Head and neck
A Cleft palate and lip
Cleft palate
Cleft palate repair is usually performed in stages, depending on the extent of the defect. For the more severe deformities, the initial operation repairs the lip and anterior portion of the hard palate. The soft palate and other deformities are usually corrected later after 6 months of age. Infants with cleft lip deformities can have difficulty feeding and may be prone to malnutrition and congenital (heart) anomalies and disease.
a) Intubation may be difficult because the laryngoscope blade can slip into the cleft. However, packing the cleft with gauze may prevent this from occurring.
b) An oral RAE tube or flexible connector is used and secured at the midline of the lower lip.
c) A specialized mouth gag is used to hold the mouth open and the endotracheal tube (ETT) in place during cleft palate surgery.
d) All air bubbles should be carefully removed from intravenous (IV) lines to prevent an air embolus because of the incidence of associated cardiac anomalies, such as an atrial ventricular defect (AVD), which may lead to air crossing from the venous to the arterial circulation.
e) Congenital heart diseases may influence drugs that are selected for maintenance of anesthesia and for infiltration of the operative site, particularly if epinephrine is selected.
f) Care must be implemented to protect the child’s eyes because accidental damage may occur during the surgical procedure.
g) Before emergence, a suture is often placed through the tip of the tongue, and the suture is taped to the cheek. This suture eliminates the need for an oral airway and prevents damage to the palatal repair.
h) If soft tissue obstruction occurs during emergence or recovery, traction on the suture can alleviate the problem. If edema occurs, a more aggressive and immediate airway management technique should be used.
i) Copious secretions, suctioning the stomach, and blood may cause laryngospasm after extubation; therefore, a clear airway is imperative.
Cleft lip
a) Management of unilateral cleft lip repair consists of routine induction followed by oral intubation using an oral RAE tube or a flexible connector.
b) Secure the tube to the lower lip and midline via tape. To decrease tension on the surgical sutures at the end of the procedure, the surgeon may place a Logan bow across the upper lip of the patient.
c) When the Logan bow is placed, mask ventilation during emergence will become impaired or impossible.
d) Extubation must be performed only with the patient fully awake and reflexes intact.
e) The child’s surgical site must also be protected from finger and hand manipulation. Some hospitals recommend the use of hand mittens or taping the extremities onto armboards during the postoperative period.
f) Close monitoring of respiration should proceed into the postoperative period.
B Dacryocystorhinostomy
Dacryocystorhinostomy is performed for patients who have chronic tearing or obstruction at the level of the nasolacrimal duct. This procedure restores drainage into the nose from the lacrimal sac. The surgeon injects lidocaine 1% with 1:100,000 epinephrine, bupivacaine (Marcaine) 0.75%, and hyaluronidase (Wydase) in the operative site along the lacrimal crest. An additional injection may be given along the medial orbital wall, anesthetizing the ethmoidal nerve. This block may cause a temporary dilated pupil or medial rectus muscle paralysis.
A small incision is made near the medial canthus to allow a subperiosteal dissection to the lacrimal sac. The bone between the lacrimal fossa and middle fossa is broken and cut, making a small canaliculi. The mucosa of the lacrimal sac is anastomosed to the mucosa of the nose. To prevent closure of the newly formed path by scarring, a silicone tube may be placed inside the duct. Muscles and tissues in the area are then closed. The patient is then asked to open the eyelids, and when the proper height is obtained, the incision is closed.
2. Preoperative assessment and patient preparation
a) History and physical examination: This procedure may be done in patients of varying age. The patient’s cardiac history should be determined because epinephrine is to be used for vasoconstriction. Infections in the surgical area should be treated with antibiotics for several days before surgery. Because of the inaccessibility of the anesthesia provider to the head, patients with obstructive sleep apnea (OSA) should also be identified and anesthesia planned accordingly.
a) Monitoring equipment: Standard
b) Additional equipment: An end-tidal carbon dioxide sensing nasal cannula may be used to give additional information about ventilation.
c) An extra-long circuit should be available because of turning of the table 90 to 180 degrees.
d) Drugs: Standard emergency and standard tabletop agents are used.
e) IV fluids: An age-appropriate IV line and fluid are used for pediatric patients. One 18-gauge IV line is used for adults with normal saline or lactated Ringer solution at 2 mL/kg/hr (blood loss should be minimal because of the use of epinephrine).
4. Perioperative management and anesthetic technique
Most of these procedures can be done with local anesthesia with sedation; general anesthesia is rarely used. The choice depends on the preferences of the surgeon and the patient preference.
a) Induction is routine for general surgery and the patient’s preference.
b) For local anesthesia with sedation, short-acting agents are best because these procedures are usually done on an outpatient basis.
d) Emergence: For general anesthesia, the patient should be extubated while awake unless the condition dictates otherwise (i.e., reactive airway disease).
There may be some temporary dilation of the pupil or medial rectus paralysis.
C Dental restoration
Dental restoration procedures are performed under general anesthesia for a multitude of reasons. These include rampant cavities, history of mental disability, and an uncooperative patient who is not an appropriate candidate for local anesthetic and an office procedure.
a) Mentally disabled patients often develop a close personal relationship with either a family member or their long-term health care worker. It is often suggested that this individual accompany the patient to decrease anxiety and communicate a health history to the anesthesia provider.
b) A thorough airway assessment should be performed before considering induction.
c) Oral midazolam (0.5 mg/kg) or ketamine (3–4 mg/kg IM) is most effective in sedating mentally disabled children in the preoperative arena.
d) Because many patients requiring dental restoration have congenital anomalies, it is common to find a patient with a small oropharynx, enlarged tonsils, a large tongue, and increased secretions.
e) Atlantoaxial instability and congenital heart disease should also be considered in the preoperative preparation and anesthetic management.
f) Preparation and appropriate airway management must be planned and implemented for these patients.
g) Patients who receive phenytoin to control seizures may have gingival hyperplasia. Because the gingiva is highly vascular, any surgical manipulation during restoration may lead to significant blood loss.
h) In patients with normal airways, a standard induction is appropriate and a nasal intubation usually facilitates the dental procedure.
i) The application of a topical vasoconstrictive nasal spray during the preoperative period reduces or prevents bleeding during the insertion of the nasotracheal tube.
j) After loss of consciousness, lubricated intranasal trumpets may be inserted into the most patent nasal airway. Starting with a smaller nasal trumpet, several are placed in increasing sizes to dilate the airway. When full dilation of the nares has occurred, a well-lubricated ETT is passed through the nose into the trachea, either blindly or assisted by Magill forceps under direct laryngoscopy.
k) The nasal ETT is preferably placed on the side opposite where the surgeon will be working. The ETT is often sewn to the nasal septum by the surgeon.
l) Throat packs may be placed to prevent blood from entering the stomach and causing nausea and vomiting; monitoring their removal is essential to preventing respiratory obstruction after extubation.
D Endoscopy
a) Endoscopic surgery includes panendoscopy, laryngoscopy, microlaryngoscopy (laryngoscopy aided by an operating microscope), esophagoscopy, and bronchoscopy. All of these procedures can be performed by using a rigid or flexible endoscope. If the rigid laryngoscope is used, the laryngoscope may be suspended from an arching support anchored to the patient’s abdomen or chest or from a Mayo stand over the patient.
b) One of the most common endoscopic procedures performed is endoscopic sinus surgery. Endoscopic sinus surgery is often associated with multiple and seasonal allergies leading to polyps. Patients undergoing surgery are often also being evaluated for such pathology responsible for hoarseness, stridor, or hemoptysis. Other possible reasons for endoscopic examination include foreign body aspiration, papillomas, trauma, tracheal stenosis, obstructing tumors, and vocal cord dysfunction. Several complications can arise with endoscopic surgery; eye trauma, epistaxis, laryngospasm, bronchospasm, and excessive plasma levels of local anesthesia and epinephrine have been reported.
a) Preoperatively, the patient should be examined for any signs of airway obstruction and proper measures taken to ensure safe and controlled airway management. Knowledge of the location and size of a mass is important, and discussion with the surgeon about chest radiography, magnetic resonance imaging (MRI), and computed tomography (CT) scan results can be invaluable.
b) Light sedation is suggested for premedication because older children and adults may experience respiratory depression and worsening of airway obstruction. The airway must be protected from aspiration of gastric contents, especially during prolonged airway manipulation and deeper sedation.
c) Premedication with an antisialagogue to dry secretions and a full regimen of acid aspiration prophylaxis in aspiration-prone patients may be indicated.
d) An awake oral or nasal intubation with minimal sedation and topical anesthesia of the oral cavity, pharynx, larynx, and nasopharynx may be indicated.
e) For shorter ear, nose, and throat (ENT) procedures, anesthesia should be maintained with short-acting inhalation and IV agents to avoid patient movement and vocal cord movement and to control sympathetic nervous system response to brief periods of extreme stimulation as in laryngoscopy.
f) Good muscle relaxation of the vocal cords is an essential part of anesthesia management for microsurgery of the larynx. A short-acting relaxant or infusion may be considered for brief cases.
g) If the procedure is expected to last 30 minutes or more, use of an intermediate-duration neuromuscular blocking drug such as vecuronium, atracurium, cis-atracurium, or rocuronium for the initial tracheal intubation allows the return of muscle strength and spontaneous respiration to meet extubation criteria at the end of the surgical procedure.
h) Emergence should include adequate oropharyngeal suctioning, humidified oxygenation, and observation in the postanesthesia care unit for laryngeal spasm or postextubation croup.
(1) One of the greatest management challenges during endoscopic procedures is to share the airway continuously with the surgeon.
(2) Several methods have been used to provide oxygenation and ventilation during the procedures. One method is to control the airway by using a small cuffed ETT (5.0–6.0 mm for an adult). Because the 5.0- and 6.0-mm ETTs are designed for smaller patients, a better ETT selection might include the microlaryngeal ETT (MLT).
(3) The MLT in similar sizes (5.0–6.0 mm) has a cuff that is larger than the small standard ETTs (5.0–6.0 mm), allowing for a larger cuff distribution across the surface of the trachea and is the same length as an adult sized tube.
(4) There are some distinct advantages of an ETT; these include a secure airway with easily controlled ventilation, a cuff to protect the lower airway from debris, monitoring of end-tidal CO2, and the ability to administer inhalational anesthetics.
(5) Several drawbacks include the potential for extubation and loss of airway, complications during laser surgery, and interference with the operative field by the ETT.
(6) Intermittent apnea is also used as a technique to ventilate patients in this shared space. The anesthesia provider or the surgeon repeatedly removes the ETT, operates during a brief period of apnea, and then allows the anesthesia provider to reintubate and ventilate the patient. One advantage of the technique is that no special equipment is needed to ventilate the patient.
(7) Many of the patients having these procedures have a long history of heavy smoking and alcohol use, which predisposes them to cardiovascular disease and labile vital signs. Some of the disadvantages of this approach include difficulty in reintubation of the patient and the time allotment between ventilations while preventing desaturations. The procedure must be interrupted frequently to ventilate the patient, and the airway is unprotected while the ETT is removed. During this technique, the blood pressure and heart rate tend to fluctuate widely. The procedure resembles a series of stress-filled laryngoscopies and intubations separated by varying periods of minimal surgical stimulation. IV administration or topical application of agents such as lidocaine; small doses of alfentanil, remifentanil, sufentanil, or fentanyl; or β-adrenergic receptor blocking drugs such as esmolol may help moderate the sympathetic response.
(8) After the procedure, suctioning blood out of the stomach will help to decrease nausea and vomiting.
E Foreign body aspiration
Aspiration of foreign bodies is a common problem. There is a high morbidity and mortality, particularly in children, who aspirate foreign objects. Some common aspirants include peanuts, popcorn, jelly beans, coins, and bites of meat and hot dogs. The majority of aspirated items are food particles; however, beads, pins, and small toys are not unusual. A common site of foreign body aspiration is the right bronchus. If the patient is supine when the aspiration occurs, the object will most likely be found in the right upper lobe. If the patient is standing, the right lower lobe is most likely to be affected. Signs of aspiration include wheezing, choking, coughing, tachycardia, aphonia, and cyanosis. These signs indicate an obstructive severe irritation and swelling in the airway. As a result of the swelling, air may be trapped in the lungs, not allowing adequate expiration.
a) The anesthetic management depends on the location of the airway obstruction, the size and location of the object, and the severity of the obstruction. If it is located at the level of the larynx, a simple laryngoscopy with Magill forceps should allow for easy removal of the object.
b) Care must be taken not to dislodge the object and allow the object to fall deeper into the airway. If the foreign body is located in the distal larynx or the trachea, the patient should have an inhalation induction performed in the operating room, maintaining spontaneous respiration. With the patient spontaneously breathing, the surgeon will most likely use a rigid bronchoscope for extraction of the foreign body.
c) A mask induction without cricoid pressure or positive-pressure ventilation is the preferred induction technique. The anesthesia provider should not assist with respirations because this may cause the object to move further into the airway and compromise ventilation with occlusion. Patients should be placed in the sitting position because it is known to produce the least adverse effect on airway symptoms.
d) An antisialagogue, H2 antagonist, and metoclopramide are often administered intravenously to decrease secretions and promote gastric emptying; the secretions may obscure the view through the bronchoscope.
e) Patients with full stomachs who are induced with a rapid sequence must be prepared for complete occlusion of the airway.
f) Direct and sometimes rigid laryngoscopy is typically performed. A rigid bronchoscope is also used and passed through the vocal cords into the trachea. Ventilation is accomplished through a side port of the laryngoscope or bronchoscope that can be attached to the anesthesia circuit.
g) If a foreign body is present, the telescope eyepiece within the bronchoscope is removed and optical forceps are inserted through the bronchoscope for retrieval of the item. While the telescopic eyepiece is being changed, a leak is present in the ventilation system and protracted periods can lead to hypoxia.
h) When an anesthesia gas machine circuit is used, high fresh gas flow rates, large tidal volumes, and high concentrations of inspired volatile anesthetic agents are often necessary to compensate for leaks around the ventilating bronchoscope.
i) Coughing, bucking, or straining during instrumentation with the rigid bronchoscope may cause difficulty for the surgeon and result in damage to the patient’s airway; these must be avoided.
j) The best anesthesia technique for rigid laryngoscopy and bronchoscopy is total IV anesthesia (TIVA), which allows greater control of cardiovascular stability and relaxation for short periods, as well as ventilation with 100% oxygen, which allows longer periods of hypoventilation without hypoxia.
k) A rigid bronchoscopy can lead to several complications, including damage to dentition, gums, and upper lips as well as chipped or damaged teeth, all of which can be prevented to some degree with the use of a mouth guard and vigilance.
l) Vagal stimulation may be noted from the extreme head extension, and tracheal tears can occur with the introduction of the bronchoscope. Inadequate ventilation manifests as hypoxemia, hypercarbia, barotrauma, and dysrhythmias.
m) The surgeon must be prepared to perform an emergency tracheostomy or cricothyrotomy if a partial obstruction suddenly becomes complete.
n) At the conclusion of the procedure, patients can be intubated to provide ventilation until returning to consciousness. Allow the patient to return to consciousness as quickly as possible with airway reflexes intact before extubation.
o) Laryngeal and subglottic edema may occur for 24 hours after removal of a foreign body. To check for airway edema, the cuff of the ETT can be deflated if not contraindicated, and the lumen of the ETT should be occluded for one or two breaths during inspiration and expiration while listening for air movement around the tube. If there is no air escaping around the ETT, postoperative sedation and ventilation might be considered. Dexamethasone can be administered prophylactically to decrease airway edema.
p) Close observation and use of humidified oxygen are suggested during the recovery period. Some additional supportive measures that can alleviate some of the postoperative complications that occur include racemic epinephrine, bronchodilators, and steroids.
F Intraocular procedures
Intraocular procedures may refer to vitrectomy, glaucoma drainage, corneal transplant, and open eye injury. These procedures involve entry into the vitreous humor. It is crucial to avoid increases in intraocular pressure (IOP) with all intraocular procedures.
The most common of these procedures, vitrectomy, is performed by making three openings into the vitreous cavity. One of these openings is used to instill balanced salt solution; another is made for insertion of a fiberoptic light. The third opening is made for the insertion of various instruments used to remove abnormal tissue from the vitreous cavity. Frequently, a gas bubble is introduced during vitrectomy to tamponade retinal tears.
a) History and physical examination: Individualized based on patient’s history and medical condition
(1) Laboratory and diagnostic tests: These are as indicated from the history and physical examination.
(2) Medications: Midazolam, 1 to 2 mg, may be given intravenously in divided doses as a premedication. The anesthesia provider must be aware that ocular drugs applied topically can have systemic effects. These include hypertension, arrhythmias, nausea and vomiting, agitation, excitement, disorientation, seizures, hypotension, and metabolic acidosis.
a) Monitoring equipment is standard.
b) Additional equipment includes standard emergency drugs, a long breathing circuit (table will be turned), and right-angled ETTs.
c) IV fluids: One 18-gauge IV line with normal saline or lactated Ringer solution at 2 to 4 mL/kg/hr is used.
d) A Hudson hood may be used to provide oxygen to the patient if a regional block with sedation is to be used. Care must be taken if there is any electrocautery because the hood will create an oxygen-rich environment under the drape and increase the risk of fire.
4. Perioperative management and anesthetic technique
a) These procedures can be done with the patient under general anesthesia or under a regional block (retrobulbar or peribulbar block) with sedation.
b) General anesthesia with endotracheal intubation is indicated for infants; young children; patients with severe claustrophobia; patients who are unable to cooperate, communicate, or lie flat for long periods; and patients with a history of acute anxiety attacks.
c) Most adult patients do well with a regional block with sedation, which is the preferred anesthetic technique. If this method of anesthesia is used, it is important to determine the patient’s response to sedatives and narcotics before administration of the block. After the table is turned and the patient is draped, it may be difficult to maintain a patent airway or a secure one if necessary. Care must be taken to avoid oversedation. If oversedated, patients tend to be startled when they arouse and may be confused and move about. A short-acting hypnotic (propofol) may be useful immediately before administration of the block. The surgeon needs to have the patient’s cooperation during the block because the surgeon may ask the patient to look from side to side.
d) General ETT anesthesia is also appropriate.
(1) Induction: Standard IV induction. Ketamine is not a drug of choice because increased IOP is to be avoided. Care must be taken to avoid pressure on the eyes with the mask. Nondepolarizing muscle relaxants are used for intubation and continued throughout the procedure titrated to patient response. It is imperative that the patient not move during the procedure. All connections in the breathing circuit should be secured.
(2) Maintenance: Continuous IV anesthesia is an option. Another option is the use of inhalational agents. Nitrous oxide (N2O) may or may not be used. If used, however, and the surgeon performs a gas-fluid exchange, the N2O should be discontinued 5 to 10 minutes before this exchange. Consider an antiemetic because of the high incidence of postoperative nausea and vomiting.
e) Bradycardia and hypotension can be caused by the oculocardiac reflex.
f) Emergence: Smooth emergence and extubation are important. Coughing, bucking, and straining should be avoided to prevent increasing the IOP. Consider deep extubation, although care must be taken not to place pressure on the operative eye with the face mask.
Again, coughing, bucking, and straining should be avoided. The patient may be positioned prone or to one side (as ordered by the surgeon) for correct positioning of the gas bubble. The patient’s respiratory status should be ensured before the patient is turned postoperatively.
G. jet ventilation
Jet ventilation has been used extensively for laryngeal surgery. When the trachea is not intubated, a metal needle mounted in the operating laryngoscope or passed through the cords can be used for jet ventilation. Jet ventilation may be performed manually using a simple hand valve attached to an appropriate oxygen source or with the use of various mechanical devices that allow for adjustment of rate and oxygen concentration. Because oxygen can support combustion, the anesthesia provider should consider as low a concentration of oxygen as is possible. Many patients will tolerate an Fio2 of 30% or less; however, oxygen requirements for each patient should be considered for their individual needs. Also, using lower levels of oxygen will minimize the risk of fire.
a) High-frequency jet ventilation: High-frequency jet ventilation (HFJV) was originally used as a technique to provide adequate oxygenation and alveolar ventilation for rigid bronchoscopy and laryngeal surgery. HFJV is typically ventilation at low tidal volumes with high respiratory rates. A needle connected to a high-pressure hose with a regulator to adjust rate and volume is used to deliver the ventilation. With the tip of the needle either above or below the glottis, the anesthesia provider directs a high-velocity jet stream of oxygen into the airway lumen. The lungs are ventilated as the mixture of oxygen forces air into the lumen. Introduction of high-pressure (up to 60 psi) jet-injected oxygen entrains room air into the lung, allowing the jet stream of gases into the airway for ventilation. Although inspiration is accomplished by HFJV pressurizing gas into the airway, the expiration is passive. Therefore, some pauses in ventilation may be necessary to provide adequate time for expiration, particularly in patients with severe respiratory disease.
If an airway mass lies above the level of delivery of the gas jet, it may be easy to force the gas down the trachea during inspiration. But the gases will be trapped during expiration. This air trapping can lead to increased airway pressure, subcutaneous emphysema, and pneumothorax, particularly in patients with bullae. The anesthesia provider or surgeon may also find it difficult to aim the jet into the airway lumen, leading to hypoxia. If the jet is not accurately aimed, gastric distention, subcutaneous emphysema, or barotrauma may result. Patients with decreased pulmonary compliance or increased airway resistance from bronchospasm, obesity, or chronic obstructive pulmonary disease (COPD) are at high risk for developing hypercarbia with jet techniques. Jet ventilation is contraindicated in any situation in which an unprotected airway is a concern (e.g., full stomach, hiatal hernia, or trauma).
Adequacy of ventilation is assessed by observing chest movement, auscultation with the precordial stethoscope, and a pulse oximeter. TIVA is the primary anesthesia technique used with HFJV because volatile agents cannot be delivered and environmental contamination is a concern. TIVA with short-acting agents such as propofol, alfentanil, fentanyl, and remifentanil provide an excellent anesthetic for these procedures.
H Laryngectomy
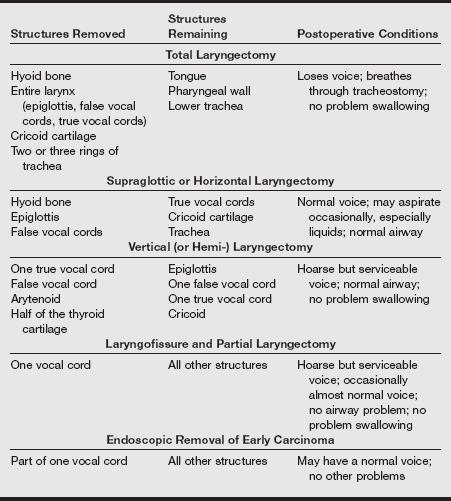
Most cancers of the upper respiratory tract are squamous cell carcinomas. When the laryngeal musculature or cartilage is invaded, total laryngectomy is performed. Intractable aspiration, with resultant pneumonia that has been unresponsive to other treatments, is another indication for laryngectomy.
(1) Total laryngectomy involves removal of the vallecula and includes the posterior third of the tongue if necessary. Surgical exposure is from the hyoid bone to the clavicle. A tracheostomy is performed, and an anode tube is placed. The larynx is usually transected just above the hyoid bone. The trachea is brought out to the skin as a tracheostomy without the need for an ETT or tracheostomy tube as the pharynx is closed.
(2) Supraglottic laryngectomy leaves the true vocal cords by resection of the larynx from the ventricle to the base of the tongue. Surgical exposure is similar to that for total laryngectomy. The specimen includes the epiglottis, the false vocal cords, the supraglottic lesions, and a portion of the base of the tongue. The thyroid perichondrium is approximated to the base of the tongue along with the strap muscles for closure. A temporary tracheostomy is required.
(3) Hemilaryngectomy or vertical partial laryngectomy retains the epiglottis but involves removal of a unilateral true and false vocal cord. Surgical exposure is similar to that of supraglottic laryngectomy, and a tracheostomy is required.
(4) Near-total laryngectomy involves removal of the entire larynx. One arytenoid is used to construct a phonatory shunt for speaking. A permanent or temporary tracheostomy is created, and the procedure may be combined with neck dissection and pharyngectomy with flap reconstruction.
The table below describes the structures removed, structures remaining, and postoperative conditions for the types of surgical procedures.
Most patients are older and have a long history of tobacco and alcohol abuse. Associated medical problems may include COPD, hypertension, coronary artery disease, and alcohol withdrawal.
a) History and physical examination: Individualized
(1) Respiratory: Smoking (more than 40 packs/year) is associated with bronchitis, pulmonary emphysema, and COPD, which impair respiratory function. Arterial blood gases may reveal carbon dioxide retention and hypoxemia. Pulmonary function tests demonstrate decreased forced expiratory volume, forced vital capacity, and the ratio of forced expiratory volume to forced vital capacity. Preoperative airway assessment is imperative because edema may distort airway anatomy, and tumor and edema may cause airway compromise. Tracheal deviation must be considered. Fibrosis, edema, and scarring from prior radiation therapy may distort the airway as well.
(2) Assess for signs of alcohol withdrawal (altered mental status, tremulousness, and increased sympathetic activity).
(3) Gastrointestinal: Weight loss, malnutrition, dehydration, and electrolyte imbalance can be significant.
a) Laboratory tests: Baseline arterial blood gases; electrolytes; hemoglobin; hematocrit; prothrombin time; partial thromboplastin time; and, if indicated from the history and physical examination, hepatic function tests are obtained.
b) Diagnostic tests: Chest radiography, ECG, pulmonary function testing, echocardiography, and stress tests are as indicated from the history and physical examination. Indirect and direct laryngoscopies preoperatively and review of CT may help in planning intubation.
c) Medications: Treatment with a long-acting hypnotic, such as chlordiazepoxide or diazepam, as a precaution for delirium tremens can be considered unless sedation would be contraindicated because of concerns of airway compromise. An IV antisialagogue (glycopyrrolate, 0.2 mg) facilitates endoscopy by the surgeon.
(3) Arterial line: Useful for serial laboratory and arterial blood gas studies
(4) Central venous pressure (CVP) catheter: If indicated by coexisting disease (prefer basilic or cephalic vein)
5. Perioperative management and anesthetic technique
General endotracheal anesthesia is used.
a) Induction: Standard IV induction is appropriate with a normal airway. The choice of an induction drug should be based on the patient’s medical condition. If airway difficulty is possible, direct laryngoscopy can be performed while the patient is breathing spontaneously, and a muscle relaxant may be administered when the glottis is visualized. In more difficult cases, awake intubation or fiberoptic laryngoscopy may be required.
b) Maintenance: The patient is in the supine position, with the head elevated 30 degrees; standard maintenance is used, considering the patient’s preexisting medical problems. An inhalation agent and supplemental narcotics benefit patients with reactive airway disease. Use of nondepolarizing muscle relaxants should be discussed with the surgeon because nerve stimulation for facial nerve localization may be performed.
c) Emergence: Many patients undergo tracheostomy. If a tracheostomy is not performed, the amount of airway edema and distortion needs to be discussed with the surgeon before determining extubation. Gradual emergence with stable hemodynamic parameters is an important consideration in the patient with coronary artery disease.
a) Injury to the facial nerve can cause facial droop. Recurrent laryngeal nerve injury can result in vocal cord dysfunction; diaphragmatic paralysis may result from phrenic nerve injury.
b) Pneumothorax may occur with low neck dissection.
c) Airway impingement results from restrictive neck dressings or hematoma development.
I Laser surgery
Specific issues during ENT surgery are described. The term laser is an acronym for light amplification by stimulated emission of radiation.
The two most common lasers used in ENT surgery are the CO2, Nd:YAG (neodymium-doped yttrium aluminum garnet), and recently the argon laser. Laser light is different from standard light. Whereas standard light has a variety of wavelengths, lasers have only one wavelength (monochromatic); laser light oscillates in the same phase or all of the photons are moving in the same direction (coherent), and its beam is parallel (collimated). The wavelength of the Nd:YAG laser beam is shorter as it passes through the garnet than that of the CO2 laser. The shorter wavelength allows less absorption by water and therefore less tissue penetration. For example, whereas the shorter wavelength of the Nd:YAG allows the laser light to pass through the cornea, the longer wavelength of the CO2 laser would burn the cornea.
Laser light emits a small amount of radiation and can be infrared, visible, and ultraviolet in the spectrum. Lasers enable very precise excision, produce minimal edema and bleeding, and are favored by surgeons for resection of tumors and other obstructions of the airway. For operations in and around the larynx, the CO2 laser is most often used because of its shallow depth of burn and extreme precision. The CO2 laser produces a beam with a relatively long wavelength that is absorbed almost entirely by the surface of these tissues, vaporizing cellular water. Intermittent bursts of the CO2 laser produce intense, precisely directed energy that results in a clean cut through the target tissue with minimal amount of penetration of surrounding tissue. A low-energy helium–neon laser is commonly used to aim or direct CO2 laser beams.
Compared with the CO2 laser, the Nd:YAG laser is poorly absorbed by water but easily absorbed by hemoglobin and pigmented tissues. The Nd:YAG laser light is capable of producing deep tissue penetration that may not be apparent for hours or days after exposure to the laser. The Nd:YAG laser allows debulking of larger tumors within body cavities. For this reason, the Nd:YAG laser is best suited for resection of bronchial, esophageal, bladder, hepatic, and splenic tumors. Laser light beams are primarily used for their thermal effect and can be used to cut, coagulate, or vaporize tissues. The exact tissue interaction of a laser is dependent on several variables, including the types of tissues being irradiated, the wavelength of the emitted beam, and the power of the beam.
a) Safety guidelines: The use of laser technology mandates taking measures to ensure the safety of the patient and operating room personnel. These measures are listed in the box below. Specific concerns include eye protection with appropriate colored glasses, avoidance of the dispersion of noxious fumes, and fire prevention. Stray or reflected beams of the Nd:YAG laser are capable of traversing the eye to the retina; therefore, green-lensed eye protection for all personnel is mandatory during its use. All persons in the operating room must wear goggles specifically designed to absorb Nd:YAG laser beams. The required protective eyewear for CO2 can be any clear glass or plastic that surrounds the face. Orange-red eye protection is required for the potassium-titanyl phosphate (KTP) laser and orange glasses for the argon laser.
When tissues are cut by a laser, the smoke and vapors that are formed are called laser “plume.” This plume is an environmental concern and potentially toxic to operating room personnel. When the tissues vaporized by the laser are malignancies or viral papilloma, the concern arises as to whether these vapors are even more dangerous to operating room personnel if not removed from the environment. Because this issue remains under investigation, it is judicious to suction the laser plume and not allow it to circulate into the room.
a) The prevention of combustion within the airway is of primary concern to the anesthesia provider. Fire in the airway is relatively uncommon (0.4%), and it is usually caused by penetration of the laser through the ETT, which exposes the beam to a rich oxygen supply.
b) N2O, although not flammable, also supports combustion and can propagate the flame. Positive-pressure ventilation in the presence of intraluminal combustion produces a blowtorch effect with serious damage to the respiratory tract of the unfortunate patient. An Fio2 of 30% or less is recommended for laser surgery that takes place in the airway.
c) Steps to reduce the possibility of fire include using the lowest concentration of oxygen appropriate for a particular patient, avoiding paper surgical drapes, spraying the flame with a 60-mL syringe filled with normal saline, and using water-based rather than oil-based lubricants.
d) When a flame has been ignited, extinguish the flame, discontinue oxygen administration, and immediately remove the ETT and replace it with a new ETT large enough to allow the surgeon to assess the lungs with a bronchoscope. The advantages and disadvantages of ETTs for use with lasers are listed in the following table.
Advantages and Disadvantages of Commonly Available Laser-Resistant Tracheal Tubes
| Tube Type | Advantages | Disadvantages |
| Metal | Atraumatic external surfaceDouble cuff maintains seal even if punctured by laser Kink resistant |
Thick-walled nonflammable cuff reflects laser and transfers heatCuff difficult to deflate if punctured Metal may reflect beam onto nontargeted tissue |
| Polyvinyl chloride (PVC) | InexpensiveNonreflective Maintains shape well Double cuff maintains seal after proximal cuff puncture |
Burns vigorously and yields pulmonary toxin (hydrogen chloride)Cuffed version contains flammable material |
| Red rubber | Wrapping protects flammable material but dries tubeMaintains structure Nonreflective |
Red rubber itself is highly flammableTubes are thick walled |
| Silicone rubber | Wrapping protects flammable materialMethylene blue aids in detection of cuff perforation Nonreflective |
Contains flammable materialTurns to toxic ash Single cuff is vulnerable to laser damage |
J Le fort procedures
a) The usual preoperative diagnosis for patients with maxillary fractures is facial trauma. Le Fort fractures are frequently associated with other skull fractures, zygoma fractures, and possible intracranial fractures and thus with cerebrospinal fluid rhinorrhea.
b) The fractures are divided into Le Fort I, II, and III. The Le Fort I fracture is a horizontal fracture of the maxilla extending from the floor of the nose and hard palate through the nasal septum and through the pterygoid plates posteriorly. The palate, maxillary alveolar bone, lower pterygoid plate, and part of the palatine bone are all mobilized. The Le Fort II fracture is a triangular fracture running from the bridge of the nose through the medial and inferior wall of the orbit beneath the zygoma and through the lateral wall of the maxilla and the pterygoid plates. The Le Fort III fracture totally separates the midfacial skeleton from the cranial base, traversing the root of the nose, the ethmoid bone, the eye orbits, and the sphenopalatine fossa.
2. Preoperative assessment and patient preparation
The airway is a priority. If the airway cannot be managed, emergency intubation becomes necessary. Avoid blind nasal intubation in patients with cerebrospinal fluid rhinorrhea, periorbital edema, “raccoon’s eyes” bruising, or other evidence of nasopharyngeal trauma.
a) Neurologic: Document any neurologic deficit; intracranial trauma may require invasive monitoring.
b) Laboratory tests: Hematocrit and any other tests are as indicated by the history and physical examination.
a) Monitoring equipment: Standard
b) Additional equipment: Fiberoptic cart, a long breathing circuit (the table will be turned 180 degrees)
d) IV fluids: One 18-gauge line with normal saline or lactated Ringer solution at 6 to 8 mL/kg/hr
4. Perioperative management and anesthetic technique
General endotracheal anesthesia is used.
a) Induction: Fiberoptic laryngoscopy should be performed if there is any doubt about the ease of intubation. Patients with mandibular and maxillary (Le Fort I and II) fractures should undergo intubation. Patients with nasal, orbital, or zygomatic fractures usually are intubated orally. Consider using anode or right-angled ETTs. A Le Fort type II or III fracture is a relative contraindication for nasal intubation or nasogastric tube placement.
(1) Muscle relaxation is usually required. Consider the prophylactic use of antiemetics for patients with wired jaws.
(2) Position: The patient is supine; check and pad pressure points. Avoid stretching the brachial plexus, and limit abduction to 90 degrees. Protect the patient’s eyes with ophthalmic ointment.
(3) Blood loss can become significant. Intraoperative measurement of hemoglobin and hematocrit is necessary.
(4) Administration of dexamethasone is frequently requested by the surgery.
c) Emergence: Extubation should be performed when the patient is fully awake in the case of difficult airway or wired jaws. A wire cutter should be available at all times. Verify that throat packing has been removed before extubating. Patients with facial or airway swelling and those involved in multiple trauma may need continued postoperative intubation and ventilation. An orogastric tube should be inserted to the stomach to suction blood before jaw wiring.
K Maxillofacial trauma
Traumatic disruption of the bony, cartilaginous, and soft tissues of the face and upper airway challenge the anesthesia provider to recognize the nature and extent of the injury and consequent anatomic alteration. It is imperative to create an anesthetic plan for securing the airway without promoting further damage or compromising ventilation. Possible mechanisms by which the upper or lower airway may become obstructed include edema; bleeding from the oral mucosa and palate; intraoral fracture sites; the presence of foreign bodies such as avulsed teeth, blood clots, or bony fragments; distortion of the nasal passages; injury of the pharynx and sinuses; and open lacerations.
Two common causes of maxillofacial fractures are blunt and penetrating trauma and gunshot wounds. Because of the intense forces required to cause facial fractures, other traumas (e.g., subdural hematoma, pneumothorax, cervical spine injury, and intraabdominal bleeding) often occur simultaneously with these fractures.
a) Initial management of the airway depends on the situation at hand. In the case of severe facial or neck trauma, alternative methods of tracheal intubation such as fiberoptic laryngoscopy, retrograde wire placement, jet ventilation via a cricothyrotomy, or emergent tracheostomy may be necessary to secure the airway.
b) Injuries of the head and neck should alert the anesthesia provider to possible cervical spine injury. Although a complete evaluation of all cervical vertebrae is ideal, inspection of a lateral radiograph of the cervical spine is judicious to determine the presence or absence of dislocations and fractures. All seven cervical vertebrae must be visible. The seventh cervical vertebra is the most common site for traumatic fracture of the spine. Physical assessment is also required to rule out the presence of neck injury. Pain, deformation, and range of motion after radiographic studies are confirmed to be normal are also ceased.
c) Vertebral artery injury must be suspected with a cervical injury because these fractures can lead to vertebral artery tear or occlusion. If deteriorating respiratory function requires immediate airway management and intubation, the head should be maintained in a fixed position before any manipulation of the airway is performed. The use of manual in-line axial stabilization (MAIS) (by a qualified assistant) or a rigid cervical collar in place is recommended. The removal of the anterior segment of the collar can facilitate intubation and manipulation of the soft tissues of the neck.
d) Blunt trauma to the face or anterior neck may produce rapid airway occlusion secondary to soft tissue edema or hematoma formation secondary to trauma of the vascular structures of the neck. If a hematoma is discovered in the vascular structures of the neck, an ENT surgeon must be notified immediately. A patient exhibiting smoke or blistering in the area of the mouth and nares or with a history of inhalation of toxic byproducts of combustion should be intubated immediately. Edema of the face and glottis, which may lack symptoms in the early stages, has the potential to produce serious airway compromise several hours after injury. Securing the airway by either oral or nasal intubation is preferable to tracheostomy, which is associated with a higher incidence of complications. It is imperative to avoid intubation in patients who may have sustained a basilar skull fracture.
L Myringotomy and tube placement
A myringotomy allows the pressure to equalize between the middle ear and the atmosphere, reducing the pressure in the middle ear compartment. Simple tubes with a lumen are placed through the patient’s tympanic membrane to alleviate the pressure created in the middle ear usually seen with chronic serous otitis media or recurrent otitis media. These tubes function as an escape for the ostium and enable nonstop drainage of this pressure. Chronic otitis media is manifested as fluid in the middle ear. Recurrent otitis media, a common pediatric disorder, is defined as six or more episodes of otitis media over the prior year. Untreated otitis media may lead to permanent middle ear damage and hearing loss; therefore, prompt treatment is necessary. Children with chronic otitis media frequently have accompanying recurrent upper respiratory infections (URIs). Intervals between URIs may be brief. The patient is usually on a regimen of antibiotics. Thus, scheduling surgery during these interludes is often impractical. Often the eradication of middle ear fluid and inflammation resolves the URI; therefore, surgery should not be delayed.
a) Bilateral myringotomies with tube insertions are typically very short operations.
b) Sedative premedications may outlast the procedure and are usually not necessary.
c) Mask or IV induction and maintenance using oxygen, N2O, and agent such as sevoflurane is routinely used.
d) If IV access is established, it is usually after mask induction in children and may include fluid therapy or an injection cap for temporary access and administration of drugs. Because most patients scheduled for myringotomics are young and healthy, IVs are not usual necessary unless another procedure is performed in addition to positron emission tomography.
e) N2O is often avoided in surgeries that involve the middle ear because it is 34 times more soluble in blood than nitrogen and can create pressure in the closed space. Because the myringotomy surgical procedure is relatively short and a tube will be placed through the tympanic membrane into the middle ear to relieve the pressure, the effects of N2O are often not relevant.
f) For bilateral procedures, the inhalation anesthetic is discontinued during the second myringotomy to facilitate prompt emergence. N2O is continued until the completion of the surgery.
g) Intubation is performed only if airway difficulties are anticipated or encountered. However, the airway equipment is always prepared and available. The procedure is typically short and without much risk of bleeding.
h) The patient is supine with the head turned to expose the ear to the microscope. An ear speculum is inserted into the ear canal, cerumen is removed, and an incision is made in the tympanic membrane. Fluid is sometimes suctioned from the middle ear. Then a tympanostomy tube is inserted through the incision into the middle ear, straddling the tympanic membrane.
i) Upon completion of the tube insertion, antibiotic and steroid eardrops frequently are inserted into the external auditory canal. The surgeon moves to the other side of the table, the microscope is repositioned, the head is turned, and the procedure is repeated in the other ear.
M Nasal surgery
Nasal surgery is often performed to restore the caliber of the nasal airway or for cosmetic purposes. Whether for rhinoplasty, septoplasty, or septorhinoplasty, the nasal cavity can be anesthetized by placing 4% cocaine–soaked pledgets up each nostril for 5 to 10 minutes. To ensure vasoconstriction and minimize bleeding, the site is infiltrated with 1% lidocaine and 1:100,000 epinephrine. A hypertensive technique may also be initiated to control bleeding.
An incision is made in the septum down to the cartilage with elevation of a submucoperichondrial flap. This may be repeated on the contralateral side. Bone and cartilaginous deformities may be resected or weakened on the face. They may also be removed first, shaped, and then replaced. When the surgeon is satisfied with the resection, the incision is closed with an absorbable suture. In rhinoplasty, depending on the area needing work, the nasal contours can be remodeled by tip remodeling, humps can be reduced, bone osteotomies can be performed to shape the contour of the nose, or combinations thereof can be done. After surgery, both nasal cavities are packed, and external splints may be used.
2. Preoperative assessment and patient preparation
Generally, these procedures are elective and can be performed on an outpatient basis. It is important to identify patients with obstructive apnea. These patients often have chronic airway obstruction, redundant pharyngeal tissues, or both. Such patients, as well as patients with asthma, should undergo arterial blood gas and pulmonary function testing. Ketorolac and acetylsalicylic acid should be avoided in patients who also have nasal polyps because they often are hypersensitive to acetylsalicylic acid, a condition that can precipitate bronchospasm.
a) History and physical examination: Carefully evaluate cardiovascular status because the use of local vasoconstrictors may cause dysrhythmia, coronary artery spasm, hypertension, and seizures.
a) Monitoring equipment: Standard
b) Additional equipment: Regular operating table, turned 90 to 180 degrees; anesthesia circuit extension available
d) IV fluids: Two 18-gauge lines with normal saline or lactated Ringer solution at 4 to 6 mL/kg/hr
4. Perioperative management and anesthetic technique
Use general endotracheal or local anesthesia with sedation; the choice depends on the preferences of the surgeon and the patient as well as on the acetylsalicylic acid status of the patient.
a) Induction: Routine. Use of an oral right-angled ETT is convenient for the surgeon but is not necessary. If a sedation technique is chosen, short-acting agents are best because these procedures are usually minor, and patients are usually sent home.
c) Emergence: Counsel patients that the nose will be packed with bandaging and possibly splinted, so mouth breathing will be necessary on awakening. To decrease the incidence of coughing during extubation, lidocaine may be given.
N Open-eye procedures
Intraocular pressure is determined by the balance between production and drainage of aqueous humor and by changes in choroidal blood volume. Resistance to outflow of aqueous humor in the trabecular tissue maintains IOP within physiologic range. Normal IOP is 12 to 16 mmHg in the upright posture and increases by 2 to 3 mmHg in the supine position.
When the globe is open, the IOP is equal to ambient pressure. If the volume of choroid and vitreous should increase while the eye is opened, the vitreous may be lost. Any deformation of the eye by external pressure on the globe will cause an apparent increase in intraocular volume. This discussion is of open-eye procedures.
2. Preoperative assessment and patient preparation
a) History and physical examination: Standard; the patient may come in as an emergency with a full stomach; ensure that the patient has no other injuries.
b) Diagnostic and laboratory tests: These are as indicated by the history and physical examination.
c) Preoperative medication and IV therapy
(1) Aspiration prophylaxis is used.
(2) Atropine or glycopyrrolate reduces oral secretions and may inhibit the oculocardiac reflex.
(3) Avoid narcotics, which may cause nausea and vomiting.
(4) Sedatives are given in the preoperative hold area and are titrated to effect.
(5) One 18-gauge IV tube with minimal fluid replacement is used.
a) Monitoring equipment: Standard
b) Pharmacologic agents: Standard; lidocaine and atropine
c) Position: Supine; the table may be turned for the surgeon’s access
4. Anesthetic technique and perioperative management
General anesthesia with endotracheal intubation because a retrobulbar block causes a transient rise in IOP, which may cause intraocular contents to be expelled.
(1) The goal is to avoid increasing IOP.
(2) When preoxygenating, avoid pressing the face mask onto the eyeball.
(3) Awake intubation is contraindicated because it may cause coughing and bucking.
(4) IV lidocaine, 1 mg/kg, may eliminate coughing and bucking.
(5) The use of succinylcholine in open eye globe injuries is controversial. If the use of succinylcholine is necessary, administration of a defasciculatiing dose of a nondepolarizing agent is warranted; it is a safe combination for rapid-sequence induction in the open eye in a patient with a full stomach.
(6) Induction may be with propofol and a large dose of a nondepolarizing muscle relaxant.
(7) Use of ketamine is contraindicated; it causes a moderate increase in IOP and nystagmus or blepharospasm.
(1) Inhalation agents cause dose-related decreases in IOP; the degree of IOP reduction is proportional to the depth of anesthesia.
(a) This is caused by traction on the extraocular muscles (medial rectus), ocular manipulation, or manual pressure on the globe.
(b) Signs and symptoms are bradycardia and cardiac dysrhythmias.
(c) Treatment is to stop surgical stimulus, ensure that dysrhythmia is not the result of hypoxia (by oxygen saturation confirmation) or ventilation, and administer atropine if needed.
(1) The goal is to avoid excessive coughing and bucking.
(2) Empty the patient’s stomach with a nasogastric tube and suction the pharynx while the patient is still paralyzed or deeply anesthetized.
(3) Administer an antiemetic before the end of surgery.
(4) Administer lidocaine, 1 mg/kg, to prevent coughing during emergence.
(5) Extubate the trachea before the patient has a tendency to cough.
O Orbital fractures
Surgical access to the orbit may be needed to repair orbital fractures. The orbit may be divided into several compartments, including the peripheral surgical space, subperiosteal space, central surgical space, and subtenon space. The approach for orbital wall fractures depends on the location and the pathologic process involved. The common approach to these fractures is the transperiosteal or extraperiosteal approach. A skin incision is made in the desired quadrant just outside the orbital rim. The periosteum is identified and incised and is then resected from the wall and orbital margin.
2. Preoperative assessment and patient preparation
a) History and physical examination: Patients are usually healthy aside from the underlying trauma. Evaluation should focus on any coexisting disease and systemic manifestations of the trauma.
b) Laboratory tests: As indicated by the history and physical examination
c) Diagnostic tests: As indicated by the history and physical examination
a) Monitoring equipment: Standard
b) Additional equipment: Regular operating table that is turned 90 to 180 degrees; availability of an anesthesia circuit extension is required
c) Drugs: Standard emergency and standard tabletop
d) IV fluids: One 18-gauge IV line with normal saline or lactated Ringer solution at 4 to 6 mL/kg/hr
4. Perioperative management and anesthetic technique
a) Use general endotracheal anesthesia for patients with orbital fractures identified as Le Fort II or III; nasal intubation is contraindicated.
b) Induction: Standard; an oral right-angled ETT may be preferred.
c) Maintenance: Standard; muscle relaxation is not required.
d) Position: Supine; check and pad pressure points. The table is turned 90 degrees; have extension tubes or long tubes for an anesthesia circuit. Check the patient’s eyes and tape or use ointment (or do both).
(1) Oculocardiac reflex is triggered by pain, direct pressure on the eye, and pulling on the extrinsic muscle of the eye. It has both trigeminal afferent and vagal efferent pathways. Bradycardia caused by the oculocardiac reflex is the most common manifestation, although junctional rhythm, atrioventricular block, ventricular premature contractions, ventricular tachycardia, and asystole also can occur.
(2) To treat, tell the surgeon to stop the stimulus, ensure adequate oxygenation and ventilation, evaluate the depth of anesthesia, and administer atropine as needed. Lidocaine infiltration near the eye muscles may help to attenuate the reflex, which is self-limiting (i.e., it will tire itself with repeated manipulations).
P Orthognathic surgery
Orthopedic orthognathic procedures often require a sagittal splitting of the mandible to move the lower jaw either forward or back. A Le Fort I or Le Fort II osteotomy may be performed to move the maxilla in any direction to correct anomalies. Many of these patients have anomalies of the mandible and maxilla, small mouth openings, and appliances that make intubation difficult and airway management challenging.
a) Because most of the malocclusions are treated orally, a nasal ETT is usually preferred over an oral intubation. Securing the nasotracheal tube away from the surgical field without causing necrotic injury of the nares is vital.
b) Blood loss during these procedures can be extensive; the patient is typed and crossmatched and deliberate hypotensive anesthetic techniques are often used.
c) Rigid external or internal fixation devices are used to maintain stability in both the mandible and maxilla postoperatively; therefore, the proper cutting tools should be at the patient’s bedside for emergency airway issues.
d) The anesthesia provider must also consider that edema will many times be extensive and progress over the first 24 hours after orthognathic surgery. To prevent postoperative respiratory problems, the patient may remain intubated for several days. If extubation is necessary, it should only be done when the patient is awake and in full command of his or her reflexes. Suctioning the stomach to remove blood and providing antiemetics can help the incidence of postoperative nausea and vomiting.
Q Ptosis surgery
If ptosis is severe, the function of the levator palpebrae is poor. Most frequently, ptosis surgery involves shortening or reattaching the muscle at its site of insertion on the superior tarsus. The upper eyelid is marked at the desired height so it matches the opposite eyelid. Local anesthetic is injected by the surgeon. The skin is incised along the upper eyelid crease, and dissection proceeds until the orbicularis oculi is reached. At the medial and lateral ends of the tarsus, scissors incisions are made, and a clamp is placed between the two incisions. The levator muscle is resected as desired, and the eyelid height is evaluated. The skin incision is then closed, with any excess being excised.
2. Preoperative assessment and patient preparation
a) This type of procedure in adults is preferably performed using local anesthesia so the patient can keep the eyes open and the eyelid position can be adjusted.
b) History and physical examination are routine.
(1) Laboratory tests: As indicated by history and physical examination
(2) Diagnostic tests: As indicated by history and physical examination
(3) Premedication: Light sedation as needed
(4) IV fluids: One 18- or 20-gauge needle with normal saline or lactated Ringer solution; keep vein open; blood loss is normally minimal
3. Perioperative management and anesthetic technique
a) Patients are kept awake such that they are able to open their eyes to facilitate adjustment of the eyelids.
b) Deep sedation is required for only localization; then the patient is kept awake.
c) Patients are positioned upright or supine with the ability to sit upright during surgery. The table is rotated 90 to 180 degrees.
R Radical neck dissection
Radical neck dissection is required when cancerous tumors have invaded the musculature and other structures of the head and neck. These tumors are often friable and bleed readily. These patients are frequently heavy drinkers and smokers who have bronchitis, pulmonary emphysema, or cardiovascular disease. If the tumor interferes with eating, then weight loss, malnutrition, anemia, dehydration, and electrolyte imbalance can be significant. Patients who have had radiation treatments of the neck and jaw before surgical intervention will have soft tissues that are less mobile, making intubation more difficult. Many of these patients are older. The number of complications in patients age 65 years and older is nearly double that of younger patients. Consultation with a surgeon as to the nature, extent, and location of the tumor; therapy administered (radiation or chemotherapy); CT results; history and physical examination; and so on remains important in determining the appropriate techniques for airway management.
Head and neck reconstruction is an integral part of surgical removal of head and neck tumors. Traditional methods of reconstruction include regional pedicle flaps with microvascular reconstruction. These flaps include pectoralis major myocutaneous flap; trapezius flap; and local rotational flaps, such as forehead flap. Additionally, small bowel may be harvested to reconstruct the oropharynx and esophagus. The anesthesia team plays an important role in maximizing the overall success rate of a free flap and microvascular flow of the flap. The anesthesia provider must communicate with the surgeon regarding the planned donor site, which limits the available sites to place lines necessary for monitoring and venous access. Although the choice of monitoring is largely dependent on the general condition of the patient, the placement of a CVP line, a Foley catheter, and an arterial line (beat-to-beat and arterial blood gas trends) is suggested, particularly if deliberate hypotension during anesthesia is used. A pulmonary artery catheter may be useful if a history of cardiac problems is present. The internal jugular approach should be avoided because of proximity to the surgical site. Sites commonly used for CVP and pulmonary catheter placement when the internal jugular is not accessible are the subclavian and femoral veins, respectively.
a) Maintenance of anesthesia is often performed with an inhalation agent and supplemental narcotics. The use of a nondepolarizing muscle relaxant should be discussed with the surgical team preoperatively because the surgeon frequently uses a nerve stimulator to locate nerves distorted by the tumor during the procedure.
b) Significant blood loss can be a problem, so hypertension should be avoided and treated aggressively. Sometimes a controlled hypotension technique may be requested. At least one (and preferably two) large-bore peripheral IV lines (14 to 16 gauge) should be in place. The patient’s blood should be typed and crossmatched, with blood readily available. Monitoring estimated blood loss and measuring the hematocrit may provide some guidelines for replacement of blood.
c) A positive fluid balance in the postoperative phase can result in edema and congestion of the flap, predisposing it to vascular compromise. Colloids may be used to help limit the amount of crystalloid required during the procedure. Patients undergoing a radical neck dissection are frequently hypovolemic and have electrolyte imbalances. This requires some fluid replacement and electrolyte balance intraoperatively to maintain cardiovascular stability.
d) In preparation for a tracheostomy or total laryngectomy to be performed during the surgical procedure, the patient should receive 100% oxygen. The trachea will be transected by the surgeon, which requires that the anesthesia provider suction the airway and remove the ETT only to a level above the tracheal incision. After the tracheostomy tube has been placed by the surgeon and ventilation validated, the ETT can then be completely removed. A reinforced tube is usually placed in the distal airway by the surgeon and connected to the anesthesia machine. A reassessment of the ventilation should be performed, including the entire procedure of listening to bilateral breath sounds and observing chest excursion, end-tidal CO2, and positive inspiratory pressure or negative inspiratory pressure. After the anesthesia provider has validated tube placement, the ETT is sutured to the chest wall for the entire surgical duration. At the end of surgery, the reinforced tube may be switched for a tracheostomy cannula.
e) During radical lymph node dissection of the neck for carcinoma, manipulation of the carotid sinus may elicit a vagal reflex, causing bradycardia, hypotension, or cardiac arrest. Small doses of local anesthetic injected near the carotid sinus or administration of an anticholinergic agent may block vagal reflexes.
f) Due to the long duration of the surgery and interruption of venous flow, venous thrombus is commonly seen in patients who are undergoing radical neck dissection. Venous air embolism may also occur during radical neck dissection from the head-up position and open neck veins during surgery. Careful monitoring with precordial Doppler sonography or transesophageal echocardiography provides the best detection of air embolism. Immediate removal of the air through the CVP is essential.
g) Laryngeal edema, vascular occlusion, and obstruction can also occur as a result of the venous stasis that follows major disruptions in venous flow during surgery or with trauma. Continuous review of complications and follow-up treatments are necessary.
h) Postoperative considerations consist of tracheostomy care; controlled ventilation; chest radiography to rule out pneumothorax, hemothorax, and pulmonary edema; and monitoring for laryngeal edema induced by thrombosis. It is suggested that these patients be admitted overnight in the intensive care unit because they have undergone major fluid and electrolyte shifts and altered ventilation–perfusion status and have spent an extensive time under the influence of anesthesia.
S Rhytidectomy or facelift
Rhytidectomy is a reconstructive plastic procedure in which the skin of the face and neck is tightened, wrinkles (rhytid) are removed, and the skin is made to appear firm and smooth. In the preoperative area, the surgeon marks where the planned incisions will be made; before incision, the surgeon localizes the area. Typically, lidocaine 1% with 1:100,000 epinephrine is infiltrated along the incision lines, and lidocaine 0.5% with 1:400,000 epinephrine is infiltrated into the anticipated dissection line.
The facelift incision begins in the temporal scalp area about 5 cm above the ear and 5 cm behind the hairline, curves down parallel to the hairline toward the superior root, and continues caudally in the natural preauricular skin crease. The dissection begins in the temporal hair-bearing area; dissection continues through temporoparietal fascia and down to the loose areolar layer. The facial nerve branches and enters the facial muscles on their deep surface; dissection during this procedure must be done carefully. The only large sensory nerve that is important is the great auricular nerve. This nerve crosses the surface of the sternocleidomastoid muscle below the caudal edge of the auditory canal and is found posterior to the external jugular.
2. Preoperative assessment and patient preparation
a) History and physical examination
(1) Most patients are older and have some effects of aging, but the age range may be anywhere from 40 to 70 years. Therefore, cardiovascular status should be evaluated because of the use of epinephrine in the local anesthetic.
(2) Because of the inaccessibility of the face to the anesthesia provider and the need for sedation, careful airway evaluation and a history of sleep apnea should be identified.
a) Monitoring equipment is standard, including an end-tidal carbon dioxide nasal cannula or a second nasal cannula attached to the capnograph.
b) Additional equipment: An extra long anesthesia circuit should be available because of the turning of the table 90 to 180 degrees, and an oral right-angled ETT is indicated if general anesthesia is to be used.
c) Drugs: Standard emergency and standard tabletop agents are used.
d) IV fluids: Because of the use of vasoconstrictors in local anesthesia, blood loss should be minimal.
e) One 18-gauge IV line with normal saline or lactated Ringer solution at 2 mL/kg/hr is used or the vein is kept open with replacement of the NPO (nothing by mouth) deficit.
4. Perioperative management and anesthetic technique
a) Most facelifts are done with deep sedation. The surgeon needs the patient to remain asleep throughout the procedure.
b) The choice depends on the patient and surgeon’s preference.
c) If a general anesthetic technique is chosen, an oral right-angled ETT may be used to facilitate exposure of the surgical field.
d) If a local anesthetic with IV sedation is the technique chosen, a nasal airway may be placed if the patient easily obstructs.
e) Induction: Routine. If a local anesthetic with sedation is chosen, a short-acting agent (i.e., propofol) should be used because most of these surgical procedures are done on an outpatient basis with the patient going home the same day.
f) Before administration of local anesthetic, the patient must be motionless and deeply sedated.
g) Maintenance: Routine. Deep sedation can be maintained with an infusion. Hypertension should be controlled because this may result in hematoma. Vital signs should be maintained within normal limits. Depending on the patient’s anatomy and the skill and experience of the surgeon, this procedure could last up to 6 hours. The surgeon may perform facial nerve monitoring. If so, paralysis should be avoided with a general anesthetic technique.
h) Emergence: If a general anesthetic is used, emergence should be smooth, preventing coughing and bucking to limit the risk of hematoma formation.
a) Hematoma is the most common complication of this procedure, usually occurring at the end of the procedure, but it may also present within the first 10 to 12 hours.
(1) The cause of this is usually intraoperative hypertension.
(2) This complication most commonly presents itself with the patient’s appearing restless and having unilateral pain to the face or neck.
(3) However, if these symptoms are noticed, the surgeon should be notified because treatment must be surgical.
(4) If left untreated, this could compromise the patient’s respiratory status.
(5) A general anesthetic technique or IV sedation technique may be done for evacuation of the hematoma. If the hematoma is large, a general technique may be performed if the patient is restless and anxious.
b) This procedure disrupts branches of the sensory nerves to the face. Numbness may last several months postoperatively, usually 2 to 6 months. The numbness is usually limited to the area of the lower two-thirds of the ear, the preauricular area, and the cheeks.
c) Nausea and vomiting can contribute to hematoma formation, so prophylaxis should be administered. Dexamethasone 4 to 8 mg is often used and has the additional benefit of reduced swelling. A serotonin receptor is also commonly administered.
T Sinus and nasal procedures
Sinus and nasal procedures for drainage of chronic sinusitis, polyp removal, repair of deviated septum, or closed reduction of fractures generally involve a young and healthy patient population. Many of the patients having sinus and nasal surgery have chronic environmental and drug allergies; therefore, there is an increased incidence of reactive airway disease in these patients. The use of fiberoptics or functional endoscopic sinus surgery for nasal and sinus surgery is indicated for treatment of chronic sinusitis.
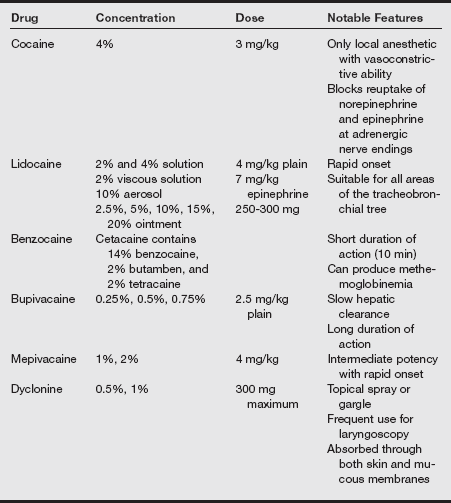
a) Nasal surgery may be successfully accomplished with local, monitored anesthesia care, or general anesthesia. All three methods of anesthesia require profound nasal vasoconstriction. The mucous membranes of the sinuses and nose are highly vascular, and blood loss may be significant if vasoconstriction is not used. The surgeon may select to control vasoconstriction with epinephrine or cocaine, as shown in the table on pg. 339.
b) The anesthesia provider may be asked to use a hypotensive technique or slight head elevation (10–20 degrees) during the procedure. Using general anesthesia has been associated with an increased blood loss even with the use of an epinephrine injection. This exaggerated blood loss may be related to the vasodilatory properties of the inhalation agents.
c) Delivering general anesthesia for sinus surgery with propofol as well as other IV anesthetic techniques for the maintenance of anesthesia has been associated with less blood loss than occurs with the use of volatile agents for maintenance.
d) The placement of an oropharyngeal pack and light suctioning of the stomach at emergence may attenuate postoperative retching and vomiting. After all of the packing is removed, extubation should be performed on the awake patient who has regained control of protective reflexes. The use of IV or topical lidocaine may reduce some of the coughing before extubation, reducing bleeding in the postoperative period.
U Strabismus repair
Strabismus repairs are performed to correct ocular malalignment. This malalignment may be esotropia (eyes deviate inward) or exotropia (eyes deviate outward). This procedure straightens the eyes cosmetically and allows the patient binocular vision by the lengthening or shortening of individual muscles or pairs of muscles. The specific muscles involved are the horizontal rectus and the oblique muscles.
A forced duction test is performed by the surgeon after induction and intubation by manipulating the sclera of the operative eye to aid the surgical plan. An incision is made through the conjunctiva in the area of the muscle to be manipulated. The muscle is then isolated and sewn back farther on the globe if the muscle tension is to be increased. If the muscle tension needs to be decreased, a segment of the muscle is removed.
Strabismus repair is the most common ophthalmic surgical procedure performed on children. These children are usually otherwise healthy. There is, however, a higher incidence of strabismus in children with cerebral palsy and myelomeningocele with hydrocephalus. Malignant hyperthermia also is more common with children undergoing strabismus repair.
a) History and physical examination
(1) A careful family history should be obtained preoperatively, including any history of family problems with anesthesia.
(2) Respiratory: For patients with signs and symptoms of an acute respiratory infection, surgery should be postponed because these children are at greater risk for laryngospasm and bronchospasm.
(1) Laboratory tests: These are as indicated by the history and physical examination. Caffeine and halothane contracture tests may be indicated if the patient is believed to be susceptible to malignant hyperthermia.
(2) Diagnostic tests: As indicated by the history and physical examination
(3) Medications: Midazolam, 0.5 to 0.7 mg/kg orally, is given as a premedication.
4. Perioperative management and anesthetic technique
a) Induction: General endotracheal anesthesia is the technique of choice. Nondepolarizing muscle relaxants may be used after the forced duction test is performed by the surgeon. Bradycardia is common owing to the oculocardiac reflex, so atropine is commonly indicated. If the oculocardiac reflex occurs, ask the surgeon to stop ocular manipulation and reassess anesthesia depth and hemodynamic stability before proceeding with the procedure.
b) Maintenance: Routine. Watch for signs and symptoms of malignant hyperthermia.
c) Emergence: Nausea and vomiting are very common. Prophylactic antiemetics are recommended.
Aggressive prophylaxis and treatment of postoperative nausea and vomiting are required. Minimal analgesia is necessary.
V Tonsillectomy and adenoidectomy
Tonsillectomy and adenoidectomy are among the most common surgical procedures performed in the United States, especially for children. Such surgical procedures are indicated for the treatment of hypertrophic tonsils and adenoids and for recurrent or chronic upper respiratory tract and ear infection and OSA.
The lateral tonsils, tonsillar tissue at the base of the tongue, and adenoids form a tonsillar “ring” around the oropharynx that can lead to significant airway challenges after surgical intervention. An adenotonsillectomy, although often considered a simple procedure, requires a great degree of finesse by the anesthesia provider.
a) Considerations of airway obstruction, shared airway, mechanical suspension of the airway, management of intubation and extubation, pain management, and the desire for a rapid awakening are all subtleties of anesthesia that challenge the anesthesia provider.
b) In adult patients, a tonsillectomy may also accompany a uvulopalatopharyngoplasty (UPPP) for Pickwickian syndrome or OSA. OSA is typically seen with obesity and redundant pharyngeal tissue. Patients with OSA can also present with a history of right heart failure, cor pulmonale, and congestive heart failure, which is not uncommon.
c) The patient undergoing a tonsillectomy or adenoidectomy will probably have a higher incidence of airway obstruction because of the hypertrophied tissues. Chronic obstruction and infections of the tonsils can lead to potential systemic involvement, producing additional cardiac and respiratory anomalies.
d) In the case of suspected airway obstruction, the clinician must choose wisely among routine IV induction, inhalation induction, awake intubation, or fiberoptic-assisted intubation before induction. Adult patients with severe OSA may require a tracheostomy under local anesthesia in advance to secure the airway before the induction of general anesthesia. Such determination is based on the degree of obstruction, physical examination of the airway, and clinical judgment of the anesthesia provider. Regardless of the induction technique chosen, the use of an antisialagogue is strongly encouraged to reduce oral secretion to improve visualization during intubation and surgery.
e) In children, anesthesia is usually induced with an inhalation agent, oxygen, with or without N2O by mask. Some institutions allow parental presence in the operating room during induction to prevent separation anxiety in the child. Tracheal intubation in children is best accomplished under deep inhalation anesthesia or aided by a short-acting nondepolarizing muscle relaxant. The airway generally is secured with an oral RAE or reinforced tube. A cuffed tube is recommended in patients older than 8 to 10 years of age, with continued attention to inflation pressures of the cuff. A properly sized pediatric ETT should allow a leak at 20 cm H2O airway pressure, which reduces the likelihood of postoperative croup and tracheal edema. The tube must be secured midline. A simple yet effective method of securing the oral RAE tube is to apply a strip of tape directly to the chin, incorporating the ETT and another strip of tape over the tube. The first strip provides a secure base for the second strip, which actually holds the tube.
f) After the airway is secured, the mouth gag is inserted by the surgeon. An adequate depth of anesthesia is needed to facilitate gag insertion. The gag, designed to maintain an open mouth and tongue retraction, is equipped with a groove for the ETT to rest in. The airway should be reevaluated at the time the gag is placed to ensure that the tube has not been moved from its original position and that occlusion of the ETT has not occurred as a result of compression from the gag. The table is frequently turned 45 to 90 degrees away from the anesthesia provider just before incision.
g) The choice of techniques varies for the maintenance of anesthesia. There are four major goals to consider when choosing an anesthetic: (1) provide a depth of anesthesia adequate to blunt strong reflex activity elicited by the procedure, (2) a rapid and smooth emergence to facilitate the return of protective reflexes, (3) good postoperative analgesia, and (4) reduced postoperative bleeding.
h) The use of intermediate-acting muscle relaxants is acceptable, but their action must be completely reversed at the end of the case. Judicious narcotic supplementation will reduce the total amount of inhalation agent required and provide analgesia with minimal postoperative respiratory depression. Although postoperative bleeding has been a concern in the past regarding the use of ketorolac, it has been successfully used as an alternative to opioids, has not been found to increase bleeding, and has lead to shortened hospital stays after tonsillectomy.
i) Blood loss during tonsillectomy is difficult to assess but has been estimated to average 4 mL/kg or 5% of blood volume. Average blood loss during UPPP is slightly higher because the procedure frequently is performed in conjunction with adenotonsillectomy. Replacement for blood loss of less than 10% of the calculated volume may be accomplished with the administration of 3 mL of crystalloid per milliliter of blood loss. Although younger, healthier patients can tolerate greater volumes of blood loss, transfusion should be considered if blood loss exceeds 10% of calculated preoperative blood volume.
j) At the end of the surgical procedure, the surgeon may release tension on the mouth gag to ensure that all bleeding has been controlled. The insertion of an orogastric tube and some irrigation may be used to remove blood and secretions from the stomach and oropharynx. This is thought to reduce the incidence of postoperative nausea and vomiting. Suctioning of the oropharynx and nares should be done very gently and briefly by avoiding the surgical beds and to prevent disruption of and prevent mucosal bleeding. Vigorous suctioning may also induce laryngospasm and bronchospasm.
k) During emergence from anesthesia after tonsillectomy or UPPP, the anesthesia provider should ensure that all protective reflexes have returned, the airway is free of blood and debris, and an adequate breathing pattern is present before the removal of the ETT. A topical spray of 2% lidocaine (maximum, 3 mg/kg) on the glottic and supraglottic areas before intubation prevents postextubation stridor and laryngospasm after adenotonsillectomy. This approach has proved as effective as administering lidocaine, 1 mg/kg IV before extubation, but without higher sedation scores.
a) The postoperative tonsillectomy patient should be transported to the recovery room in the “tonsil position” (i.e., on one side with the head slightly down). This allows blood or secretions to drain out of the mouth rather than flow back onto the vocal cords.
b) Adults frequently prefer a middle or high Fowler position after UPPP. This position aids in ventilation and feeling of asphyxiation in the immediate postoperative period. The anesthesia provider must ensure that the patient is awake enough to manage his or her own airway.
c) One hundred percent oxygen with a high-humidity mist is given by face mask or face tent to hydrate the airway. The pharynx should be rechecked directly for bleeding and edema before discharge from the recovery room.
Bleeding tonsil
The incidence of posttonsillectomy bleeding that requires surgery is 0.3% to 0.6%. Approximately 75% of the postoperative tonsillar hemorrhages that occur are within 6 hours of the surgical procedure. The remaining 25% of the postoperative bleeds occur within the first 24 hours of surgery, although bleeding may be noted up until the sixth postoperative day. Because the cautery is used for control of bleeding instead of ligatures, a slow oozing of the tonsillar bed is far more common than profuse bleeding.
One concern is that these patients may swallow large volumes of blood before bleeding is actually discovered. The patient may present with signs of hypovolemia, which are evidenced by tachycardia, hypotension, and agitation. If the blood is swallowed, the patient may have nausea and vomiting. Appropriate laboratory tests (e.g., hemoglobin and hematocrit) should be performed to determine replacement. If reoperation is deemed necessary, restoration of intravascular volume or blood (or both) based on the volume lost should precede induction. It is important to evaluate the adequacy of IV access before induction (two IV lines may be appropriate), assess the coagulation variables, and be prepared to transfuse blood. All such patients should be assumed to have a significant amount of blood in the stomach, and an awake intubation of the trachea should be an initial consideration to maintain reflexes.
At induction of anesthesia, an additional person should be available to provide suctioning of blood from the oropharynx. If an awake technique is not practical, a rapid-sequence induction with cricoid pressure should be implemented. The patient should be placed in a slight head-down position to protect the trachea and glottis from aspiration of blood. A nasogastric tube may be placed to remove stomach contents before induction and then removed after induction. The induction agent selected is based on the hemodynamics and condition of the patient.
W Tracheotomy
Tracheotomy is an incision into the trachea to form a temporary or permanent opening, the latter of which is called a tracheostomy. The incision is made through the second, third, or fourth tracheal ring, and a tube is inserted through the opening to allow passage of air and the removal of tracheobronchial secretions. Except in cases of head, neck, and face trauma, tracheotomy is rarely performed as an emergency procedure.
a) Indications for tracheostomy
(1) To relieve upper airway obstruction
(c) Acute infection: acute epiglottitis, diphtheria
(1) Patient positioned supine with sandbag between scapulae
(2) Transverse cervical skin incision 1 cm above the sternal notch
(3) Incision extending to the sternocleidomastoid muscles
(4) Dissection through fascial planes and retraction of anterior jugular veins
(5) Retraction of the strap muscles
(6) Division of the thyroid isthmus and oversewing to prevent bleeding
(7) Placement of a cricoid hook on the second tracheal ring
(8) Stoma fashioned between the third and fourth tracheal rings
(9) Removal of the anterior portion of the tracheal ring
(10) No advantage in creating a tracheal flap
(11) ETT withdrawn to the subglottis
(12) Tracheostomy tube inserted using an obturator
2. Preoperative assessment and patient preparation
a) History and physical examination: These patients may or may not be already intubated. If the patient is not intubated, his or her airway should be carefully assessed. Information regarding any abnormal pathologic features that may make intubation difficult should be sought from the surgeon or reports from specific tests such as triple endoscopy. If intubated, the patient’s respiratory status and the following should be assessed: vent settings, peak airway pressures, respiratory rate, amount and color of tracheal secretions, need for and frequency of suctioning, lung sounds, arterial blood gases, chest radiography, and the presence of pulmonary infections.
(1) Monitoring is routine, with a CVP or pulmonary arterial catheter, as well as an arterial line as indicated by the patient’s history.
(2) If peak airway pressures are greater than 60 mmHg, the patient may need a ventilator from the intensive care unit.
(3) A sterile 6-inch connector is used to attach the ETT to the vent or sterile circuit.
(4) Consider a bronchial adapter. Patients frequently have a bronchoscopy after tracheotomy placement.
4. Anesthetic technique and perioperative management
Use general anesthesia and skeletal muscle paralysis or local anesthesia.
a) Induction: If a difficult airway is anticipated, awake fiberoptic intubation should be performed. The surgeon should be on standby for an emergency tracheotomy in the event that intubation attempts are unsuccessful. If the patient is already intubated, titrate anesthetic agents to the patient’s need or convert sedation to general anesthesia.
(1) Adjust the oxygen and air mixture to maintain saturation at greater than 95%.
(2) If the patient is stable, an inhalation agent, and a narcotic may be introduced.
(3) Attempt to maintain the oxygen concentration at 30% to decrease the chance of airway fires.
(a) Pour saline into the pharynx to absorb the heat.
(b) Temporarily discontinue the oxygen source.
(c) Extubate and reintubate with a new ETT.
(d) Follow up with chest radiography, bronchoscopy, steroids, and blood gas measurements.
(5) Maintain constant communication with the surgeon. Use a team approach. Use hand ventilation with 100% oxygen during insertion of the tracheotomy tube. The surgeon will ask the anesthesia provider to gently pull back the oral ETT before insertion of the tracheostomy tube.
(1) The patient may be transferred to the intensive care unit after the procedure. The nondepolarizing muscle relaxant may not have to be reversed if prolonged ventilation is planned.
(2) The patient has 100% oxygen through an Ambu bag with monitoring devices functioning and is returned to the unit.
X Uvulopalatopharyngoplasty
Uvulopalatopharyngoplasty is performed primarily for the treatment of OSA. Tonsillectomy is often performed concurrently. Nasopharyngeal airway obstruction is relieved by removing redundant and obstructing tissues of the posterior pharynx.
Inspiratory muscle tone is lost during rapid eye movement sleep, resulting in relaxation of the pharyngeal muscles and thus creating airway obstruction. Adults with OSA are often obese.
a) History and physical examination
(1) Cardiac: Hypoxia and hypercapnia may lead to pulmonary hypertension, right ventricular hypertrophy, cor pulmonale, cardiac arrhythmias, and failure of the right side of the heart.
(2) Respiratory: Frequent nocturnal arousals (up to 50 times per hour) are common. Periods of apnea may last up to 2 to 3 minutes. These patients often have a long history of snoring.
(3) Neurologic: Loss of rapid eye movement sleep results in excess daytime somnolence, fatigue, and impaired judgment.
(4) Gastrointestinal: These patients may have increased incidence of gastroesophageal reflux disease and hiatal hernia and should be considered to have full stomachs.
b) Patient preparation: Medical management includes weight reduction in obese patients, decreasing alcohol consumption, and nasal continuous positive airway pressure.
(1) Laboratory tests: As indicated by the history and physical examination. These patients often develop polycythemia from chronic hypoxemia.
(2) Diagnostic tests: As indicated by the history and physical examination
(3) Medications: Use minimal preoperative narcotics or sedatives because these patients have heightened sensitivity to them. Anticholinergics are helpful to decrease secretions.
a) Monitoring equipment: Standard
b) Additional equipment: Airway adjuncts, difficult airway cart
c) Operating room table: Ensure an appropriate weight limit.
4. Perioperative management and anesthetic technique
(1) Awake fiberoptic laryngoscopy and intubation may be indicated.
(2) Inhalation agents are used with maintenance of spontaneous respiration and succinylcholine only after visualization of the larynx.
(3) IV rapid-sequence induction is performed after 3 to 4 minutes of preoxygenation, cricoid pressure, and elevation of the head of the bed.
(1) Inhalation agent: Isoflurane or desflurane
(2) 50% oxygen (may require high fractional inspired oxygen)
(1) Lidocaine, 1 to 1.5 mg/kg before extubation
(2) As with tonsillectomy, the surgeon may release the mouth gag to see whether there is any uncontrolled bleeding. At this time, the patient should have an orogastric tube placed, and the stomach should be suctioned. The nasal cavity and oropharynx should also be gently suctioned and care taken not to dislodge any clots that may precipitate bleeding and cause laryngospasm.
c) Hemoglobin and hematocrit if blood loss was excessive
d) Careful titration of narcotics
e) Postoperative complications: Airway obstruction resulting from swelling is the most common postoperative complication of uvulopalatopharyngoplasty. Typically, the patient will receive a dose of steroids intraoperatively to aid in reducing this swelling. Patients who undergo this procedure are usually admitted to the hospital, where their respiratory and airway status may be monitored carefully. If the tonsils have been removed, the possibility of recurrent bleeding must also be considered.