum tali. Anterior process fractures require differentiation from a calcaneus secundarius accessory ossification center (see Fig. 58-15).139
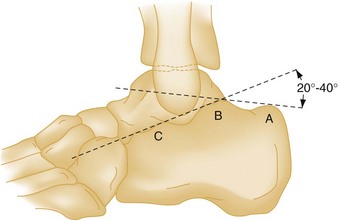
Two assessments are critical to the management of calcaneal fractures: whether the fracture involves the subtalar joint, and the degree of depression of the posterior facet.140 Compression fractures are not always obvious, and measurement of Boehler’s angle (Fig. 58-22) can be helpful. Because Boehler’s angle may be normal even in the presence of severely comminuted calcaneal fractures, it has been considered more useful prognostically than diagnostically, although recent findings raise questions regarding the prognostic utility of this measurement as well.141 Boehler’s angle is measured on the lateral view as the angle between two lines, one between the posterior tuberosity and the apex of the posterior facet and the other between the apex of the posterior facet and the apex of the anterior process. Although several values for this measurement have been cited, an angle of 20 to 40 degrees defines a normal range with the best diagnostic performance.142 An angle of less than 20 degrees suggests a compression fracture. Comparison measurement of the uninjured side may be helpful in questionable cases; however, the degree of variability between feet in the same individual is poorly defined, and advanced imaging is preferable in such situations.
Imaging of the calcaneus can be difficult because of the complex three-dimensional nature of its articulations. Plain radiography can underestimate injury severity, and the CT scan has revolutionized the assessment of calcaneal fractures, with good correlation of findings with outcome.140,143 MRI is also an excellent modality for imaging the hindfoot and has a role in assessment of selected calcaneal fractures.
Management.: The management of intra-articular or displaced calcaneal fractures is controversial, with many operative and nonoperative approaches described.140 Minimally invasive surgical approaches and new technologies are changing the surgical approach to these injuries.144 A recently published 15-year follow-up of a randomized trial comparing operative and nonoperative management of displaced intra-articular calcaneal fractures found no differences in clinical outcomes between the treatment groups.141 The treatment of nondisplaced extra-articular fractures usually involves casting for 6 to 8 weeks.
Disposition.: Intra-articular or displaced calcaneal fractures require orthopedic consultation in the ED. Outpatient orthopedic follow-up care can be arranged for more innocuous injuries, provided that this approach is consistent with local practice and no associated injuries that warrant hospitalization are present. In considering outpatient follow-up, it is important to bear in mind that plain radiographs often significantly underestimate the extent and severity of calcaneal fractures. Minor extra-articular fractures usually heal uneventfully; however, with significant calcaneal fractures, complications, including compartment syndrome, are frequent. In both conservatively and surgically treated patients, the incidence of long-term pain, loss of joint mobility, and functional disability approaches 50%.145
Midtarsal Joint Injuries: The midtarsal joint (Chopart’s joint) is composed of the talonavicular and calcaneocuboid joints. Injury in this area, although rare, can occur with any ankle, hindfoot, or midfoot trauma. Midtarsal joint injuries usually result from forced dorsiflexion and often are associated with other significant fractures. Sprains, fracture-subluxations and fracture-dislocations, and an isolated “swivel dislocation” (a variant of a subtalar dislocation) all can occur at the midtarsal joint. Pain, swelling, inability to bear weight, and tenderness over the midtarsal joint are usual findings. Although standard radiographs often are abnormal in appearance, the diagnosis frequently is overlooked or delayed, with symptoms ascribed to an ankle sprain (see Fig. 58-12 and Box 58-2). The possibility of a midtarsal joint injury should be considered with any isolated midfoot fracture,146 particularly those of the navicular tuberosity. MRI can be helpful in the evaluation of midfoot tendon and ligamentous injuries.147 Undisplaced injuries may heal with casting, but operative fixation is often required and management can be difficult.148 Complications are common and include persistent pain, arthritis, and long-term disability.
Midfoot Injuries
Principles of Disease: Anatomy.: The navicular has a curved shape—hence the derivation of its name from the Latin word navis, meaning “ship.” Because of the navicular’s extensive articular surface, its blood supply can enter only through a small waist of cortex, and the middle third is relatively avascular. As a result, the navicular is at particular risk for avascular necrosis after fractures, analogous to its counterpart in the wrist, the scaphoid bone.149
Pathophysiology.: Navicular fractures, although relatively rare, are the most common midfoot fracture and are classified into dorsal avulsion fractures, tuberosity fractures, and body fractures. Dorsal avulsion fractures account for one half of navicular fractures and usually occur when an eversion stress causes bony avulsion from either the talonavicular capsule or the deltoid ligament. These fractures usually do not involve a significant amount of articular surface. Tuberosity fractures also occur from eversion forces, leading to an avulsion at the insertion of the posterior tibial tendon. A tuberosity fracture may be the only clue to the presence of a midtarsal joint injury. Body fractures are uncommon and result from an axial loading mechanism. They often are comminuted, intra-articular, and associated with other midtarsal pathologic conditions. Stress fractures of the navicular can also occur.
Clinical Features.: Navicular fractures cause localized tenderness over the dorsal and medial aspects of the midfoot. The navicular tuberosity may be tender and is located by first identifying the sustentaculum tali, a shelf of bone on the medial aspect of the ankle approximately 2.5 cm below the tip of the medial malleolus. The tuberosity is then easily palpable just anterior to this landmark. In the case of tuberosity fractures, pain may be exacerbated by passive eversion or active inversion of the foot.
Diagnostic Strategies: Radiology.: Standard foot radiographs usually demonstrate navicular fractures; however, CT or MRI may be required. Care is taken not to confuse the commonly occurring os tibiale externum, also called an accessory navicular bone, with an acute fracture (see Fig. 58-15).
Management.: Dorsal avulsion and tuberosity fractures not involving a significant amount of articular surface are usually treated with a walking cast for 4 to 6 weeks. Body fractures and displaced fractures involving more than 20% of the articular surface often require operative fixation.
Disposition.: Most navicular fractures are suitable for outpatient orthopedic follow-up; however, significant fractures, particularly if intra-articular, warrant orthopedic consultation in the ED. Navicular tuberosity fractures can be complicated by nonunion. Avascular necrosis and arthritis, particularly in body or other intra-articular fractures, are potential late sequelae.
Cuboid Fractures: Isolated cuboid fractures are uncommon and usually result from lateral subluxation of the midtarsal joint in Lisfranc’s injury. Cuboid fracture has been termed a nutcracker fracture because the cuboid is crushed between the bases of the fourth and fifth metatarsals and the anterior calcaneus.150 These fractures are also associated with fractures of the posterior malleolus.
The cuboid is best evaluated by the oblique view of a standard foot radiographic series because this demonstrates both the calcaneocuboid and the cuboid-metatarsal relationship. The possibility of Lisfranc’s injury should be considered with any cuboid fracture. Treatment of isolated injuries ranges from casting for minor nondisplaced fractures to operative fixation.151 Extra-articular cuboid fractures can lead to serious disability from dysfunction of the peroneus longus tendon at the level of the peroneal groove. All cuboid fractures warrant orthopedic assessment.
Cuneiform Fractures: Fractures of the cuneiforms are extremely uncommon and usually result from direct trauma. As with cuboid fractures, the patient should be assessed carefully for the presence of Lisfranc’s injury. Treatment usually is by casting; however, displaced fractures require orthopedic assessment.
Dislocations of the Navicular, Cuboid, and Cuneiforms: Isolated dislocations of each of the midfoot bones have been described. These are uncommon injuries that often require open reduction. Orthopedic consultation in the ED is required for any of these injuries.
Lisfranc (Tarsometatarsal) Fractures and Dislocations:
Principles of Disease: Anatomy.: Collectively, the tarsometatarsal joints (see Fig. 58-14) are commonly called Lisfranc‘s joint. Any injury to this area, whether sprain, dislocation, or fracture-dislocation, is termed a Lisfranc injury. Knowledge of the anatomy of the Lisfranc joint complex is central to an understanding of these injuries.
Pathophysiology.: Lisfranc injuries are uncommon, in part because tremendous energy is often required to disrupt this complex. Such injuries arise from three mechanisms: rotational forces, whereby the body twists around a fixed forefoot; axial loads, whereby the weight of the body drives the hindfoot into the bases of the metatarsals; and crush injuries. Because of the mechanisms involved, associated injuries, such as MTP joint dislocations, can occur. Most Lisfranc injuries are incurred in MVCs. Sports involving fixation of the forefoot (e.g., equestrian activities and windsurfing) also are associated with these injuries. Of note, one third of Lisfranc ligamentous injuries arise from seemingly trivial mechanisms such as stumbles or falls. Most Lisfranc injuries are closed.
Numerous classifications for displaced Lisfranc injuries exist, none of which aids in determining appropriate treatment or outcome.152 The most intuitive classification categorizes the direction of the dislocation in the horizontal plane (Fig. 58-23).153–155 In homolateral injuries, all five metatarsals are displaced in the same direction. In isolated injuries, one or more metatarsals are displaced away from the others. In divergent injuries, the metatarsals are splayed outward in both the medial and the lateral directions. These injuries usually occur between the first and second metatarsals because of their lack of an intermetatarsal connection. A component of dorsal displacement also is commonly present in displaced Lisfranc injuries, whereas plantar displacement is uncommon because of the joint’s bone architecture and the strength of the plantar ligaments and fascia.
Clinical Features.: Most Lisfranc injuries are clinically obvious; however, findings may be subtle, and the true extent of the pathologic condition can easily be missed or misdiagnosed.156 Apparently trivial fractures, if viewed in isolation, fail to reflect the serious soft tissue disruption that can be present. Some estimate that the diagnosis is missed on initial ED presentation in up to 20% of cases.157–159
Diagnostic Strategies: Radiology.: Standard radiographic views of the foot usually are sufficient to diagnose injuries to the Lisfranc complex, although findings may be subtle (Fig. 58-24). The anteroposterior view identifies fractures and alignment, with the oblique view greatly aiding this assessment by eliminating overlap at the metatarsal bases. The lateral view shows the soft tissues and identifies any dorsal or plantar displacement. Weight-bearing (stress) radiographs may be helpful in uncertain cases,157 and, although poorly studied, it has been suggested that up to 10% of Lisfranc injuries are undetectable without stress views.160 In situations in which pain precludes weightbearing, regional anesthesia may facilitate obtaining weight-bearing radiographs. Comparison views are extremely helpful, and a 30-degree oblique view, in addition to the standard 45-degree oblique view, also may be of value. As is the case elsewhere in the hindfoot and midfoot, CT scanning has revolutionized the diagnosis and evaluation of Lisfranc injuries.161 Because of its ability to image ligamentous structures, MRI may be useful to predict Lisfranc joint complex instability.162
Management.: Lisfranc injuries usually are treated with closed reduction and internal fixation with percutaneous Kirschner wires. This is followed by non–weight-bearing casting for 12 weeks and wearing of an orthotic for 1 year. Treatment of a sprain of the Lisfranc complex usually involves immobilization for 6 weeks in a below-knee walking cast.
Disposition.: Any obvious or suspected Lisfranc injury requires orthopedic consultation in the ED. Patients suspected of having a sprain of the Lisfranc complex require casting and orthopedic assessment on an outpatient basis, because operative fixation can be required. The incidence of complications with a Lisfranc injury depends on the timing of diagnosis and the degree of anatomic reduction achieved. Aggressive surgical management clearly improves outcome.
Delayed treatment or missed diagnosis of Lisfranc injuries can result in significant complications.163 Degenerative arthritis is a common complication. Other potential complications include compartment syndrome, residual pain, unequal metatarsal pressure, loss of the metatarsal arch, and complex regional pain syndrome. Unstable sprains of the Lisfranc complex can result in biomechanical problems if untreated, and delayed presentations pose management challenges and often result in complications.164
Forefoot Injuries
Metatarsal Fractures: Metatarsal fractures are common and account for one third of foot fractures. The best approach is first to classify the injury anatomically as occurring in the shaft, the head and neck, or the base. Management is then dictated by the metatarsal involved, the specific location and type of fracture, and the nature of any associated injuries.165,166
Principles of Disease: Pathophysiology.: Metatarsal shaft fractures arise from either direct trauma (e.g., a crush injury from a heavy object) or indirect trauma (e.g., a twisting force applied to a fixed forefoot). Because of the nature of the mechanism of injury, associated phalangeal fractures often occur. Direct trauma may be highly disruptive, resulting in multiple metatarsal fractures and severe complications. The third metatarsal is the most commonly fractured, and metatarsal shaft stress fractures are common.
Clinical Features.: Metatarsal shaft fractures cause weight-bearing difficulty and tenderness, which usually is maximal on the plantar surface and can be difficult to localize if swelling is significant. Axial compression of the involved toe often is painful, and ecchymosis usually appears within 12 hours of injury. Rotational alignment should be assessed by evaluating the position and plane of the involved digit.
Diagnostic Strategies: Radiology.: Standard radiographs are sufficient to diagnose most metatarsal shaft fractures; however, radiographs usually are exposed for visualization of the talar bones, and the forefoot may be overpenetrated. Adjustment of penetration or coned views may be required for visualization of subtle fractures. Displacement and angulation, in both the sagittal and mediolateral planes, should be assessed.
Management.: Most undisplaced metatarsal shaft fractures of the second through fifth metatarsals are treated with a below-knee walking cast for 2 to 4 weeks. Early casted ambulation may be beneficial to healing and may reduce the incidence of complex regional pain syndrome. Although some practitioners recommend a non–weight-bearing cast for 4 to 6 weeks for these fractures, others suggest that a metatarsal pad, stiff shoes, and crutches, if needed, are sufficient. These various approaches attest to the fact that most nondisplaced metatarsal shaft fractures heal well regardless of the treatment.
The great toe metatarsal requires more aggressive management because of its biomechanical role and the stresses imposed on it during gait. Nondisplaced first metatarsal fractures should be treated with casting for 4 to 6 weeks.167 For at least the first 3 weeks of this immobilization, if not the entire period, the patient should not bear weight.
Reduction should be considered in any metatarsal shaft fracture with more than 3 mm of displacement or 10 degrees of angulation. Closed reduction, with toe traps and countertraction at the ankle, is often successful. Non–weight-bearing casting for 4 to 6 weeks should follow. The indications for open reduction are controversial but generally include the presence of compartment syndrome, unstable fractures, open fractures, fractures that have failed closed reduction, and multiple fractures. These are treated with fixation with either Kirschner wires or plates.167 In particular, displaced first and fifth metatarsal shaft fractures are commonly treated operatively. Major forefoot trauma, with crushing and multiple open metatarsal fractures, requires an aggressive approach with staged operative management.
Disposition.: Most undisplaced metatarsal shaft fractures are suitable for management without orthopedic referral. Orthopedic consultation in the ED should be obtained for patients with multiple or displaced fractures. Complications are rare in nondisplaced or minimally displaced metatarsal shaft fractures. Complex regional pain syndrome can occur and may be related to the unnecessary use of non–weight-bearing casting. Inadequate reduction, particularly in the sagittal plane, can lead to biomechanical problems and formation of painful callosities or metatarsalgia. Malunion in the mediolateral plane, particularly if involving the first or fifth metatarsal, can lead to development of pressure points, neuromas, or biomechanical problems. Delayed union, nonunion, compartment syndrome, and soft tissue complications occur uncommonly.
Metatarsal Head and Neck Fractures: Metatarsal head and neck fractures, although similar in their pathophysiology and assessment to shaft fractures, commonly are multiple and often result from direct trauma. Nondisplaced fractures may be treated with a walking cast for 4 to 6 weeks. Often these fractures are displaced, with the distal fragment pulled in a plantar and lateral direction by the flexor tendons, a finding best appreciated on oblique and lateral radiographic views. Precise realignment of neck and head fractures is important to maintain the transverse arch. Although reduction may be successful with toe traps, instability is common, and operative fixation is required more commonly than with shaft fractures. Most of these fractures warrant orthopedic consultation in the ED, particularly if they are displaced or intra-articular. Complications are similar to those seen with shaft fractures.
Principles of Disease: Pathophysiology.: Isolated fractures of the first through fourth metatarsal bases are uncommon. Most are nondisplaced transverse fractures within 1 cm of the tarsometatarsal articulation and arise as a result of direct trauma. An indirect mechanism is more suggestive of the presence of an occult Lisfranc injury. The most commonly encountered metatarsal base fractures occur at the fifth metatarsal.
Fifth Metatarsal.: Jones fracture is a term often erroneously applied to any fracture of the fifth metatarsal base. The eponym is in reference to Sir Robert Jones, a physician who in 1902 described a fracture he sustained while dancing and a series of similar injuries. In reality, two distinct acute fractures can occur in the region of the fifth metatarsal base, and debate continues regarding which one Jones actually described.168 More important than the terminology, these two fractures differ dramatically in their mechanism, treatment, and prognosis.169
The more common, and benign, fracture at the fifth metatarsal base is of the tuberosity. Also called the styloid, the tuberosity is the bulge of the fifth metatarsal that is easily palpated over the lateral edge of the foot. It is fractured by a sudden inversion of a plantar-flexed foot. For decades, this fracture was thought to be caused by an avulsion at the insertion of the peroneus brevis tendon; however, it is now known that the plantar aponeurosis is responsible for the location and nature of this fracture.170
Tuberosity fractures range from tiny flecks to lesions involving the entire tuberosity and usually are extra-articular, although they may extend into the cubometatarsal joint. Often these injuries masquerade as ankle sprains (see Fig. 58-12 and Box 58-2), making the fifth metatarsal base an important area to palpate in any twisting injury.
The more serious acute fracture at the base of the fifth metatarsal is a transverse fracture occurring at least 15 mm distal to the proximal end of the bone.169 This diaphyseal fracture probably is a true Jones fracture and involves the fourth and fifth intermetatarsal articulations but not the cubometatarsal articulation. Diaphyseal fractures result from a complex combination of forces generated when a load is applied to the lateral forefoot in the absence of inversion.169 Typically these occur in running and jumping sports. Further subclassification schemes of proximal diaphyseal fractures exist and can be helpful in determining management.152 Fifth metatarsal diaphyseal stress fractures can also occur and should be considered when a seemingly acute injury is preceded by a prodrome of pain in the region over weeks to months.152,166
Clinical Features.: The assessment of metatarsal base fractures is similar to that described for fractures of the metatarsal shaft. Pain often is diffuse and difficult to localize in these injuries, with the exception of the easily palpable fifth metatarsal tuberosity. Passive inversion also may be painful with a fifth metatarsal base fracture.
Diagnostic Strategies: Radiology.: Standard radiographic views easily demonstrate most metatarsal base fractures. Radiographs should be carefully assessed for fracture angulation, displacement, and articular extension. If the fracture is intra-articular, an estimation of the percentage of articular surface involved is essential in determining management. In difficult cases, CT studies may be helpful.
With fractures of the first through fourth metatarsal bases, it is important to search for other radiologic clues to a Lisfranc injury. A fracture of the second metatarsal base is virtually pathognomonic for occult tarsometatarsal joint disruption. In assessment for a fifth metatarsal base fracture, differentiation between the tuberosity and diaphysis is essential (Fig. 58-25). Care should be taken not to misinterpret an os vesalianum or os peroneum for a fifth metatarsal base fracture (see Fig. 58-15). Standard ankle radiographs also demonstrate the fifth metatarsal base, and this area should be routinely scrutinized.
Management.: Nondisplaced extra-articular fractures of the first through fourth metatarsal bases usually are managed with a below-knee cast. Displaced fractures should be reduced and often require fixation. Intra-articular fractures, especially those of the first metatarsal, often lead to complications. Operative fixation may be required, even in nondisplaced intra-articular first metatarsal base fractures, if more than 25% of the articular surface is involved.
The management of fifth metatarsal base fractures depends on the type of fracture. Extra-articular tuberosity fractures, regardless of their size or degree of displacement, heal well and are managed symptomatically with a walking cast for 2 to 3 weeks, compression wrap, or stiff shoes.168 Intra-articular tuberosity fractures involving more than 30% of the articular surface, or with more than 2 mm of displacement, may require fixation.168 Nondisplaced intra-articular fractures usually are treated initially with non–weight-bearing casting for 6 to 8 weeks, followed by radiographic reassessment.168 Immobilization for up to 6 months may be required for complete healing, and immediate fixation may be advisable in athletes.169 Displaced fifth metatarsal diaphyseal fractures usually are managed operatively,171 and prolonged treatment may be necessary particularly for diaphyseal stress fractures.
Disposition.: Because they are rare and treatment varies, most first through fourth metatarsal base fractures require orthopedic assessment. Nondisplaced extra-articular fractures of the first through fourth metatarsal bases are suitable for orthopedic follow-up on an outpatient basis. Orthopedic consultation in the ED should be obtained in any other first through fourth metatarsal base fracture or if Lisfranc’s injury is suspected. Significant or displaced intra-articular fifth metatarsal tuberosity fractures or diaphyseal fractures warrant orthopedic evaluation in the ED.
Principles of Disease: Pathophysiology.: Phalangeal fractures are the most common forefoot fracture. They usually arise from direct trauma, often the result of dropped heavy objects or stubbing the toe. Less commonly, indirect mechanisms involving twisting of the forefoot can lead to phalangeal fractures. Proximal phalanges are more commonly fractured than middle or distal phalanges, and the proximal phalanx of the fifth toe is most commonly injured. Fractures of the hallux often are displaced, whereas fractures of the lesser phalanges are often comminuted but less commonly displaced.
Clinical Features.: Although phalangeal fractures generally are considered minor injuries, they can lead to disabling sequelae and merit careful assessment.172 The patient with a phalangeal fracture has acute pain and swelling of the affected toe, often with difficulty ambulating or wearing shoes. Examination may reveal tenderness, crepitus, and reduced range of motion. A subungual hematoma often is present if the distal phalanx is involved, and open fractures are common.
Diagnostic Strategies: Radiology.: Standard radiographic views usually are sufficient to demonstrate phalangeal fractures, with the lateral view being most sensitive. Often the uninjured toes must be positioned out of the way for adequate radiographs to be obtained, and magnification radiographs occasionally are required. Angulation and joint involvement should be assessed.
Management.: Most phalangeal fractures are easily managed and heal well. Large and symptomatic subungual hematomas should be evacuated, and, on rare occasions, nail bed repair may be required. Nondisplaced lesser phalangeal fractures should be stabilized by “buddy-taping”—splinting the injured toe to an adjacent, ideally longer, toe with adhesive tape. Placement of gauze between the splinted toes is advisable to prevent skin maceration. Phalangeal fractures often remain painful for 2 to 3 weeks until stabilized by callus.
Nondisplaced phalangeal fractures involving the hallux are treated by buddy-taping, with a walking cast worn for 2 to 3 weeks if the toe is painful. Alternatives to standard casting techniques, such as the slipper cast, have also been described for phalangeal fractures.173 Displaced phalangeal fractures of the hallux require reduction. If the reduction is inadequate or unstable, operative fixation may be indicated. Unless completely nondisplaced, most intra-articular fractures involving the hallux are treated with operative fixation, although this is an area of controversy.
Sesamoid Fractures: The sesamoids are two flat oval bones found within the tendon of the flexor hallucis brevis, under the head of the first metatarsal. Their name comes from the Greek word sesamoeides, meaning “resembling a sesame seed.” Ten percent of the population has sesamoid bones under the fifth metatarsal head, and uncommonly, sesamoids are found under the second, third, or fourth metatarsal (see Fig. 58-15). Sesamoid fractures are uncommon and usually are caused by direct trauma from falls. Hyperextension of the great toe can indirectly lead to a sesamoid fracture.174 Sesamoid fractures also can be found in association with MTP joint dislocations. The medial sesamoid of the great toe is more commonly fractured than the lateral, and a suspected fracture should be differentiated from a bipartite sesamoid, which occurs in up to one third of the population and also is more common on the medial aspect. Stress fractures of the sesamoids also occur. Sesamoid fractures generally require a below-knee walking cast for 3 to 4 weeks. Most heal without complications and do not require orthopedic consultation.
Metatarsophalangeal Dislocations:
Principles of Disease: Pathophysiology.: Dislocations of the MTP joint are uncommon injuries because of the protection footwear provides and the inherent stability of MTP and IP joints. MTP joint dislocations can occur in any joint and in any direction. First MTP joint dislocations require large forces and usually result from MVCs. These injuries often are open and typically involve dorsal dislocations of the distal component caused by hyperextension of the MTP joint. Associated sesamoid fractures may be present. Complex dislocations, in which the sesamoids or local tendons prevent closed reduction, can occur. Second through fifth MTP dislocations usually are medial or lateral displacements that occur when the toe strikes or hooks an object. The most common is a lateral dislocation of the fifth MTP joint.
Clinical Features.: Dislocations of the MTP joint cause pain, swelling, and difficulty bearing weight on the ball of the foot. First MTP joint dislocations usually are obvious on clinical examination because the toe is angled upward with dorsal and proximal displacement of the proximal phalanx. This deformity leads to a striking prominence of the metatarsal head over the plantar surface. Skin tenting or a dimple may be present. Rarely the sesamoids are palpable dorsal to the metatarsal, indicating a complex dislocation. Dislocations of the lesser toes often are more subtle in presentation, and comparison with the uninjured foot may be helpful. Neurovascular compromise is rare.
Diagnostic Strategies: Radiology.: Dislocations of the MTP joint are well visualized on standard radiographic views of the foot. In first MTP joint dislocations, a double density often is present, caused by superimposition of the base of the proximal phalanx over the metatarsal head. Radiographs should be scrutinized for signs suggesting complex dislocation, such as the sesamoids lying between the two articular surfaces or dorsal to the metatarsal head.
Management.: Most MTP joint dislocations, particularly of the lesser toes, are easily reduced with longitudinal traction. Appropriate analgesia or local anesthesia should be administered before reduction is attempted. Dorsal dislocations of the first MTP joint can be more challenging and may require initial accentuation of the deformity in addition to longitudinal traction for reduction. Joint stability should be assessed and repeat radiographs obtained after reduction of an MTP joint dislocation. After reduction, a walking cast with a toe plate is worn for 3 weeks, followed by physiotherapy to ensure adequate range of motion. Alternatively, buddy-taping and an aluminum splint can be used for immobilization.
Disposition.: Most MTP joint dislocations can be managed without orthopedic consultation. If crepitus or obvious instability is present or postreduction radiographs show joint incongruity or an intra-articular fracture, orthopedic consultation should be obtained for possible fixation. First MTP joint dislocations that are open, show radiographic evidence of complexity, or do not easily reduce require orthopedic consultation in the ED, because open reduction may be required. Very rarely, MTP joint dislocations of the lesser toes require open reduction.
Interphalangeal Joint Dislocations: IP joint dislocations are much less common than MTP joint dislocations and are sometimes overlooked. Most IP joint dislocations occur in the great toe and are a result of axial loading. IP joint dislocations usually involve dorsal displacement of the distal component and are easily managed without orthopedic consultation. Reduction is performed with longitudinal traction after digital block anesthesia is achieved. Initial accentuation of the deformity may be necessary if reduction is unsuccessful with simple traction. If the dislocation involves the great toe, a walking cast with a toe plate for 3 weeks is indicated after reduction. Lesser toes require only buddy-taping. As with the MTP joint, complex dislocations involving the first IP joint can occur, and orthopedic consultation in the ED for open reduction may be necessary. Very rarely, lesser toe IP joint dislocations are irreducible with closed methods and will require open reduction.
Perspective.: Foot pain, particularly in the absence of obvious trauma, poses a diagnostic and therapeutic challenge. Plain radiographs commonly are normal in appearance, so the history and physical examination assume increased importance. Although a definitive diagnosis often is difficult to obtain in the ED, a structured approach aids in appropriate patient management and disposition. Most causes of foot pain are minor and self-limited, but the possibility of serious pathologic conditions (e.g., infection, arthritis, tumor) should be considered. Although orthopedic consultation in the ED is rarely required, orthopedic or sports medicine follow-up on an outpatient basis is indicated for selected cases.
Hindfoot Pain.: Hindfoot pain is a common complaint that usually is the result of overuse rather than acute trauma.175 Bone pain in the hindfoot necessitates consideration of talar or calcaneal stress fractures. A calcaneal stress fracture may be suspected when pain is elicited on squeezing the calcaneus mediolaterally. Another cause of bone pain is impingement by an os trigonum (see Fig. 58-15) or prominent lateral posterior talar process. The os trigonum syndrome involves pain during plantar flexion of the foot and is particularly common in ballet dancers. A bone scan may be required for diagnosis, and treatment is surgical.
Most patients with hindfoot pain describe subcalcaneal heel pain, a complaint with an extensive differential diagnosis.176 The literature on this topic is conflicting and fraught with inconsistent terminology. The most common causes of subcalcaneal pain are plantar fasciitis, subcalcaneal bursitis, acute rupture of the plantar fascia, and nerve compression.
The plantar fascia is a tough layer of the sole that is functionally significant during foot strike and the early stance phase of walking. Plantar fasciitis, an overuse injury of insidious onset, usually begins with pain on first weightbearing in the morning or after prolonged sitting.177 This progresses to persistent pain during gait. Pain and tenderness are localized to the medial aspect of the heel. Plantar fasciitis is particularly common in cavus feet, although the nature of this association is unclear.178 Plain radiography is not diagnostic but shows a calcaneal spur in 50% of patients with plantar fasciitis. This is a stress-related ossification with a 16% incidence in asymptomatic persons and is not considered the primary cause of pain in plantar fasciitis. Rarely, fascial ossification (an os subcalcis) may be seen.
Plantar fasciitis is distinct from subcalcaneal bursitis, a condition with an identical presentation in which the pain is localized to the bursa directly below the calcaneus. Differentiating these two conditions can be difficult and usually is academic, because initial treatment is identical: a combination of avoiding precipitating conditions, rest, padding, orthotics, nonsteroidal anti-inflammatory drugs, and occasionally steroid injections. Extracorporeal shock wave therapy can be beneficial in refractory cases.179 Very rarely, surgical release of the plantar fascia is required, a therapy that can be beneficial in either condition.
Compression of either the abductor digiti quinti nerve or the posterior tibial nerve (the so-called “tarsal tunnel syndrome”) can cause subcalcaneal heel pain.180 Diagnosis of these conditions is difficult and is sometimes facilitated by assessing the impact of selective nerve block with local anesthesia. Initial treatment of these conditions is similar to that for plantar fasciitis, although local steroid injections or surgical release may be required. Other nerve entrapments also can occur in the hindfoot area.
Midfoot Pain.: Isolated midfoot pain is less common than forefoot or hindfoot pain. Stress fractures are uncommon in the midfoot and most commonly involve the navicular. Other causes of midfoot pain include symptomatic accessory bones, particularly the accessory navicular, os tibiale externum, and os peroneum (see Fig. 58-15). An os tibiale externum is present in up to 14% of the normal population and is asymptomatic in most cases. This accessory bone can produce debilitating pain on the medial aspect of the midfoot. A bone scan facilitates diagnosis, and surgical excision may be necessary. An os peroneum is one of several conditions that can cause lateral plantar pain in the midfoot region. Localization of tenderness is aided by resisted plantar flexion, and treatment ranges from immobilization to surgical excision.
Forefoot Pain.: The forefoot is the site for a myriad of painful problems. Bunions, painful bursae, blisters, corns, calluses, hammertoes, and ingrown toenails all are diagnostically obvious but can pose therapeutic challenges. Many are the result of poor footwear or a biomechanical problem with the foot and respond to appropriate padding, avoidance of precipitants, and occasionally surgical intervention.
Metatarsalgia is an often used, although loosely defined, term referring to pain in the region of the metatarsal heads.181 This is a common presenting complaint with many potential causes. Metatarsal stress fractures are extremely common and should be considered in the differential diagnosis for any unexplained forefoot pain. Flexor or extensor tendinitis also can produce metatarsal area pain and is suggested when plain radiographs show areas of tendinous calcification. Arthritis, sesamoiditis, or a sesamoid stress fracture should be considered when pain occurs in the area of the hallux. “Turf toe” is MTP joint inflammation of the hallux resulting from repeated hyperextension stress.117 It usually responds to symptomatic measures but can be a significant and debilitating injury in some athletes, such as football players.
An important cause of unilateral metatarsalgia is a perineural fibrosis of the intermetatarsal plantar digital nerve, more commonly known as Morton‘s neuroma.181 This neuropathy of unknown cause was first described in 1876 and usually involves the second-third or third-fourth intermetatarsal space, causing lancinating pain with weightbearing. The pain may be associated with paresthesias and can radiate into the toes. In addition, “afterburn” pain can persist during rest. The pain of Morton’s neuroma is reproduced when structures of the affected interspace are pinched or when the metatarsal heads are compressed together. Hence, pain may occur intermittently with tight-fitting footwear (e.g., rock-climbing shoes, ski boots). Crepitus or a nodule may be palpable. Initial treatment usually involves a metatarsal pad and the use of shoes with a widened toe box. Surgical excision or neurolysis may be required if conservative management is unsuccessful.182
Freiberg‘s disease is an osteochondrosis of the metatarsal head, usually involving the second metatarsal, and is another cause of pain in this area. Ingrown toenails are a common affliction that can occur in any toe, most commonly the hallux. Often the abnormality is perpetuated by short nail trimming, which affords the opportunity for a spicule of nail to grow under the nail fold.183 Allowing the nail to grow out and providing local care usually will lead to resolution of the condition. Antibiotics are indicated if infection is present. Chronic or recurring ingrowth necessitates partial or complete excision of the nail and germinal ablation.183
Special Considerations
Principles of Disease: Pathophysiology: Stress fractures can occur anywhere in the appendicular skeleton but are particularly common in the lower extremity. Athletic activities, particularly running, account for most stress fractures. Predisposing factors include training errors, poor footwear, a previous period of inactivity, change in running surface, and the “female athlete triad” of disordered eating, menstrual disturbances, and low bone mineral density.184 Anatomic variations may play a role, with cavus feet being more prone to stress fractures than flat feet.
Clinical Features: Although the history is variable, most stress fractures produce localized pain of insidious onset, usually with aching over a period of weeks.185 The pain may be anywhere in the hindfoot, midfoot, or forefoot but is most common along a metatarsal. Initially symptoms occur after athletic activities, but later they limit such activities. Often a predisposing factor, such as a training regimen change, is present. A menstrual history should be obtained in female patients because amenorrhea, often a result of training, can predispose to stress fractures.185–187
Diagnostic Strategies: Radiology: Initial plain radiographs are commonly normal because bone reaction in stress fractures depends on the length of time from symptom onset. Radiographic abnormalities in the metaphyses can take up to 4 weeks to develop, and those in the diaphyses can take 6 weeks.25 Although plain radiographs have low sensitivity for stress fractures, their specificity is high. The three important findings are periosteal new bone, endosteal thickening, or a radiolucent line. Radiographic findings vary with location: Metatarsal fractures usually show callus or periosteal reaction, whereas navicular fractures show a lucent line, and calcaneal fractures show curvilinear sclerosis.
The diagnosis of a stress fracture is easily missed because only 50% of patients develop plain radiographic abnormalities. Until recently, radionuclide bone scanning was the imaging modality of choice for stress fractures. Bone scans are nonspecific but extremely sensitive for stress fractures, usually showing abnormal uptake within 24 hours of injury. Rarely, a bone scan may be falsely negative if pain occurs before the onset of a demonstrable pathologic condition. MRI scanning has been found to be equally sensitive and more specific and has emerged as the imaging modality of choice for the outpatient evaluation of this condition.25,115
Management: Athletic stress fractures are overuse injuries and necessitate an evaluation of training habits, equipment, and techniques. Most pedal stress fractures resolve in 4 to 6 weeks simply with limitation of impact activities and do not require immobilization unless symptoms are severe. Two locations, however, are unique and deserve specific discussion.
Navicular stress fractures are uncommon and often delayed in diagnosis. Healing is hampered by the relative avascularity of the middle third of the bone, and initial treatment is with non–weight-bearing casting for 6 to 8 weeks. Stress fractures of the fifth metatarsal base are also problematic. Fifth metatarsal diaphyseal stress fractures (also called chronic Jones fractures) are usually initially treated with non–weight-bearing status and casting. As with acute diaphyseal fractures, delayed healing is common, and casting for up to 20 weeks may be required.168
Disposition: Any patient diagnosed with or suspected of having a stress fracture should undergo orthopedic or sports medicine follow-up on an outpatient basis. Delayed union or nonunion can occur with stress fractures, particularly those of the navicular or fifth metatarsal base. Bone grafting or hardware fixation may be required. Most other pedal stress fractures heal without complications.
Contusions and Sprains
Tendon Injuries: Acute tendon ruptures in the foot, apart from the Achilles and posterior tibial tendons, are rare. Although isolated ruptures of the flexor hallucis longus and anterior tibial tendons have been described, most tendon transections are the result of lacerations. These typically arise from one of two mechanisms: penetrating wounds to the sole of the foot or major trauma from such sources as dropped objects, lawn mowers, or MVCs. Plantar penetrating trauma usually results in flexor tendon injuries, whereas most major mechanisms involve extensor tendons.
Crush Injuries, Amputations, and Major Vascular Injuries
Rapid assessment, stabilization, and immediate consultation are priorities in the ED management of a major crush injury, amputation, or vascular injury of the foot. The injured limb is handled gently and can be irrigated with sterile saline solution to remove debris. Use of other irrigating solutions, exploration, or débridement, even if done carefully, is contraindicated.188 Antibiotics should be administered, as with any open fracture. Compartment syndrome should be considered in crush injuries. Many factors enter into surgical decision-making for patients with such injuries,189 and objective measures, such as the “mangled extremity score,” have been developed to predict the need for amputation.190 Local crush injuries often heal better than diffuse crush injuries.188 A surgical goal is preservation of as much length as possible to maintain a longitudinal arch, and care plans are typically individualized.191 In the presence of a major vascular injury, the likelihood of permanent disability is high.
Compartment Syndrome
Principles of Disease: Pathophysiology: Compartment syndrome is defined as an increase in pressure within a confined osseofascial space that impedes neurovascular function, resulting in tissue damage.188 Compartment syndrome in the foot, as elsewhere in the body, constitutes a medical emergency. Classically, four foot compartments—medial, central, lateral, and interosseous—are described, although studies using dye injection have suggested that there may be as many as nine foot compartments.188
Pedal compartment syndrome is most commonly caused by significant crush injuries, fractures, or dislocations. Other causes include bleeding disorders, burns, electrical injury, postischemic swelling after arterial injury or thrombosis, drug or alcohol overdose, excessive exercise, and venous obstruction.37 Pedal compartment syndrome after an ankle sprain has also been reported.192 Damage is related to the duration and magnitude of compartment pressure rise and the arteriovenous gradient. Compartment syndrome can develop anywhere from 2 hours to 6 days after an insult, although the peak incidence is at 15 to 30 hours.
Clinical Features: Compartment syndrome typically causes pain out of proportion to that expected for the injury. The pain is not decreased by immobilization and can be described as a feeling of tautness within the foot.193 In the case of calcaneal fractures, the pain often is a relentless burning involving the entire foot. Physical examination may reveal tense swelling and sensory deficits. Pain is exacerbated by any movement (active or passive) that stretches the muscles of the involved compartment. Passive dorsiflexion of the toes often is painful. Peripheral pulses and capillary refill usually are normal in compartment syndrome and thus offer no reassurance when present. Presence of an open wound does not guarantee that all compartments are decompressed.
Diagnostic Strategies: Special Procedures: The only way to diagnose a compartment syndrome is to measure intracompartmental pressure. The decision to perform this maneuver relies on appropriate clinical suspicion. Techniques of pressure measurement are well described, with a pressure greater than 30 mm Hg generally considered diagnostic.193,194 Compartment syndrome can occur at lower pressures in hypotensive patients. More details on the pathophysiology and diagnosis of this condition can be found in Chapter 49. The needle localization and distinguishing of foot compartments is challenging because of their small size. For this reason and because of its importance in surgical decision-making, measurement of pedal compartment pressures usually should be left to an orthopedic surgeon.
Management: Early identification and prevention of further tissue damage are important considerations in any patient with a mechanism consistent with the development of compartment syndrome. Circumferential bandages and casts should be avoided during early management. In diagnosed or suspected cases of compartment syndrome, the limb should be positioned at the level of the heart. Limb elevation beyond this point is contraindicated because it would decrease arterial flow, thereby narrowing the arterial-venous pressure gradient.
References
1. Grimston, SK, Nigg, BM, Hanley, DA, Engsberg, JR. Differences in ankle joint complex range of motion as a function of age. Foot Ankle. 1993;14:215.
2. Simon RR, Sherman SC, Koenigsknecht SJ, eds. Emergency Orthopedics: The Extremities, 5th ed, New York: McGraw-Hill, 2007.
3. Stiell, IG, et al. Implementation of the Ottawa Ankle Rules. JAMA. 1994;271:827.
4. Davidovitch, RI, Egol, KA. Ankle fractures. In: Bucholz RW, Court-Brown CM, Heckman JD Tornetta P, eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott: Williams & Wilkins; 2010:1973.
5. Brandser, EA, et al. Missed fractures on emergency room ankle radiographs: An analysis of 433 patients. Emerg Radiol. 1997.
6. Yu, JS, Cody, ME. A template approach for detecting fractures in adults sustaining low-energy ankle trauma. Emerg Radiol. 2009;16:309.
7. Ho, K, Connell, DG, Janzen, DL, Grunfeld, A, Clark, TW. Using tomography to diagnose occult ankle fractures. Ann Emerg Med. 1996;27:600.
8. Stiehl, JB. Ankle fractures with diastasis. Instr Course Lect. 1990;39:95.
9. Bachmann, LM, Kolb, E, Koller, MT, Steurer, J, ter Riet, G. Accuracy of Ottawa Ankle Rules to exclude fractures of the ankle and mid foot: Systematic review. BMJ. 2003;326:1.
10. Plint, AC, et al. Validation of the Ottawa Ankle Rules in children with ankle injuries. Acad Emerg Med. 1999;6:1005.
11. Libetta, C, Burke, D, Brennan, P, Yassa, J. Validation of the Ottawa Ankle Rules in children. Pediatr Emerg Care. 1999;19:73.
12. Boutis, K, et al. Sensitivity of a clinical examination to predict need for radiography in children with ankle injuries: A prospective study. Lancet. 2001;358:2118.
13. Yuen, MC, Saunders, F. Towards evidence based emergency medicine: Best BETs from the Manchester Royal Infirmary. The Ottawa Ankle Rules in children. Emerg Med J. 2001;18:466.
14. Karpas, A, Hennes, H, Walsh-Kelly, CM. Utilization of the Ottawa Ankle Rules by nurses in a pediatric emergency department. Acad Emerg Med. 2002;9:130.
15. Clark, KD, Tanner, S. Evaluation of the Ottawa Ankle Rules in children. Pediatr Emerg Care. 2003;19:73.
16. Dayan, PS, et al. Derivation of clinical prediction rules to identify children with fractures after twisting injures of the ankle. Acad Emerg Med. 2004;11:736.
17. Gravel, J, Hedrei, P, Grimard, G, Gouin, S. Prospective validation and head-to-head comparison of 3 ankle rules in a pediatric population. Ann Emerg Med. 2009;54:534.
18. Dowling, S, et al. Accuracy of Ottawa Ankle Rules to exclude fractures of the ankle and midfoot: A meta-analysis. Acad Emerg Med. 2009;16:277.
19. Fiesseler, F, Szucs, P, Kec, R, Richman, PB. Can nurses appropriately interpret the Ottawa Ankle Rule? Am J Emerg Med. 2004;22:145.
20. Derksen, RJ, et al. Can nurses appropriately interpret the Ottawa Ankle Rule? [letter]. Am J Emerg Med. 2004;23:201.
21. Derksen, RJ, et al. Specialized emergency nurses treating ankle and foot injuries: A randomized controlled trial. Am J Emerg Med. 2007;25:144.
22. Holroyd, BR, Wilson, D, Rowe, BH, Mayes, DC, Noseworthy, T. Uptake of validated clinical practice guidelines: Experience with implementing the Ottawa Ankle Rules. Am J Emerg Med. 2004;22:149.
23. Brehaut, JC, Stiell, IG, Visentin, L, Graham, ID. Clinical decision rules “in the real world”: How a widely disseminated rule is used in everyday practice. Acad Emerg Med. 2005;12:948.
24. Bencardino, JT, Rosenberg, ZS. MR imaging and CT in the assessment of osseous abnormalities of the ankle and foot. Magn Reson Imaging Clin N Am. 2001;9:567.
25. Muthukumar, T, Butt, SH, Cassar-Pullicino, VN. Stress fractures and related disorders in foot and ankle: Plain films, scintigraphy, CT and MR imaging. Semin Musculoskelet Radiol. 2005;9:210.
26. Choplin, RH, Buckwalter, KA, Rydberg, J, Farber, JM. CT with 3D rendering of the tendons of the foot and ankle: Technique, normal anatomy, and disease. Radiographics. 2004;24:343.
27. Johnson, PT, Fayad, LM, Fishman, EK. Sixteen-slice CT with volumetric analysis of foot fractures. Emerg Radiol. 2006;12:171.
28. Leffler, S, Disler, DG. MR imaging of tendon, ligament, and osseous abnormalities of the ankle and hindfoot. Radiol Clin North Am. 2002;40:1147.
29. Buckwalter, KA. CT arthrography. Clin Sports Med. 2006;25:899.
30. Scharf, S. SPECT/CT Imaging in general orthopedic practice. Semin Nucl Med. 2009;39:293.
31. Dahners, LE. The pathogenesis and treatment of bimalleolar ankle fractures. Instr Course Lect. 1990;39:85.
32. Michelson, JD, Magid, D, McHale, K. Clinical utility of a stability-based ankle fracture classification system. J Orthop Trauma. 2007;21:307.
33. Kennedy, JG, et al. An evaluation of the Weber classification of ankle fractures. Injury. 1998;29:577.
34. Shariff, SS, Nathwani, DK. Lauge-Hansen classification—a literature review. Injury. 2006;37:888.
35. Gardner, MJ, Demetrakopoulos, D, Briggs, SM, Helfet, DL, Lorich, DG. The ability of the Lauge-Hansen classification to predict ligament injury and mechanism in ankle fractures: An MRI study. J Orthop Trauma. 2006;20:267.
36. Stiehl, JB. Open fractures of the ankle joint. Instr Course Lect. 1990;39:113.
37. Newton, EJ, Love, J. Emergency department management of selected orthopedic injuries. Emerg Med Clin North Am. 2007;25:763.
38. Michelson, JD. Fractures about the ankle. J Bone Joint Surg Am. 1995;77:142.
39. Broos, PL, Bisschop, AP. Operative treatment of ankle fractures in adults: Correlation between types of fracture and final results. Injury. 1991;22:403.
40. Martin, AG. Weber B ankle fracture: An unnecessary fracture clinic burden. Injury. 2004;35:805.
41. Gardner, MJ, Demetrakopoulos, D, Briggs, SM, Helfet, DL, Lorich, DG. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot Ankle Int. 2006;27:788.
42. Donken, CC, Goorden, AJ, Verhofstad, MH, Edwards, MJ, van Laarhoven, CJ. The outcome at 20 years of conservatively treated “isolated” posterior malleolar fractures of the ankle: A case series. J Bone Joint Surg Br. 2011;93:1621.
43. Wei, SY, Okereke, E, Winiarsky, R, Lotke, PA. Nonoperatively treated displaced bimalleolar and trimalleolar fractures: A 20-year follow-up. Foot Ankle Int. 1999;20:404.
44. Tejwani, NC, et al. Are outcomes of bimalleolar fractures poorer than those of lateral malleolar fractures with medial ligamentous injury? J Bone Joint Surg Am. 2007;89:1438.
45. Sherbondy, PS, Sebastianelli, WJ. Stress fractures of the medial malleolus and distal fibula. Clin Sports Med. 2006;25:129.
46. Grantham, SA. Trimalleolar ankle fractures and open ankle fractures. Instr Course Lect. 1990;39:105.
47. Gosselin, RA, Roberts, I, Gillespie, WJ. Antibiotics for preventing infection in open limb fractures. Cochrane Database Syst Rev. 1, 2004.
48. Nanchahal, J, et al. Standards for the Management of Open Fractures of the Lower Limb. London: Royal Society of Medicine Press; 2010.
49. Hoiness, P, Stromsoe, K. Early complications of surgically managed ankle fractures related to the AO classification: A review of 118 ankle fractures treated with open reduction and internal fixation. Arch Orthop Trauma Surg. 1999;119:276.
50. Crist, BD, Khazzam, M, Murtha, YM, Della Rocca, GJ. Pilon fractures: Advances in surgical management. J Am Acad Orthop Surg. 2011;19:1610.
51. Harris, AM, Patterson, BM, Sontich, JK, Vallier, HA. Results and outcomes after operative treatment of high energy tibial plafond fractures. Foot Ankle Int. 2006;27:256.
52. Kilian, O, Bündner, MS, Horas, U, Heiss, C, Schnettler, R. [Long-term results in the surgical treatment of pilon tibial fractures. A retrospective study.]. Chirurg. 2002;73:65.
53. Sirkin, M, Sanders, R, DiPasquale, T, Herscovici, D, Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 2004;18(8 Suppl):S32.
54. Blauth, M, Bastian, L, Krettek, C, Knop, C, Evans, S. Surgical options for the treatment of severe tibial pilon fractures: A study of three techniques. J Orthop Trauma. 2001;15:153.
55. Bridgman, SA, et al. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg Med J. 2003;20:508.
56. Fernandez, WG, Yard, EE, Comstock, RD. Epidemiology of lower extremity injuries among U.S. high school athletes. Acad Emerg Med. 2007;14:641.
57. McKay, GD, Goldie, PA, Payne, WR, Oakes, BW. Ankle injuries in basketball: Injury rate and risk factors. Br J Sports Med. 2001;35:103.
58. Fallat, L, Grimm, DJ, Saracco, JA. Sprained ankle syndrome: Prevalence and analysis of 639 acute injuries. J Foot Ankle Surg. 1998;37:280.
59. Cooke, MW, Lamb, SE, Marsh, J, Dale, J. A survey of current consultant practice of treatment of severe ankle sprains in emergency departments in the United Kingdom. Emerg Med J. 2003;20:505.
60. Kerkhoffs, GM, et al. Different functional treatment strategies for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 3, 2002.
61. Malliaropoulos, N, Papacostas, E, Papalada, A, Maffulli, N. Acute lateral ankle sprains in track and field athletes: An expanded classification. Foot Ankle Clin. 2006;11:497.
62. Williams, GN, Jones, MH, Amandola, A. Syndesmotic ankle sprains in athletes. Am J Sports Med. 2007;35:1197.
63. Anandacoomarasamy, A, Barnsley, L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39:e14.
64. Valderrabano, V, Hintermann, B, Horisberger, M, Fung, TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34:612.
65. van Dijk, CN, Lim, LS, Bossuyt, PM, Marti, RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78:958.
66. Frost, SC, Amendola, A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9:40.
67. Kerkhoffs, GM, Handoll, HH, de Bie, R, Rowe, BH, Struijs, PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2, 2007.
68. Kerkhoffs, GM, et al. Functional treatments for acute ruptures of the lateral ankle ligament: A systematic review. Acta Orthop Scand. 2003;74:69.
69. Janis, LR, Kittleson, RS, Cox, DG. Chronic lateral ankle instability: Assessment of subjective outcomes following delayed primary repair and a new secondary construction. J Foot Ankle Surg. 1998;37:369.
70. Wedmore, IS, Charette, J. Emergency department evaluation and treatment of ankle and foot injuries. Emerg Med Clin North Am. 2000;18:85.
71. Boyce, SH, Quigley, MA, Campbell, S. Management of ankle sprains: A randomized controlled trial of the treatment of inversion injuries using an elastic support bandage or an Aircast ankle brace. Br J Sport Med. 2005;39:91.
72. Beynnon, BD, Renström, PA, Haugh, L, Uh, BS, Barker, H. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34:1401.
73. Kerkhoffs, GM, et al. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 3, 2002.
74. Struijs, PA, Kerkhoffs, GM. Ankle sprain. Clin Evid (Online). 2010;5:1115.
75. Lamb, SE, et al. Mechanical supports for acute, severe ankle sprain: A pragmatic, multicentre, randomised controlled trial. Lancet. 2009;373:575.
76. Bleakly, CM, et al. Effect of accelerated rehabilitation on function after ankle sprain: Randomised controlled trial. BMJ. 2010;340:c1964.
77. Kerkhoffs, GM, et al. Immobilisation for acute ankle sprain: A systematic review. Arch Orthop Trauma Surg. 2001;121:462.
78. Nadarajah, A, Abrahan, L, Lau, FL, Hwang, LJ, Fakir-Bolte, C. Efficacy and tolerability of celecoxib compared with diclofenac slow release in the treatment of acute ankle sprain in an Asian population. Singapore Med J. 2006;47:534.
79. Cukiernik, VA, et al. Naproxen versus acetaminophen for therapy of soft tissue injuries to the ankle in children. Ann Pharmacother. 2007;41:1368.
80. Hewitt, DJ, et al. Tramadol/acetaminophen or hydrocodone/acetaminophen for the treatment of ankle sprain: A randomized, placebo-controlled trial. Ann Emerg Med. 2007;49:468.
81. Mahler, P, et al. Double-blind, randomized, controlled study on the efficacy and safety of novel diclofenac epolamine gel formulated with lecithin for the treatment of sprains, strains and contusions. Drugs Exp Clin Res. 2003;29:45.
82. Predel, HG, et al. Diclofenac patch for topical treatment of acute impact injuries: A randomised, double blind, placebo controlled, multicentre study. Br J Sports Med. 2004;38:318.
83. Arnold, BL, Docherty, CL. Bracing and rehabilitation—what’s new. Clin Sports Med. 2004;23:83.
84. Rotem-Lehrer, N, Laufer, Y. Effect of focus of attention on transfer of a postural control task following an ankle sprain. J Orthop Sports Phys Ther. 2007;37:564.
85. Karlsson, J, Eriksson, BI, Swärd, L. Early functional treatment for acute ligament injuries of the ankle joint. Scand J Med Sci Sports. 1996;6:341.
86. Mansour, R, Jibri, Z, Kamath, S, Mukherjee, K, Ostlere, S. Persistent ankle pain following a sprain: Review of imaging. Emerg Radiol. 2011;18:211.
87. Parmar, C, Meda, KP. Achilles tendon rupture associated with combination therapy of levofloxacin and steroid in four patients and a review of the literature. Foot Ankle Int. 2007;28:1287.
88. Ufberg, J, Harrigan, RA, Cruz, T, Perron, AD. Orthopedic pitfalls in the ED: Achilles tendon rupture. Am J Emerg Med. 2004;22:596.
89. Thompson, TC, Doherty, JH. Spontaneous rupture of tendon of Achilles: A new clinical diagnostic test. J Trauma. 1962;2:126.
90. Mayich, DJ, Younger, A, Krause, F. The reverse Silfverskiöld test in Achilles tendon rupture. CJEM. 2009;11:242.
91. Khan, RJ, Carey Smith, RL. Surgical interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev. 9, 2010.
92. Wong, J, Barrass, V, Maffulli, N. Quantitative review of operative and nonoperative management of Achilles tendon ruptures. Am J Sports Med. 2002;30:565.
93. Baer, GS, Keene, JS. Tendon injuries of the foot and ankle. In DeLee JC, Drez D, Miller MD, eds.: DeLee and Drez’s Orthopedic Sports Medicine: Principles and Practice, 3rd ed, Philadelphia: Elsevier, 2009.
94. Strauss, EJ, Ishak, C, Jazrawi, L, Sherman, O, Rosen, J. Operative treatment of acute Achilles tendon ruptures: An institutional review of clinical outcomes. Injury. 2007;38:832.
95. Khan, RJ, et al. Treatment of acute Achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am. 2005;87:2202.
96. Lansdaal, JR, et al. The results of 163 Achilles tendon ruptures treated by a minimally invasive surgical technique and functional aftertreatment. Injury. 2007;38:839.
97. Scott, WN, Inglis, AE, Sculco, TP. Surgical treatment of reruptures of the tendoachilles following nonsurgical treatment. Clin Orthop Relat Res. 1979;140:175.
98. Selmani, E, Gjata, V, Gjika, E. Current concepts review: Peroneal tendon disorders. Foot Ankle Int. 2006;27:221.
99. Ogawa, BK, Thordarson, DB. Current concepts review: Peroneal tendon subluxation and dislocation. Foot Ankle Int. 2007;28:1034.
100. Slater, HK. Acute peroneal tendon tears. Foot Ankle Int. 2007;12:659.
101. Major, NM, Helms, CA, Fritz, RC, Speer, KP. The MR imaging appearance of longitudinal split tears of the peroneal brevis tendon. Foot Ankle Int. 2000;21:514.
102. Foster, AP, Thompson, NW, Crone, MD, Charlwood, AP. Rupture of the tibialis posterior tendon: An important differential in the assessment of ankle injuries. Emerg Med J. 2005;22:915.
103. Michelson, J, Dunn, L. Tenosynovitis of the flexor hallucis longus: A clinical study of the spectrum of presentation and treatment. Foot Ankle Int. 2005;26:291.
104. Rivera, F, Bertone, C, De Martino, M, Pietrobono, D, Ghisellini, F. Pure dislocation of the ankle: Three case reports and literature review. Clin Sports Med. 2006;16:269.
105. Wroble, RR, Nepola, JV, Malvitz, TA. Ankle dislocation without fracture. Foot Ankle Int. 1988;9:64.
106. Ounpuu, S. The biomechanics of walking and running. Clin Sports Med. 1994;13:843.
107. Young, CC, Niedfeldt, MW, Morris, GA, Eerkes, KJ. Clinical examination of the foot and ankle. Prim Care. 2005;32:105.
108. Roche, A, Hunter, L, Pocock, N, Brown, D. Physical examination of the foot and ankle by orthopaedic and accident and emergency clinicians. Injury. 2009;40:136.
109. Koulouris, G, Morrison, WB. Foot and ankle disorders: Radiographic signs. Semin Roentgenol. 2005;40:358.
110. De Smet, AA, Doherty, MP, Norris, MA, Hollister, MC, Smith, DL. Are oblique views needed for trauma radiography of the distal extremities? AJR Am J Roentgenol. 1999;172:1561.
111. Gratton, MC, Salomone, JA, Watson, WA. Clinically significant radiograph misinterpretations at an emergency medicine residency program. Ann Emerg Med. 1990;19:497.
112. Mellado, JM, et al. Accessory ossicles and sesamoid bones of the ankle and foot: Imaging findings, clinical significance, and differential diagnosis. Eur Radiol. 2003;13(Suppl 4):L164.
113. Miller, TT. Painful accessory bones of the foot. Semin Musculoskelet Radiol. 2002;6:153.
114. Lewis, P. Scintigraphy in the foot and ankle. Foot Ankle Clin. 2000;5:1.
115. Teague, DC. Stress fractures. In: Bucholz RW, Court-Brown CM, Heckman JD, Tornetta P, eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott: Williams & Wilkins; 2010:518–530.
116. Watura, R, Cobby, M, Taylor, J. Multislice CT in imaging trauma of the spine, pelvis, and complex foot injuries. Br J Radiol. 2004;77:S46.
117. Umans, HR. Imaging sports medicine injuries of the foot and toes. Clin Sports Med. 2006;25:763.
118. Zoga, AC, Schweitzer, ME. Imaging sports injuries of the foot and ankle. Magn Reson Imaging Clin N Am. 2003;11:295.
119. Kavanagh, EC, Zoga, AC. MRI of trauma to the foot and ankle. Semin Musculoskelet Radiol. 2006;10:308.
120. Cerezal, L, Abascal, F, García-Valtuille, R, Canga, A. Ankle MR arthrography: How, why and when. Radiol Clin North Am. 2005;43:693.
121. Anmad, J, Raikin, SM. Current concepts review: Talar fractures. Foot Ankle Int. 2006;27:475.
122. Berkowitz, MJ, Kim, DH. Process and tubercle fractures of the hindfoot. J Am Acad Orthop Surg. 2005;13:492.
123. Chan, GM, Yoshida, D. Fracture of the lateral process of the talus associated with snowboarding. Ann Emerg Med. 2003;41:854.
124. Vallier, HA, Nork, SE, Barei, DP, Benirschke, SK, Sangeorzan, BJ. Talar neck fractures: Results and outcomes. J Bone Joint Surg Am. 2004;86:1616.
125. Abrahams, TG, Gallup, L, Avery, FL. Nondisplaced shearing-type talar body fractures. Ann Emerg Med. 1994;23:891.
126. Horst, F, Gilbert, BJ, Nunley, JA. Avascular necrosis of the talus: Current treatment options. Foot Ankle Clin. 2004;9:757.
127. Schachter, AK, Chen, AL, Reddy, PD, Tejwani, NC. Osteochondral lesions of the talus. J Am Acad Orthop Surg. 2005;13:152.
128. O’Loughlin, PF, Heyworth, BE, Kennedy, JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38:392.
129. Frost, A, Roach, R. Osteochondral injuries of the foot and ankle. Sports Med Arthrosc. 2009;17:187.
130. Naran, KN, Zoga, AC. Osteochondral lesions about the ankle. Radiol Clin North Am. 2008;46:995.
131. Stroud, CC, Marks, RM. Imaging of osteochondral lesions of the talus. Foot Ankle Clin. 2000;5:119.
132. van Dijk, CN, Reilingh, ML, Zengerink, M, van Bergen, CJ. The natural history of osteochondral lesions in the ankle. Instr Course Lect. 2010;59:375.
133. Kelberine, F, Frank, A. Arthroscopic treatment of osteochondral lesions of the talar dome: A retrospective study of 48 cases. Arthroscopy. 1999;15:77.
134. Bibbo, C, Anderson, RB, Davis, WH. Injury characteristics and the clinical outcome of subtalar dislocations: A clinical and radiographic analysis of 25 cases. Foot Ankle Int. 2003;24:158.
135. de Palma, L, Santucci, A, Marinelli, M, Borgogno, E, Catalani, A. Clinical outcome of closed isolated subtalar dislocations. Arch Orthop Trauma Surg. 2008;128:593.
136. Wagner, R, Blattert, TR, Weckbach, A. Talar dislocations. Injury. 2004;35(Suppl 2):SB36.
137. Daftary, A, Haims, AH, Baumgaertner, MR. Fractures of the calcaneus: A review with emphasis on CT. Radiographics. 2005;25:1215.
138. Hess, M, Booth, B, Laughlin, RT. Calcaneal avulsion fractures: Complications from delayed treatment. Am J Emerg Med. 2008;26:254e1.
139. Hodge, JC. Anterior process fracture or calcaneus secundarius: A case report. J Emerg Med. 1999;17:305.
140. Maskill, JD, Bohay, DR, Anderson, JG. Calcaneus fractures: A review article. Foot Ankle Clin. 2005;10:463.
141. Ibrahim, T, et al. Displaced intra-articular calcaneal fractures: 15-year follow-up of a randomised controlled trial of conservative versus operative treatment. Injury. 2007;38:848.
142. Knight, JR, Gross, EA, Bradley, GH, Bay, C, LoVecchio, F. Boehler’s angle and the critical angle of Gissane are of limited use in diagnosing calcaneus fracture in the ED. Am J Emerg Med. 2006;24:423.
143. Brian, PL, Mahraj, RP. Imaging of the calcaneus. Foot Ankle Clin. 2005;10:443.
144. Swanson, SA, Clare, MP, Sanders, RW. Management of intra-articular fractures of the calcaneus. Foot Ankle Clin. 2008;13:659.
145. Germann, CA, Perron, AD, Miller, MD, Powell, SM, Brady, WJ. Orthopedic pitfalls in the ED: Calcaneal fractures. Am J Emerg Med. 2004;22:607.
146. Pinney, SJ, Sangeorzan, BJ. Fractures of the tarsal bones. Orthop Clin North Am. 2001;32:21.
147. Mengiardi, B, Pfirrmann, CW, Zanetti, M. MR imaging of tendons and ligaments of the midfoot. Semin Musculoskelet Radiol. 2005;9:187.
148. Swords, MP, Schramski, M, Switzer, K, Nemec, S. Chopart fractures and dislocations. Foot Ankle Clin. 2008;13:679.
149. DiGiovanni, CW. Fractures of the navicular. Foot Ankle Clin. 2004;9:25.
150. Ceroni, D, De Rosa, V, De Coulon, G, Kaelin, A. Cuboid nutcracker fracture due to horseback riding in children: Case series and review of the literature. J Pediatr Orthop. 2007;27:557.
151. Mihalich, RM, Early, JS. Management of cuboid crush injuries. Foot Ankle Clin. 2006;11:121.
152. Reid, JJ, Early, JS. Fractures and dislocations of the midfoot and forefoot. In: Bucholz RW, Court-Brown CM, Heckman JD, Tornetta P, eds. Rockwood and Green’s Fractures in Adults. 7th ed. Philadelphia: Wolters Kluwer Health/Lippincott: Williams & Wilkins; 2010:2110–2174.
153. Chiodo, CP, Myerson, MS. Developments and advances in the diagnosis and treatment of injuries to the tarsometatarsal joint. Orthop Clin North Am. 2001;32:11.
154. Desmond, EA, Chou, LB. Current concepts review: Lisfranc injuries. Foot Ankle Int. 2006;27:653.
155. Hunt, SA, Ropiak, C, Tejwani, NC. Lisfranc joint injuries: Diagnosis and treatment. Am J Orthop. 2006;35:376.
156. Saab, M. Lisfranc fracture-dislocation: An easily overlooked injury in the emergency department. Eur J Emerg Med. 2005;12:143.
157. Perron, AD, Brady, WJ, Keats, TE. Orthopedic pitfalls in the ED: Lisfranc fracture-dislocation. Am J Emerg Med. 2001;19:71.
158. Sherief, TI, Mucci, B, Greiss, M. Lifranc injury: How frequently does it get missed? And how can we improve? Injury. 2007;38:856.
159. Germann, CA, Perron, AD. Risk management and avoiding legal pitfalls in the emergency treatment of high-risk orthopedic injuries. Emerg Med Clin North Am. 2010;28:969.
160. Arntz, CT, Veith, RG, Hansen, ST. Fractures and fracture-dislocations of the tarsometatarsal joint. J Bone Joint Sur Am. 1988;70:173.
161. Gupta, RT, Wadhwa, RP, Learch, TJ, Herwick, SM. Lisfranc injury: Imaging findings for this important but often-missed diagnosis. Curr Probl Diagn Radiol. 2008;37:115.
162. Raikin, SM. Prediction of midfoot instability in the subtle Lisfranc injury. Comparison of magnetic resonance imaging with intraoperative findings. J Bone Joint Surg Am. 2009;91:892.
163. Philbin, T, Rosenberg, G, Sferra, JJ. Complications of missed or untreated Lisfranc injuries. Foot Ankle Clin. 2003;8:61.
164. Aronow, MS. Treatment of the missed Lisfranc injury. Foot Ankle Clin. 2006;11:127.
165. Hatch, RL, Alsobrok, JA, Clugston, JR. Diagnosis and management of metatarsal fractures. Am Fam Physician. 2007;76:817.
166. Fetzer, GB, Wright, RW. Metatarsal shaft fractures and fractures of the proximal fifth metatarsal. Clin Sports Med. 2006;25:139.
167. Rammelt, S, Heineck, J, Zwipp, H. Metatarsal fractures. Injury. 2004;35(Suppl 2):SB77–SB86.
168. Vorlat, P, Achtergael, W, Haentjens, P. Predictors of outcome of non-displaced fractures of the base of the fifth metatarsal. Int Orthop. 2007;31:5.
169. Chuckpaiwong, B, Queen, RM, Easley, ME, Nunley, JA. Distinguishing Jones and proximal diaphyseal fractures of the fifth metatarsal. Clin Orthop Relat Res. 2008;466:1966.
170. Richli, WR, Rosenthal, DI. Avulsion fracture of the fifth metatarsal: Experimental study of pathomechanics. AJR Am J Roentgenol. 1984;143:889.
171. Mologne, TS, Lundeen, JM, Clapper, MF, O’Brien, TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970.
172. Schnaue-Constantouris, EM, Birrer, RB, Grisafi, PJ, Dellacorte, MP. Digital foot trauma: Emergency diagnosis and treatment. J Emerg Med. 2001;22:163.
173. Smith, GD, Hart, RG, Wolff, TW. Slipper cast management of emergency foot problems. Am J Emerg Med. 2004;23:343.
174. Vilke, GM. Great toe pain. J Emerg Med. 2003;24:59.
175. Lutter, LD. Hindfoot problems. Instr Course Lect. 1993;42:195.
176. Karr, SD. Subcalcaneal heel pain. Orthop Clin North Am. 1994;25:161.
177. Cullen, NP, Singh, D. Plantar fasciitis: A review. Br J Hosp Med. 2006;67:72.
178. Wearing, SC, Smeathers, JE, Urry, SR, Hennig, EM, Hills, AP. The pathomechanics of plantar fasciitis. Sports Med. 2006;36:585.
179. Rompe, JD, Furia, J, Weil, L, Maffulli, N. Shock wave therapy for chronic plantar fasciopathy. Br Med Bull. 2007;183:81–82.
180. Kinoshita, M, Okuda, R, Yasuda, T, Mi, Abe. Tarsal tunnel syndrome in athletes. Am J Sports Med. 2006;34:1307.
181. Wu, KK. Morton neuroma and metatarsalgia. Curr Opin Rheumatol. 2000;12:131.
182. Thompson, CE, Gibson, JN, Martin, D. Interventions for the treatment of Morton’s neuroma. Cochrane Database Syst Rev. 3, 2004.
183. Bos, AM, van Tilburg, MW, van Sorge, AA, Klinkenbijl, JH. Randomized trial of surgical technique and local antibiotics for ingrowing toenail. Br J Surg. 2007;94:292.
184. Harrast, MA, Colonno, D. Stress fractures in runners. Clin Sports Med. 2010;29:399.
185. Zeni, AI, Street, CC, Dempsey, RL, Staton, M. Stress injury to bone among women athletes. Phys Med Rehabil Clin N Am. 2000;11:929.
186. Gehrmann, RM, Renard, RL. Current concepts review: Stress fractures of the foot. Foot Ankle Int. 2006;27:750.
187. Feingold, D, Hame, SL. Female athlete triad and stress fractures. Orthop Clin North Am. 2006;37:575.
188. McGee, DL, Dalsey, WC. The mangled extremity: Compartment syndrome and amputations. Emerg Med Clin North Am. 1992;10:783.
189. Oakes, R, Urban, A, Levy, PD. The mangled extremity. J Emerg Med. 2008;35:437.
190. Cannada, L. The mangled extremity: Limb salvage vs. amputation. Curr Surg. 2005;62:563.
191. Tarkin, IS, Sop, A, Pape, HC. High-energy foot and ankle trauma: Principles for formulating an individualized care plan. Foot Ankle Clin. 2008;13:705.
192. Maurel, B, Brilhault, J, Martinez, R, Lermusiaux, P. Compartment syndrome with food ischemia after inversion injury of the ankle. J Vasc Surg. 2007;46:369.
193. Fulkerson, E, Razi, A, Tejwani, N. Review: Acute compartment syndrome of the foot. Foot Ankle Int. 2003;24:180.
194. Richter, J, Schulze, W, Klaas, A, Clasbrummel, B, Muhr, G. Compartment syndrome of the foot: An experimental approach to pressure measurement and release. Arch Orthop Trauma Surg. 2008;128:199.