Hematometra and Hematocolpos
Synonyms/Description
Etiology
Hematometra/Hydrometra
Hematocolpos/Hydrocolpos
Ultrasound Findings
Differential Diagnosis
Clinical Aspects and Recommendations
Figures

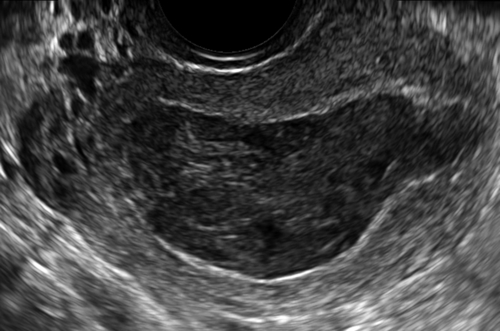
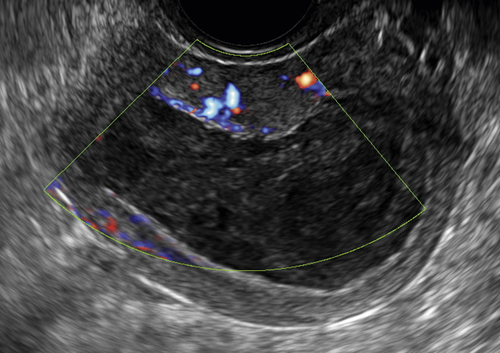
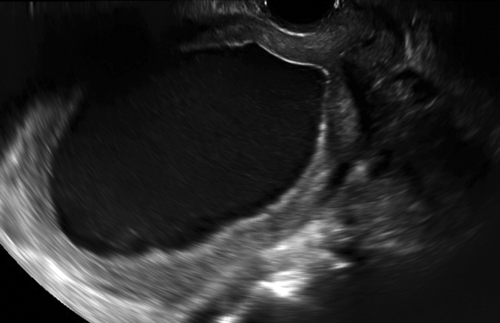
Figure H1-1 A and B, Longitudinal and transverse views of the uterus with fluid present in the cavity, including the cervix. Note that the fluid has low-level echoes, which is characteristic of unclotted blood. This was the result of an obstruction at the level of the external os. C, Blood flow in the myometrium but no flow within the uterine cavity.
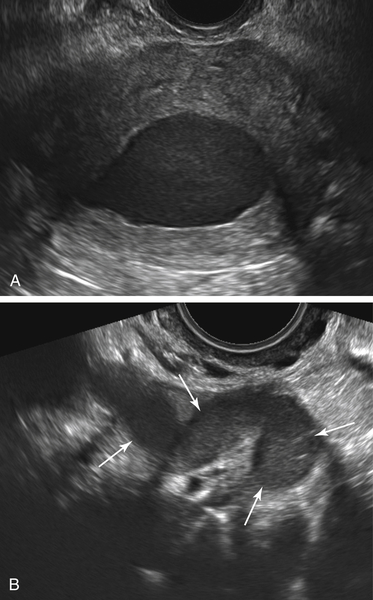
Figure H1-4 This is a patient post-endometrial ablation with pelvic pain. A, A transverse view through the uterine fundus showing a hematometra (centrally). B, A dilated fallopian tube full of fluid (arrows) with debris consistent with a hematosalpinx. The contralateral tube had the same appearance, suggesting that there is residual cycling endometrium at the uterine fundus, above the level of the ablation.
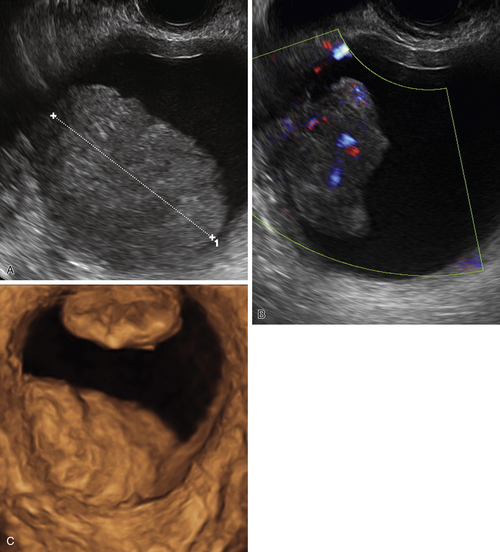
Figure H1-5 Postmenopausal patient with endometrial cancer and a 5-week history of postmenopausal bleeding. A and B, An endometrial mass (calipers) with abundant vascularity, located in the uterus and outlined by intracavitary fluid. C, A 3-D rendered image of the uterine cavity distended with fluid, showing two separate irregular masses in the endometrium and protruding into the cavity.
Suggested Reading
Goldstein S.R. Postmenopausal endometrial fluid collections revisited: look at the doughnut rather than the hole. Obstet Gynecol. 1994;83:738–740.
Drakonaki E.E., Tritou I., Pitsoulis G., Psaras K., Sfakianaki E. Hematocolpometra due to an imperforate hymen presenting with back pain: sonographic diagnosis. J Ultrasound Med. 2010;29:321–322.
Shaked O., Tepper R., Klein Z., Beyth Y. Hydrometrocolpos—diagnostic and therapeutic dilemmas. J Pediatr Adolesc Gynecol. 2008;21:317–321.
Verma S.K., Baltarowich O.H., Lev-Toaff A.S., Mitchell D.G., Verma M., Batzer F. Hematocolpos secondary to acquired vaginal scarring after radiation therapy for colorectal carcinoma. J Ultrasound Med. 2009;28:949–953.