ANIMAL ATTACKS
Most animal attacks are from “man’s best friend,” the pet dog. Other animals that will attack humans, given provocation, include the cat, rat, raccoon, tiger, lion, skunk, squirrel, camel, elephant, bear, alligator, crocodile, bat, wolf, rhinoceros, and hippopotamus. Although there are unique variations to the nature of the wounds created by different animals (in most part related to the size of the animal, types of teeth and claws, and risk of infection), the basic out-of-hospital management of an animal bite or mauling is the same for all creatures.
GENERAL TREATMENT
1. If a person is bitten or mauled by an animal, apply pressure to stop any brisk bleeding, and follow the instructions for management of bleeding and cuts (see pages 54 and 260).
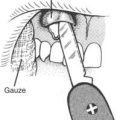
2. It is important to clean the wounds well. Flush any injury that has broken the skin with at least 2 quarts (liters) of disinfected water, scrub with mild soap, and flush again. If you are carrying povidone iodine (Betadine) solution 10% (not soap or scrub); benzalkonium (Zephiran) liquid 1% antiseptic; or, in a pinch, Bactine antiseptic (benzalkonium 0.13%), rinse the wound with one of these for 1 minute (to help kill rabies virus), and then rinse away the solution until there is no discoloration of the wound.
3. Do not tightly sew or tape closed any animal bite, unless it is absolutely essential to allow rescue. If a large tear is present, the wound edges can be held together with tape and wraps (see page 266). Tight closure of a contaminated wound (all animal bites and scratches introduce bacteria into the wound) can lead to a devastating infection. Apply a thin layer of bacitracin or mupirocin ointment or mupirocin cream into the wound.
4. If the victim is more than 5 hours from a physician, administer cefuroxime axetil, dicloxacillin, azithromycin, amoxicillin–clavulanic acid, cefixime, cephalexin, trimethoprim-sulfamethoxazole, or ciprofloxacin with clindamycin. If the bite is from a cat, domestic or wild, administer an antibiotic as soon as possible. If an animal bite becomes infected, the same antibiotics are recommended, with the exception that for cat (domestic and “big” cat) bites, dicloxacillin should be given with penicillin.
SPECIAL CONSIDERATIONS
High-Risk Wounds
Wounds at high risk for infection include bites to the hands and feet, and all puncture wounds (see page 258). These should be rinsed copiously and never cinched shut by any method. Anyone who sustains such a wound should be given antibiotics for 4 days (see step 4 on page 409). Cat, human, and primate bites are enormously prone to infection, and require prompt attention by a physician. In a typical human bite, which occurs when a closed fist strikes an opponent’s teeth, the cut extends deeply into a knuckle and inoculates the underlying tendon sheath with saliva and bacteria. As the fist is opened, the wound becomes “closed,” and an infection can develop quickly. If a human bite is incurred in this manner, splint the hand in the position of function (see Figure 39) and administer cefuroxime axetil, ciprofloxacin plus erythromycin, or dicloxacillin plus ampicillin for 7 days.
Rabies
Rabies virus infection occurs more frequently in wild than in domestic animals. In some foreign countries where immunization of animals is infrequently practiced, the risk is great even in domesticated animals. The virus is carried in saliva and is transmitted by bite or lick (if the skin is broken). It has been transmitted by bats in caves either by aerosolized saliva or undetected bites. Raccoons, dogs, cats, foxes, coyotes, skunks, wolves, bats, woodchucks, and groundhogs are the most common carriers. Rabies has not been reported in bears. Although rabbits, hares, mice, squirrels, chipmunks, rats, guinea pigs, and ferrets may be rabid, they are rarely involved in the transmission of rabies to humans. Domestic animals such as cattle, horses, and sheep become infected in regions where skunk or raccoon rabies is found. In developing countries in Asia, Africa, and South and Central America, dogs are the most common carriers.
The incubation period of rabies ranges from 9 days to more than 1 year, but is usually between 2 and 16 weeks. The first symptoms are fatigue, weakness, anxiety, irritability, fever, headache, nausea and vomiting, sore throat, abdominal pain, and loss of appetite. Some victims complain of numbness and tingling where they were initially bitten. After a few days to 2 weeks, the virus shows its devastating effect on the nervous system, with symptoms of increased agitation, hyperactivity, seizures, hallucinations, uncontrollable behavior, and inability to drink (hydrophobia) because of muscle spasms in the throat. This constellation is called “furious rabies.” With “dumb” rabies, a person becomes progressively weak, uncoordinated, and paralyzed. Unfortunately, rabies is virtually always fatal, with the terminal events being one or more of coma, respiratory failure, seizures, abnormal heart rhythms, paralysis, and pneumonia.
Skunks
1. Fels Naphtha soap. Wet an affected dog with water and rub it down with the soap. Be sure to rinse the animal well.
2. One box of baking soda. Slightly moisten the animal and then and rub the fur thoroughly with the baking soda, using gloved hands. Then, take a bottle of white household vinegar—keeping vinegar far away from eyes, nose, and mouth of the animal—and pour it directly onto the baking soda impregnated coat. The immediate and violent effervescence is supposed to lift out the musk and odor. Spray or otherwise rinse the animal thoroughly after allowing for full interaction between baking soda and vinegar.
Bubonic Plague
Cases of bubonic plague are still reported in the United States. The disease is transmitted by the bites of fleas that have acquired the plague bacillus, Yersinia pestis, from infected squirrels, rats, prairie dogs, chipmunks, marmots, rabbits, and mice. Rarely, the disease can be contracted from direct contact with infected pets, particularly cats. It can also be contracted from skinning an infected wild animal, such as a coyote or bobcat.
Preexposure immunization against plague is available (see page 455). If you have not been immunized against plague and will be actively exposed to plague-infected animals, ingest tetracycline 500 mg four times a day during the period of exposure.
Anthrax
Anthrax is a communicable disease caused by Bacillus anthracis transmitted by spores via inhalation, ingestion (contaminated meat), or inoculation into the skin. The spores can persist in the environment for years, and are typically present in infected animals or contaminated animal products. Anthrax is not transmitted from person to person. After exposure to the spores, the incubation period is typically 1 to 5 days, although it can be as long as 40 days. With inhalation anthrax, the victim initially has a nonspecific flu-like illness (fever, fatigue, muscle pains, dry cough, and chest or abdominal pain) followed by severe respiratory distress and overwhelming infection that leads to shock and death. With cutaneous anthrax, the first lesion is usually a painless red raised area on the head, neck, or limb, usually at the site of a small cut or scrape through which the spore enters. In a day or two, a clear blister(s) forms, surrounded by swelling. The blister ruptures, and then turns into an ulcer covered by a black crust in a few days. This disappears in a few weeks. With gastrointestinal anthrax, the victim suffers abdominal pain and swelling, nausea, vomiting, and bloody diarrhea 2 to 5 days after eating the undercooked spore-containing meat. He may also suffer from dizziness, fatigue, muscle aching, and fever. Anthrax may rarely cause primary infection of the lining of the brain, and cause a clinical presentation similar to meningitis (see page 174).
AVOIDANCE OF HAZARDOUS ANIMALS
1. Do not surprise or otherwise provoke animals. Unless they are apex predators, starving, senile, or ill, most animals will not attack humans without provocation. Do not corner or provoke a carnivore. Do not tease animals. Do not approach an animal when it is with young. If you are a photographer approaching a wild animal that may become provoked and charge, do not come any closer to the animal than 100 yards distance. Some experts say that you should attempt to stay even further away from a bear.
2. Do not disturb a feeding animal. Do not explore into its feeding territory, approach during rut, or disrupt mating patterns.
3. Do not separate fighting animals using your bare hands. If possible, drive animals apart using a long stick or club.
4. In bear country, make your presence known by calling out, clapping your hands, or otherwise making noise, particularly when approaching streams and blind spots on the trail. Hang all food off the ground in trees away from the campsite. Never keep food or captured game inside a tent. Use proper food storage to keep food away from bears. Cook at a site away from the sleeping area. Do not sleep in clothes worn while cooking or eating. Make noise when hiking, particularly on narrow paths or through tall grass. If you confront a brown (grizzly) bear, avoid eye contact and try to slowly back away. If you confront a black bear, shout, yell, throw rocks or sticks, or do whatever you can to frighten off the animal. If attacked by a bear, do not try to outrun it; you can’t. If you are carrying pepper spray (at least 1% capsaicin or capsaicinoids) in a canister intended for use against a bear (“bear pepper spray” that meets EPA standards; a spray distance of 25 feet under optimum conditions, minimum spray duration of 6 seconds, minimum net content of 7.9 ounces or 2.25 grams), use it if you have time. Personal defensive spray, such as Mace, will likely not work because the canister shoots a relatively thin stream and the substance is not sufficiently potent. Carry the spray where it is obvious and can be immediately deployed. It should be on a holster on your waist or chest, not in the bottom of your pack. Show your companions its location. If you are not carrying bear pepper spray, cover your head and the back of your neck with your arms and curl into a fetal position or lay flat on the ground, face down, to protect your abdomen. If you are wearing a backpack, keep it on for additional protection. Use your elbows to cover your face if a bear turns you over. After a bear attack, remain on the ground until you are certain that the bear has left the area. More than one victim has successfully protected himself during the initial attack, only to arise too soon (before the bear has lost interest and left the area) and be mauled during the second attack.
5. Never leave a small child alone with an animal, regardless of the animal’s demeanor.
6. Do not pet or feed animals (particularly dogs and monkeys).