Anatomy of the Vagina
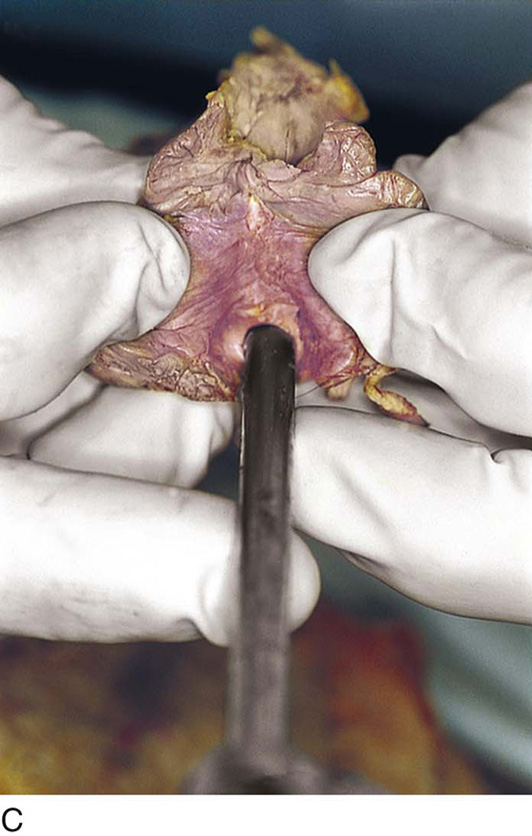
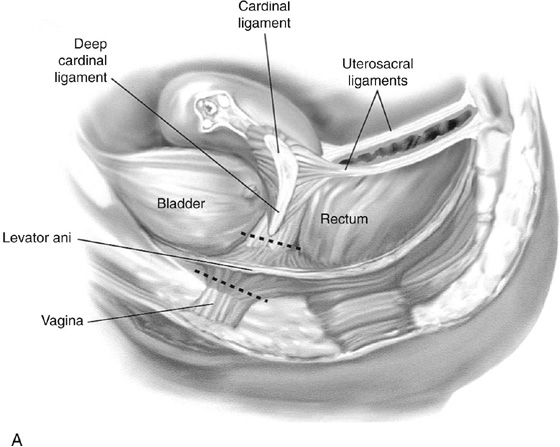
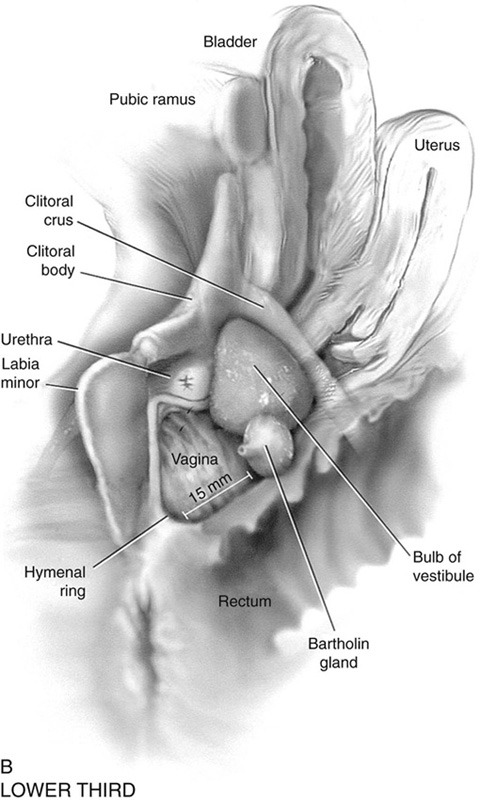
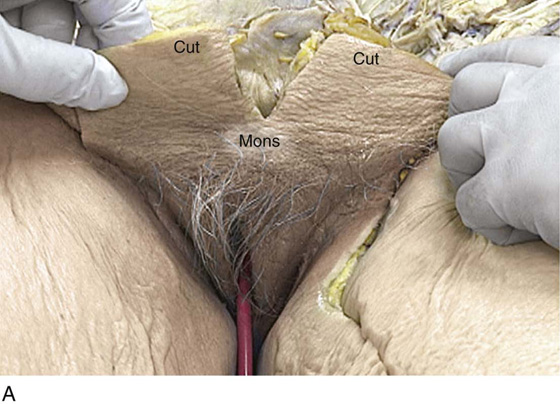
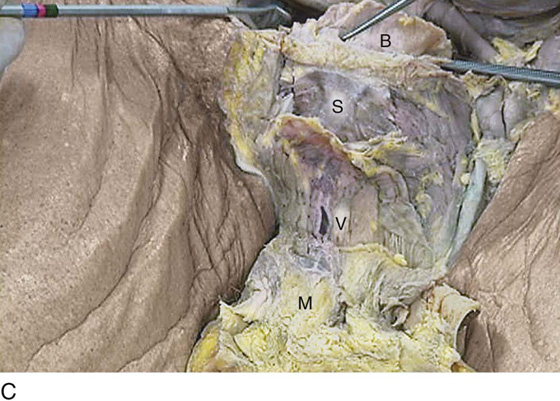
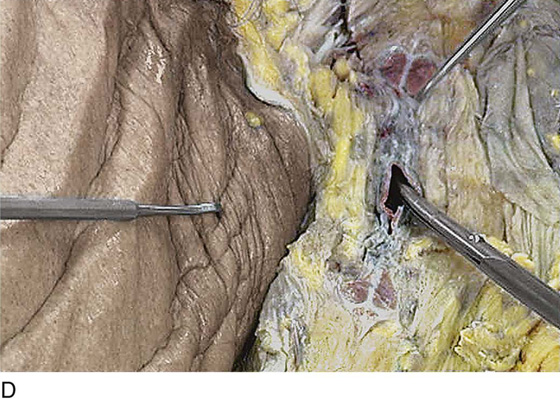
The vagina is a potential space that connects the lower portion of the uterus (cervix) to the outside environment. The vagina measures 8 to 8.5 cm from the hymenal ring to the top of the anterior fornix; 7 to 7.5 cm to the top of the lateral fornix; and 9 to 9.5 cm to the top of the posterior fornix. For the sake of organization, the vagina may be divided into thirds: upper, middle, and lower. The upper third of the vagina is closely related to the cervix uteri, to which it is attached (Fig. 51–1). Throughout its length, the vagina is intimately applied to the bladder and urethra anteriorly and is similarly applied to the rectum posteriorly. In its lower third, the vagina, rectum, and urethra share common walls. The lower third of the vagina also is closely related to the vulva, to which it is attached at the level of the vulvar vestibule (Fig. 51–2A). This particular transitional area can be considered the entry portal to or the exit portal from the vagina. In fact, in the lower third, one might consider the urethra, vagina, and anus–rectum as a single interdependent and interrelated structure rather than as independently functioning anatomic units (Fig. 51–2B, C). By sawing away the symphysis pubis and dissecting the bladder and urethra from the anterior vagina, important relationships can be seen and better understood (Fig. 51–2D through F).
The microscopic vagina consists of a mucosa that is made up of multilayered noncornified squamous epithelium. The underlying stroma consists of collagen admixed with elastic tissue. Beneath the stroma is smooth muscle interspersed with collagen. The epithelium measures 0.15 to 0.30 mm from top to bottom (surface to basement membrane). The entire vaginal wall thickness in a menstruating woman ranges from 2 to 3 mm.
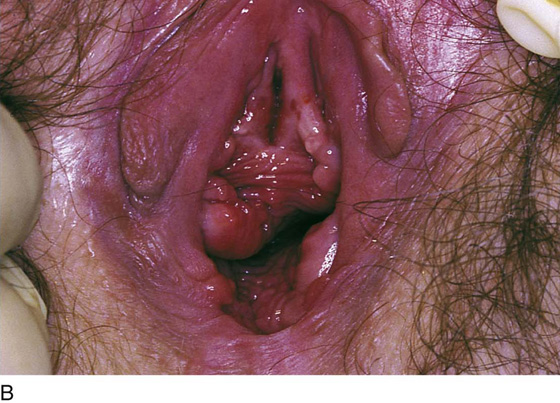
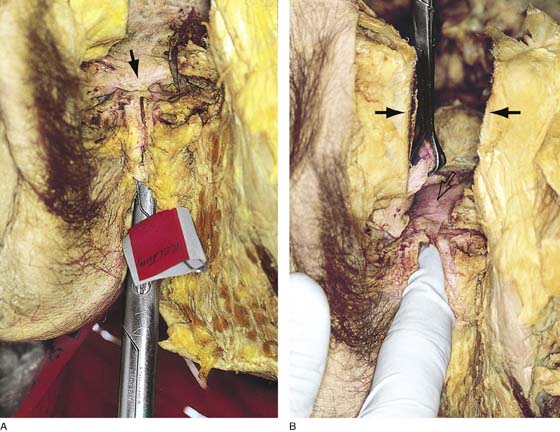
Lower Third
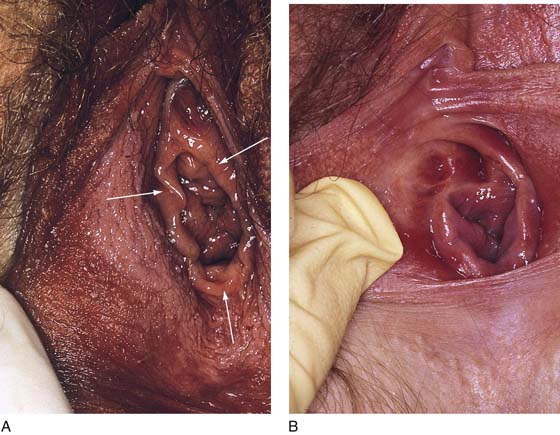
The hymenal ring forms the boundary between vagina and vestibule (Fig. 51–3A, B). Although the vagina contains no glandular elements under normal circumstances, several mucus-secreting structures are in close proximity: the paraurethral and vestibular glands (Fig. 51–4). The Bartholin glands (greater vestibular glands) are closely applied to the posterolateral wall of the vagina at a level 15 mm deep from the surface of the vestibule (Fig. 51–5A, B). At the 6-o’clock position, the rectum is 3 to 4 mm beneath the vagina, and at 12 o’clock, the urethra is 2 to 3 mm anterior to the vagina (Figs. 51–6A, B and 51–7A).
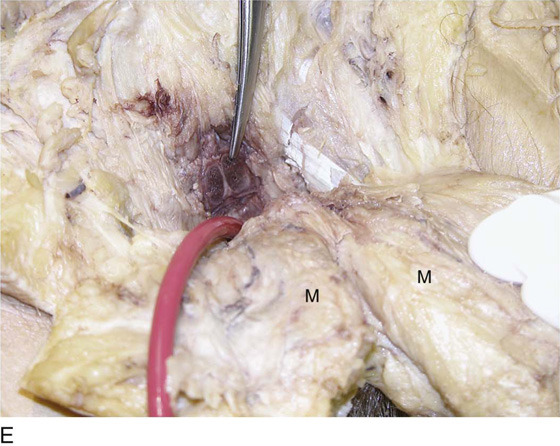
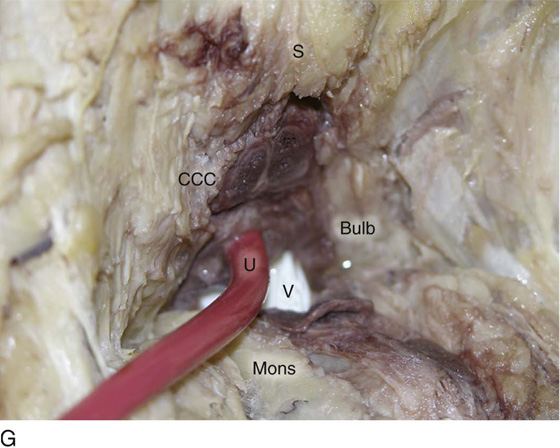
The vagina is highly vascularized, particularly on the anterolateral and lateral walls, from the level of the hymenal ring to the urethrovesical junction (Fig. 51–7B). Large venous sinuses and cavernous sinuses account for this vascularity, which is most plentiful at the level of the bulb of the vestibule. The bulb is encountered at a depth of 1.5 cm from the surface of the vestibule and lies in close proximity to the urethra and the anterolateral wall of the vagina. The urethra is covered on its anterior and lateral aspects with cavernous tissue emanating from the clitoris and the bulb (Fig. 51–8A through G). When one is dissecting in this area, consideration should be given to the pronounced vascularity along the lateral and anterolateral walls and the need for vasoconstrictive agents.
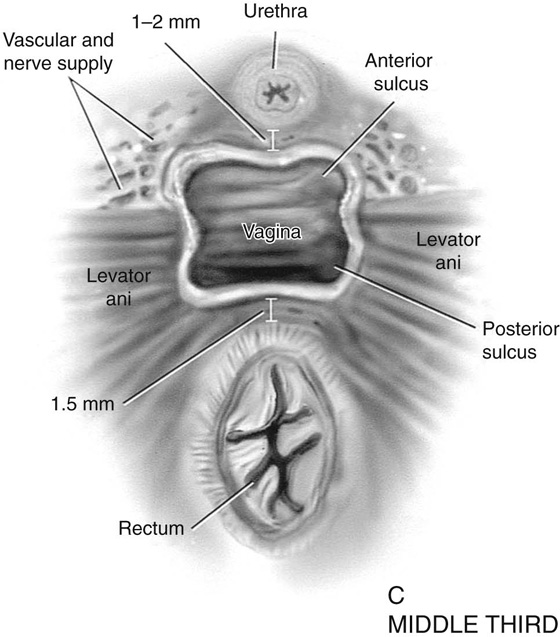
Middle Third
The middle third begins just below the urethrovesical junction and crosses beneath the lower margin of the symphysis pubis (posterior-inferior margin) (2.5 to 3.5 cm from the hymenal ring). The levator ani muscle is applied to the lateral and posterior vaginal walls most prominently at the junction of the middle and lower thirds (see Fig. 51–7C). This portion, together with the cranial portion of the lower third, has the greatest degree of mobility compared with the rest of the vagina.
Upper Third
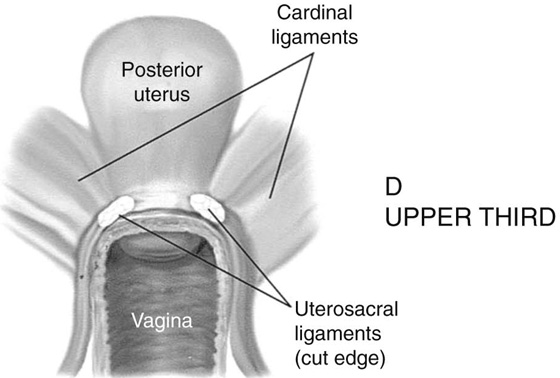
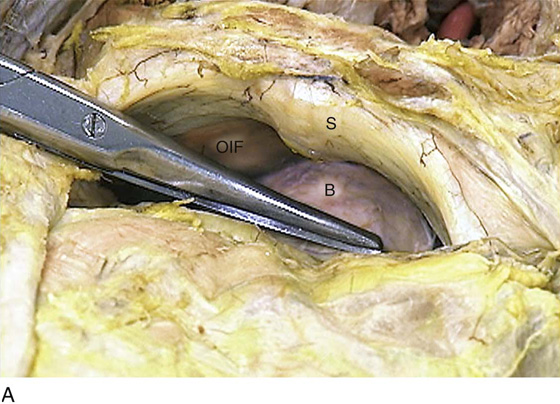
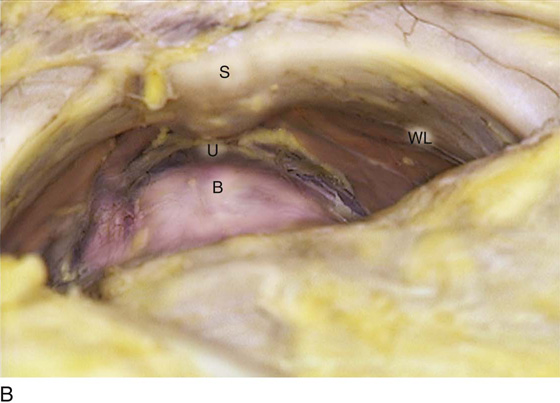
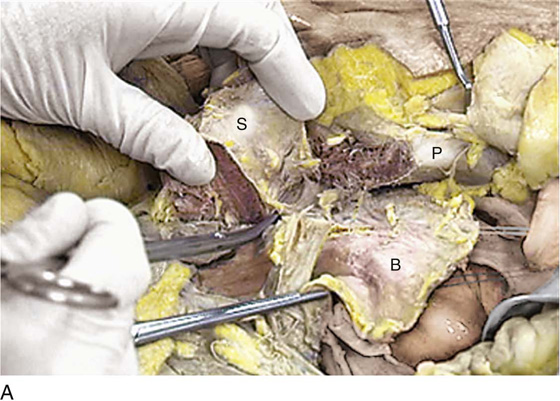
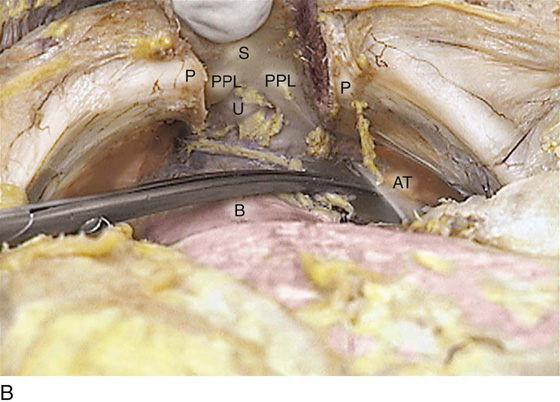
The upper vagina is closely applied to the bladder but does not share the common wall encountered at the level of the urethra. A layer of loose areolar tissue permits the bladder to be easily dissected from the upper vagina (see Figs. 51–2D through F). Similarly, the rectum can be easily dissected from the upper vagina. However, as one dissects caudally, the wall shared among bladder, urethra, and vagina allows no easy plane of separation. The vagina terminates around the cervix, and the vaginal vault is divided into fornices by the protruding portio vaginalis of the cervix. The stroma of the vagina is actually inseparable from the cardinal and uterosacral ligaments (see Fig. 51–7D). Between the latter is a bloodless entry point between the posterior fornix of the vagina and the cul-de-sac (i.e., the entry into the peritoneal cavity). The relationships of the upper vagina to the bladder, urethra, and cervix require precise anatomic knowledge of the retroischial and retropubic (extraperitoneal) spaces. Many gynecologists refer to the lateral areas as paravaginal, but in reality these areas constitute the perivesical spaces in their entirety. The anterior boundary of the retropubic space is the symphysis pubis and the pubic bone. The posterior boundary is the main body of the urinary bladder. The perivesical spaces extend on either side of the bladder and end above at the pubic bone and the obturator internus muscle, and below at the obturator internus muscle and the ischial bone. The levator ani muscle originates from the lower margin of the inferior pubic ramus and the fascia of the obturator internus and funnels downward to the junction of the middle one third and the lower one third of the vagina and into the perineal and perianal areas. The anatomy can be demonstrated only by sawing away a portion of the pubic bone (Fig. 51–9A through D).
FIGURE 51–1 The upper third of the vagina is closely related to the uterus, particularly the cervix uteri. The rugous vaginal mucosa can be seen to merge with the smooth cervical mucosa on the far periphery of the portio vaginalis of the cervix. The central cervix creates the vaginal fornices at the vault.
FIGURE 51–2 A. The lower third of the vagina forms a unit with the labia minora, vestibule, urethra, and rectum. The urethra is incorporated into the anterior vaginal wall. The anterior and posterior walls are in apposition. B. Compared with the lower vagina, seen in Figure 51–2A, this woman’s vagina is agape with a definite space visible between the anterior and posterior walls. Note the size and shape of the enlarged external urethral meatus. C. The bladder, the urethra, and a portion of the vestibule have been dissected free of the anterior wall of the vagina and have been removed. A metal cannula traverses the urethra into the bladder. D. The pubic bone has been cut away with a saw (large arrow). The previously excised bladder (B) and urethra (U) (see Fig. 51–2C) have been replaced in the pelvis. The bladder covers the retroverted uterus, and the sigmoid colon (C) covers the uterus, which lies in the cul-de-sac. The small arrow points to the right ureter. E. The bladder-urethra complex has been removed, exposing the anterior (outside) wall of the vagina (V). The surgeon’s finger is in the partially incised vagina and is located in the right lateral fornix (arrow). The scissors are directly lateral to the ureter. F. Detail of Figure 51–2E. The tip of the scissors is pointing to the pubocervical fascia of the vaginal wall. The blades of the scissors lie on that fascia and over the anterior vaginal fornix (F). Note the two sawed edges of the pubic bone overlying the surgeon’s gloved hand.
FIGURE 51–3 A. The hymenal ring (arrows) separates the vagina from the vestibule. B. In this case of vestibulitis, the boundary between the vagina and the vestibule is even more apparent.
FIGURE 51–4 The proximity of several mucous glands to the vagina is apparent. The Skene ducts (small arrow), paraurethral ducts (large arrow), and Bartholin ducts (white arrow) all are intimate with the outer wall of the vagina.
FIGURE 51–5 A. The relationship of the Bartholin gland to the posterolateral wall of the vagina (V) is shown here. The V overlies the bloody postvaginal mucosa. Clamps are placed across the upper and lower margins of the Bartholin gland (arrow points to the gland). The Allis clamp is attached to the lower vaginal lateral wall (introitus). B. The arrow points to the vagina. Allis clamps stretch the lateral wall of the vagina over the site where the Bartholin gland previously was located. A proctoscopic swab has been placed in the defect created by extirpation of the gland. The gland occupied a location 15 mm deep as measured from the outer edge of the introitus.
FIGURE 51–6 A. Scissors have been placed into the anus. Note the direction that the anus (scissors) takes to reach the posterior wall of the vagina. The bulge in the vagina is highlighted by the arrow. B. The anal sphincter and the perineal body have been cut, permitting a view of the direction of a finger placed in the anus relative to the posterior vagina. The Babcock clamp is attached to the incised anterior vaginal wall. The open arrow points to the posterior vaginal wall. The cut margins of the pubic bone are noted by arrows.
FIGURE 51–7 A. The vagina is divided into thirds of roughly equal length. The lower third is attached to the vestibule at the hymenal ring and is closely associated with vulvar vestibular structures. The middle third and upper lower third lateral walls are applied to the levator ani muscles. The upper third of the vagina is attached to the cervix. The cardinal and uterosacral ligaments likewise support the upper vagina as well as the uterus. Throughout its course, the vagina is intimately connected anteriorly to the bladder-urethra and posteriorly to the rectum. B. The lower portion of the left wall of the vagina has been removed. The lower right interior lateral wall of the vagina is seen. Approximately 15 mm deep from the surface of the vestibule is the left Bartholin gland and the left vestibular bulb. These are located at the lateral and posterolateral outer aspects of the left vaginal wall. Crossing above the vagina and urethra from the pubic ramus is the left clitoral crus (corpora cavernosum clitoris). C. A cross-section through the middle third of the vagina. Note the proximity of the rectum and the urethra. The levator ani inserts into the lateral vaginal walls. The anterior and lateral sulci are formed by the anterior and posterior walls, which are relatively relaxed compared with the fixed lateral walls. D. The posterior vaginal wall has been cut away at the level of the upper third of the vagina. Note the relationship of the uterosacral and lower cardinal ligaments to the vaginal vault.
FIGURE 51–8 A. The incision line cut into the mons is shown. A catheter has been placed into the cadaver’s urethra. B. The mons (M) has been cut and turned down. The distal portion of the corpora cavernosa clitoris (CCC) is seen in this view. The retropubic space has been opened and the relative positions of the pubic bone and symphysis (P) and the bladder (B) to the midvagina can be appreciated. C. This view is taken from the foot. The mons (M) is turned down. The midvagina (V) is seen as it passes beneath the symphysis (S) pubis. The bladder (B) is seen behind the pubic bone. D. Close-up of Figure 51–8C with the dissecting scissors placed into the midvagina. The upper hook marks the location of the corpora cavernosa clitoris. E. The catheter is in the urethra. The scissors point to the corpora of the clitoris located just above the midurethra. The mons (M) has been cut and reflected caudad. F. Close-up view showing the spongelike consistency of the cavernous tissue. G. The operator’s gloved finger is in the vagina (V). The bulb of the vestibule surrounds the urethra (U) on three sides. The corpora cavernosa clitoris (CCC) lies immediately anterior to the urethra with bulb tissue interposed between the two structures.
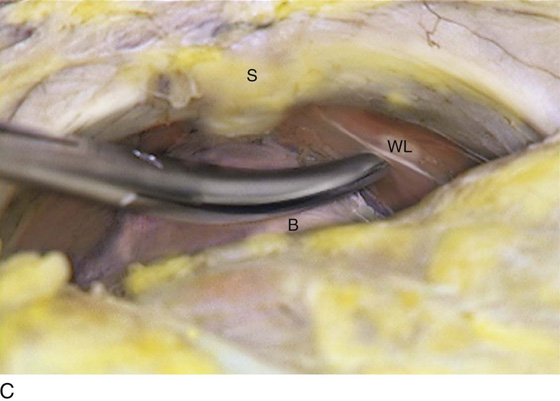
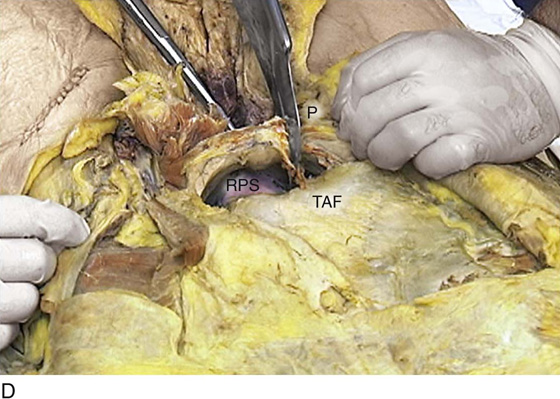
FIGURE 51–9 A. The relationships of the urethra, vagina, and bladder can be best understood by widely exposing the retropubic space. Important reference points include the symphysis pubis (S), the obturator internus muscle and its covering fascia (OIF), and the urinary bladder (B). B. This view of the retropubic space details the urethrovesical junction (U and B) at the lower margin of the caudal sloping symphysis pubis (S). A thickening in the obturator internus fascia creates a whitish appearance, i.e., a white line (WL). C. The scissors tip rests on the obturator internus fascia at the white line. D. The dissection into the retropubic space (RPS) is entirely extraperitoneal. Abdominal contents are contained under the transversus abdominis fascia (TAF), which is bound to the parietal peritoneum of the anterior abdominal wall. The relationships between the middle and upper vagina and the urethra and bladder base cannot be appreciated without removing a portion of the pubic bone (P) with a saw.
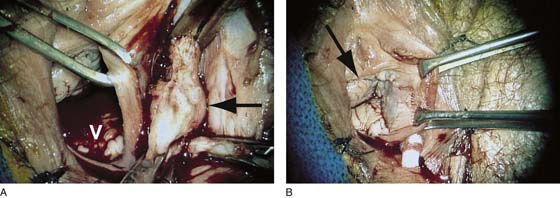
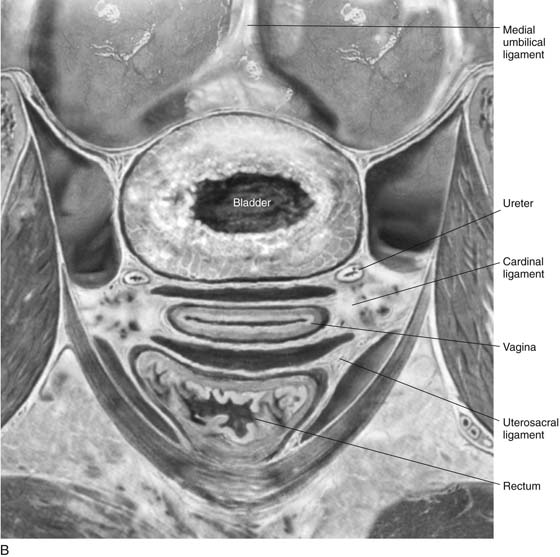
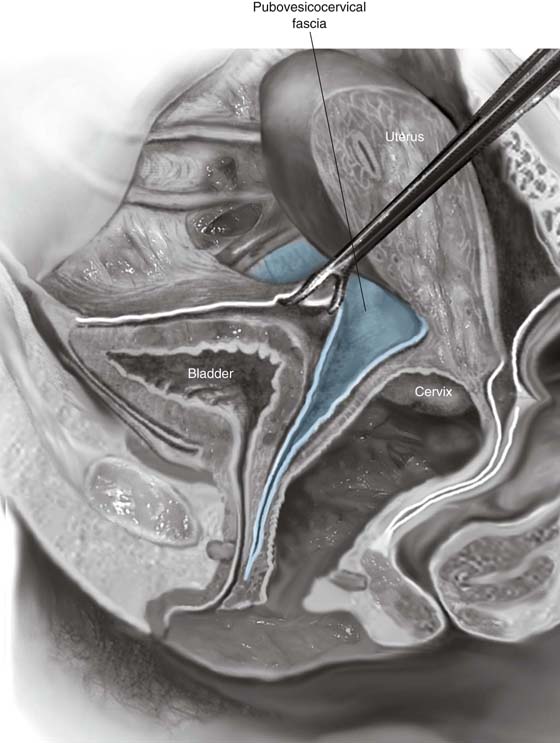
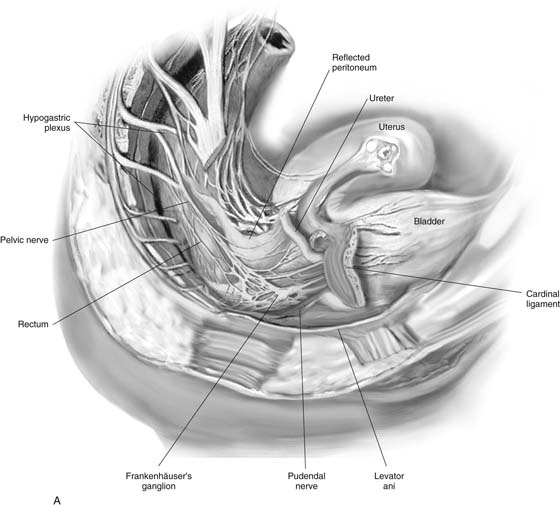
Much controversy has existed as to which structures support and maintain the position and integrity of not only the vagina but also its immediate neighbors: the bladder, the urethra, and the rectum. Specific anatomic sites of support to individual as well as paired structures can be identified (Fig. 51–10A through C). The ureters and the bladder base are closely related and applied to the area of the anterior upper vagina and the anterolateral fornices (Fig. 51–11A, B). Common walls are shared by the urethra, bladder, and vagina anteriorly and with the rectum and vagina posteriorly. Figure 51–11C shows an overview of the urethra (urethrovaginal complex) and the bladder after the pubic bone was removed (Figs. 51–11C through G). The major support to the upper vagina consists of the cardinal ligaments as well as shared walls between bladder, rectum, and, to a lesser extent, uterosacral ligaments. The vaginal vault therefore is mainly supported (as is the cervix and bladder base) by the deep cardinal ligaments (Fig. 51–12A through C). Also, between the cervix, upper vagina, and bladder exists a well-defined fascial layer, silvery white in color. This layer is the pubovesicocervical fascia and could likewise be considered part of the paravaginal fascia (Fig. 51–13). The deep cardinal ligaments extend into the perivesical spaces to the pelvic side wall, that is, the obturator internus muscle, arcing posteriorly toward the ischial spine along the retroischial space (Figs. 51–14A through G, 51–15A through C).
The upper vagina is supplied via the pelvic plexus with input from the hypogastric plexus, prevertebral ganglia, and sacral nerves. The lower vagina is supplied by the pudendal nerve. Curiously, the vagina is relatively insensitive to biopsy forceps and to light touch (see Fig. 51–14A).
The blood supply emanates from the descending branch of the uterine artery, the vaginal artery, and the internal pudendal artery.
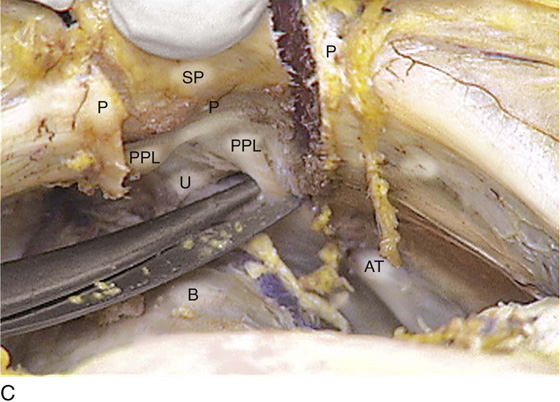
FIGURE 51–10 A. The symphysis pubis (S) has been sawed through. The cut edges of the pubic bone are clearly seen. The most prominent support of the urethra (U) as it passes beneath the symphysis (i.e., at its junction with the bladder [B]) is the posterior puboprostatic ligaments (pubourethral ligaments). The clamp points to the left ligament. B. The cut symphysis pubis (S) is pulled forward, exposing the urethra (U) at its junction with the bladder (B). Note the cut edges of the pubic bone (P). The right and left posterior puboprostatic ligaments (PPLs) are clearly seen at the lower margin of the symphysis. Note that the arcus tendineus (AT) terminates at the puboprostatic ligament on either side. C. The right puboprostatic ligament (PPL) is about to be cut to free the symphysis pubis (SP) from the urethra (U) and bladder (B). P, Cut edges of pubic bone; OIF, obturator internus fascia; AT, arcus tendineus.
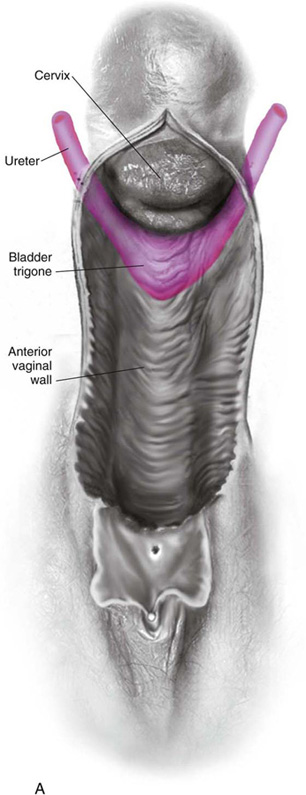
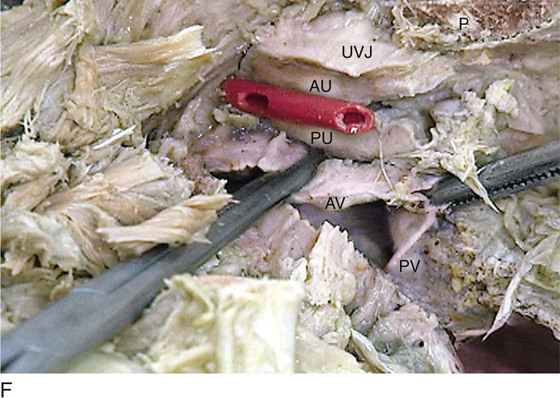
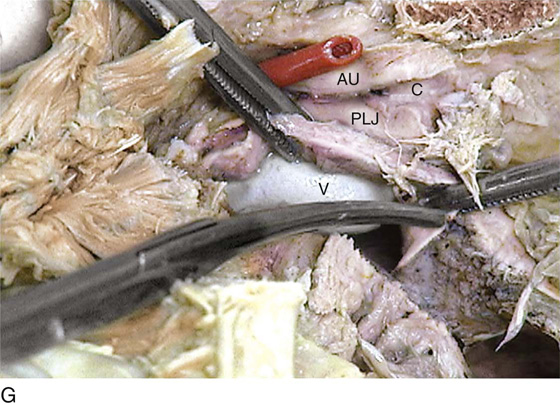
FIGURE 51–11 A. The rectum and the posterior wall of the vagina have been excised. The relationship of the ureters and bladder base to the anterior and anterolateral vagina is illustrated. Urinary tract structures are pink. If the picture is inverted, the relationship of the urethra and the vestibule to the anterior vagina can be better understood. B. Coronal section detailing the relationships of the upper vagina, ureters, cardinal ligaments, and vesicovaginal and rectovaginal spaces. C. This panoramic view of the urethra (U), the bladder (B), and the perivesical space (scissors) can be seen only after the pubic bone is widely sawed away. D. The cut edge of the pubis allows dissection of the ureter beneath the area previously occupied by the symphysis pubis. The anterior wall of the urethra is being cut. E. The anterior wall of the urethra has been filleted open, as has the lower anterior bladder wall. F. The urethra and the vagina share a common wall. The catheter occupied the urethral canal before the urethra was cut open. A sagittal cut has been made through the urethrovesical junction (UVJ). The anterior (AU) and posterior (PU) urethral walls are seen. The scissors point to the common wall shared between the urethra and the vagina, specifically the anterior wall of the vagina (AV). The posterior wall of the vagina (PV) is also exposed. G. The relationship between the urethra (AU and PU) and the mid and upper vagina (V) is demonstrated by the surgeon’s finger placement within the vagina.
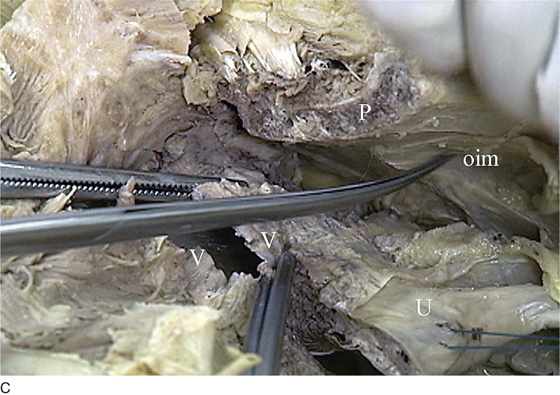
FIGURE 51–12 A. The junction of the upper one third and the middle one third of the vagina (V) beneath the symphysis (sawed away) is nicely demonstrated here. The cut and sloping edge of the pubic bone (P) is seen in the right upper corner. B. The scissors have been pushed through the right upper vaginal wall (V) into the retropubic space located behind (cranial) the cut pubic bone (P). C. The uterus (U) has been hemisected and is seen via sagittal view. The uterus is pulled upward via the blue fundal traction stitch. The Kocher clamp is located at the cervicovaginal junction. The cervix is also sagittally viewed. The vagina has been opened laterally, and the anterior and posterior vaginal (V) walls are in clear view. The scissors point to the obturator internus muscle (oim). P, Cut edge of the pubic bone.
FIGURE 51–13 The distribution of the pubovesicocervical fascia is shown here. The fascial space may be entered at the level of the cervix. As the space is developed, a nice plane of dissection permits identifiable separation of the vagina from the urinary bladder.
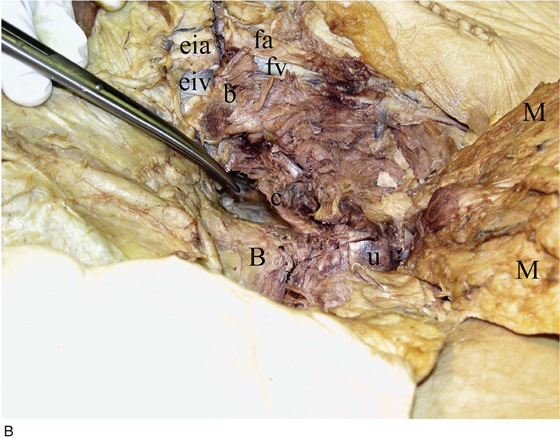
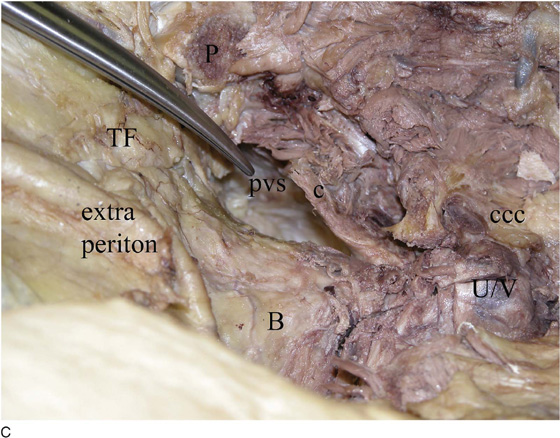
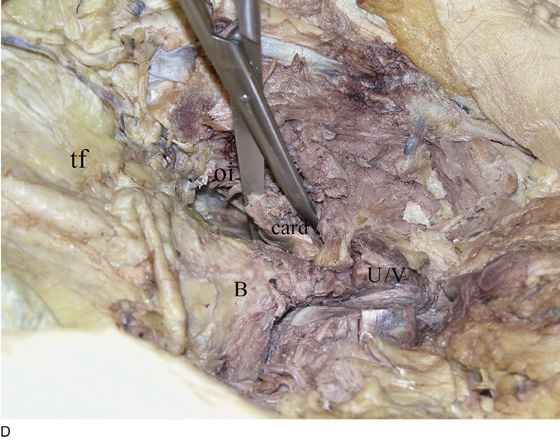
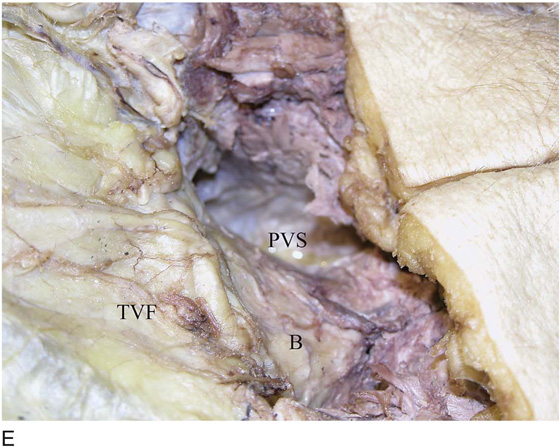
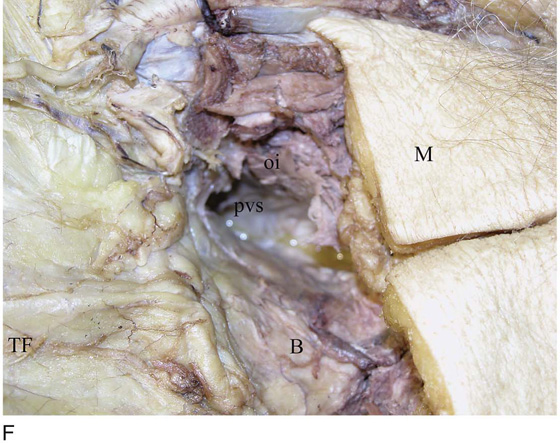
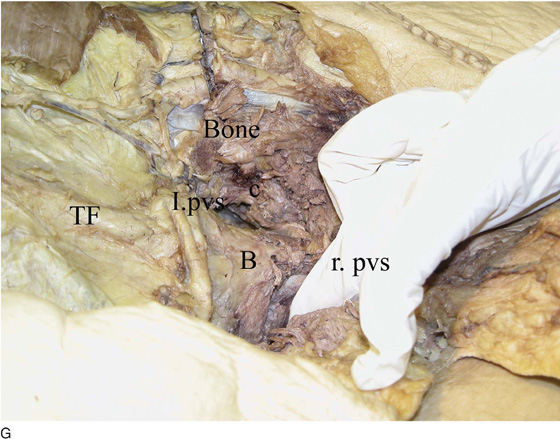
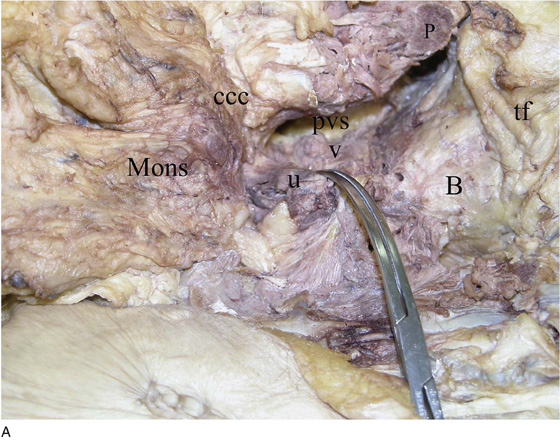
FIGURE 51–14 A. The nerves supplying the cervix and the vagina are shown. The focal points of distribution are the pelvic nerves and the hypogastric plexus. B. The entire retropubic and subpubic areas have been exposed and are viewed from above. The external iliac artery and vein (eia, eiv) and the extension into the thigh as the femoral artery and vein (fa, fv) are seen crossing over the cut edge of the pelvic bone (b). The scissors point into the perivesical space to the left of the bladder (B). The urethra (u) has been cut along the anterior wall through most of its length. The deep cardinal ligament (c) attaches to the bladder base and upper vagina. The mons (M) has been cut and reflected caudally. C. This magnified view of part B shows details of the urethrovaginal complex (U/V), the bladder and the perivesical space (pvs), and the deep cardinal ligament (c). The left clitoral crus (ccc) can be seen to the left of the mid U/V complex. The widely cut edge of the pubic bone (P) is seen in the background. The transversus abdominis fascia (TF) covers the anterior intra-abdominal contents extraperiton, extraperitoneum. D. The scissors are in place to cut the deep cardinal ligament (card). E. The deep cardinal ligament has been severed, creating a large perivesical space (PVS), which extends posteriorly and caudally behind the ischial bone. F. This magnified view with the mons (M) replaced to its normal position shows the relationship of the obturator internus (oi) muscle to the deep perivesical space (pvs) after the cardinal ligament has been cut. G. This view shows the left deep cardinal ligament (c), the left perivesical space (l.pvs), and the bladder (B). The surgeon’s finger has been placed into the right perivesical space (r.pvs).
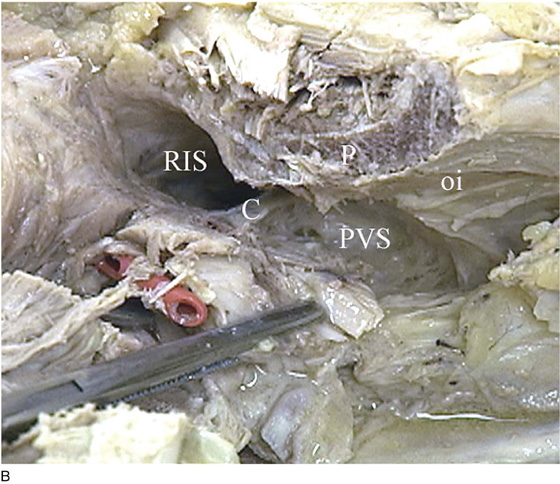
FIGURE 51–15 A. This picture is taken from the left side looking to the right. The mons again has been turned down. The pubic bone (P) has been sawed out. The operator’s finger has been placed into the vagina (v), and the vagina has been pushed to the right of the urethra (u) at the junction of the urethra and the bladder (B). The clamp points to the bulging vagina. The right corpora cavernosa clitoris (ccc) is in front of where the symphysis pubis would have been located. The perivesical space (PVS) is lateral to the vagina. B. Detail of the right perivesical space (PVS) and retroischial space (RIS). Note that the deep cardinal (C) ligament curves and arcs posteriorly along the arcus tendineus and represents a much more substantive structure than the arcus formed by the obturator internus (oi) fascia. C. The scissors are poised to cut the right cardinal ligament (C), which will connect the retroischial space with the perivesical (PVS) space. P, Cut edge of the pubic bone.

 Mickey M. Karram
Mickey M. Karram