Applied anatomy of the shoulder
Introduction
The main function of the joints of the shoulder girdle (Fig. 1) is to move the arm and hand into almost any position in relation to the body. As a consequence the shoulder joint is highly mobile, where stability takes second place to mobility, as is evident from the shape of the osseous structures: a large humeral head lying on an almost flat scapular surface. Stability is provided mainly by ligaments, tendons and muscles; the bones and capsule are of secondary importance.
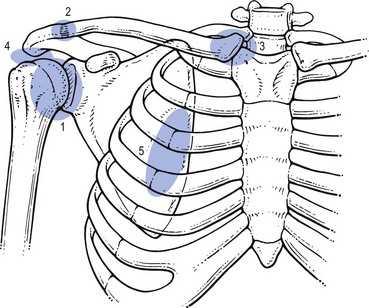
Fig 1 A global view of all five joints of the shoulder girdle: 1, glenohumeral joint; 2, acromioclavicular joint; 3, sternoclavicular joint; 4, subacromial joint or subacromial gliding mechanism; 5, scapulothoracic gliding mechanism.
The function of the shoulder girdle requires an optimal and integrated motion of several joints. In fact five ‘joints’ of importance to ‘shoulder’ function can be distinguished:1
• The acromioclavicular joint (2)
• The sternoclavicular joint (3)
• The subacromial joint or subacromial gliding mechanism (4): the space between the coracoacromial roof and the humeral head, including both tubercles. This is the location of the deep portion of the subdeltoid bursa
• The scapulothoracic gliding mechanism (5): this functional joint is formed by the anterior aspect of the scapula gliding on the posterior thoracic wall.
Optimal mobility also requires an intact neurological and muscular system.
It is not our intention to give a complete anatomical review, which can be obtained from anatomy texts. Only those structures which are of specific clinical importance will be focused on.
Bones
Osseous structures of interest are the scapula, humerus and clavicle. Neither the vertebral column nor the thoracic cage is discussed here (see chapters on the anatomy of the cervical and thoracic spine).
Scapula
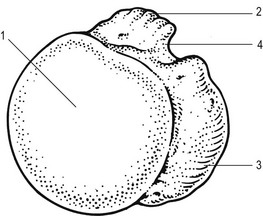
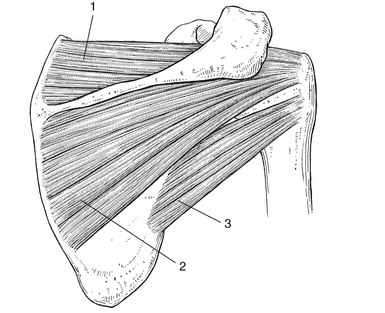
The scapula is a thin sheet of bone that functions mainly as a site of muscle attachment (Figs 2–3, see Putz, Figs. 286, 287, 288). Its medial border is parallel to the spine, the lateral and superior borders are oblique. It has a superior, a lateral and an inferior angle. The inferior angle corresponds to the interspinal level between the spinous processes of T7 and T8.
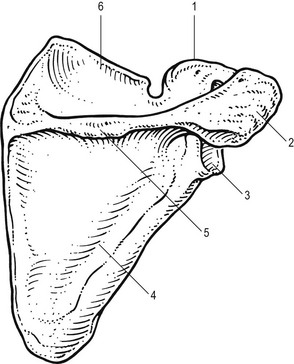
Fig 2 Posterior view of the scapula: 1, coracoid process; 2, acromion; 3, glenoid; 4, infraspinal fossa; 5, scapular spine; 6, supraspinal fossa.
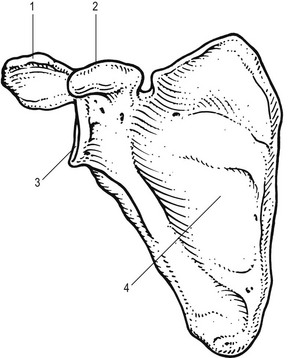
Fig 3 Anterior view of the scapula: 1, acromion; 2, coracoid process; 3, glenoid fossa; 4, anterior surface.
The scapula contains four processes: the acromion, the coracoid, the spine and the articular process (the glenoid).
The dorsum of the scapula is convex. It is divided by its spine into two fossae: the supraspinal and infraspinal fossa, containing the corresponding muscles. The scapular spine runs from the junction of the upper and middle third of the medial border, where it is rather flat, and corresponds to the level of the third thoracic spinous process. Laterally it becomes more prominent and meets the acromion at a right angle posteriorly. This angle is easily palpable and is one of the main bony landmarks at the shoulder. The acromion turns further anteriorly and covers part of the humeral head.
The coracoid process is found at the anterior aspect of the scapula. The tip points outwards and is easily palpated in the lateral part of the subclavian fossa. Further down, on the anterior aspect of the scapula, is a large concavity which contains the subscapularis muscle.
At the lateral angle, just beyond the neck of the scapula, is the glenoid fossa. This has a rather shallow surface, which is directed anterolaterally and slightly cranially tilted. It is approximately one-quarter the size of the humeral head and this, plus its shallow concavity, makes the joint both very mobile and vulnerable to (sub)luxations.
The ventral surface of the scapula is flat and covered with the attachment of the subscapularis muscle, except for the medial border and inferior angle where the serratus anterior muscle is inserted.
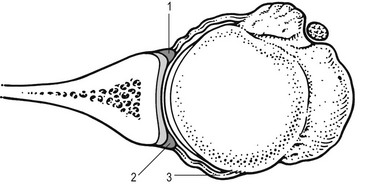
Humerus
The articular surface of the humeral head points in a medial, posterior and slightly caudal direction and is separated from the major and minor tuberosities by its anatomical neck.
When the arm is hanging down the side with its anterior aspect facing the body, the greater tuberosity lies laterally and the lesser tuberosity anteriorly. They are separated from each other by the bicipital sulcus (Fig. 4).
Clavicle
The clavicle joins the sternum to the acromion. At its medial end it has a forward convexity whereas its lateral end is rather more concave (see Putz, Fig. 284).
The joint capsules of both the sternoclavicular and the acromioclavicular joints are reinforced by several ligaments.
The clavicle has many muscular and ligamentous attachments. The insertion of the coracoclavicular ligament is of practical importance. It is found laterally on the inferior aspect of the clavicle, and just medial to it is the origin of the subclavius muscle.
The clavicle gives support to the shoulder girdle by acting as a strut between scapula and sternum. Due to its S-shape, the outer end describes a much larger rotation during arm elevation than its inner end. Therefore, lesions of the acromioclavicular joint ligaments are more frequent than are lesions of the sternoclavicular joint ligaments.
Joints and intracapsular ligaments
Glenohumeral joint
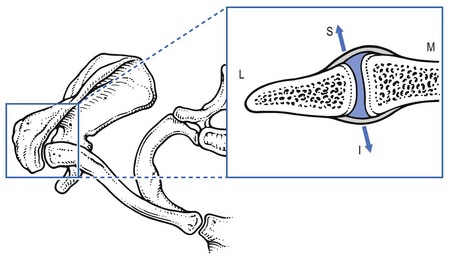
The glenohumeral joint (Fig. 5) is a ball-and-socket between humeral head and glenoid fossa. There is a remarkable geometrical relationship between glenoid and head which is responsible for the considerable mobility of the joint but is also an important predisposing factor to glenohumeral instability. First, the large spherical head of the humerus articulates against the small shallow glenoid fossa of the scapula (only 25–30% of the humeral head is covered by the glenoid surface). Second, the bony surfaces of the joint are largely incongruent (flat glenoid and round humerus). However, the congruence is greatly restored by the difference in cartilage thickness: glenoid cartilage is found to be the thickest at the periphery and thinnest centrally, whereas humeral articular cartilage is thickest centrally and thinnest peripherally. This leads to a uniform contact between humeral head and glenoid surface throughout shoulder motion.
The labrum is a fibrous structure that forms a ring around the periphery of the glenoid (see Putz, Fig. 298). It acts as an anchor point for the capsuloligamentous structures and for the long head of the biceps. It further contributes to stability of the joint by increasing the depth of the glenoid socket, enlarging the surface area and acting as a load-bearing structure for the humeral head.
The synovial membrane of the joint capsule is mainly attached to the labrum, covering its inner surface, and at the anatomical neck of the humerus. It forms a sleeve around the intra-articular and inter-tubercular part of the long tendon of the biceps.
The fibrous portion of the capsule is very lax and has several recesses, depending on the position of the arm. At its caudal end it forms the axillary recess, which allows normal elevation of the arm. Very often adhesions form here.
The joint capsule is large, loose and redundant: the capacity of the glenohumeral joint capsule is larger than that of the humeral head to allow full and free range of motion of the shoulder.
At the anterior portion of the capsule three local reinforcements are present: the superior, medial and inferior glenohumeral ligaments (Fig. 6). These contribute, together with the subscapularis, supraspinatus, infraspinatus and teres minor muscles, to the stability of the joint.
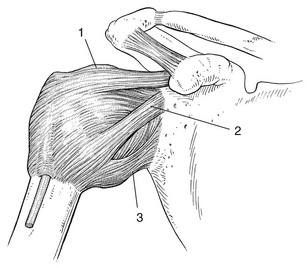
Fig 6 The glenohumeral joint capsule and ligaments: superior (1), medial (2) and inferior (3) glenohumeral ligaments.
The supraspinatus, infraspinatus, teres minor and subscapularis tendons reinforce the superior, posterior and anterior capsule. By virtue of the blending of their tendons with the glenohumeral capsule and ligaments, selective contraction of the cuff muscles can adjust the tension in these structures, producing ‘dynamic’ ligaments.
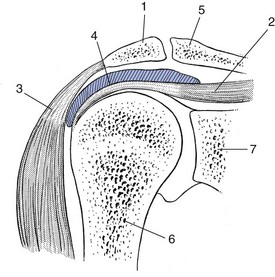
Subacromial space
The suprahumeral gliding mechanism consists of the coracoacromial arch (see below) on one side and the proximal part of the humerus, covered by the rotator cuff and the biceps tendon on the other. Both parts are separated by the subacromial bursa that acts as a joint space (Fig. 7). Investigators point to the importance of contact and load transfer between the rotator cuff and the coracoacromial arch in the function of the normal shoulder. Normally there is no communication between the bursa and the glenohumeral joint space but it may be established by rupture of the rotator cuff.
Acromioclavicular joint
The acromioclavicular joint (Fig. 8) is the only articulation between the clavicle and the scapula. It contains a disc which usually has a large perforation in its centre. The capsule is thicker on its superior, anterior and posterior surfaces than on the inferior surface. The anteroposterior stability of the acromioclavicular joint is controlled by the acromioclavicular ligaments and the vertical stability is controlled by coracoclavicular ligaments (conoid and trapezoid).
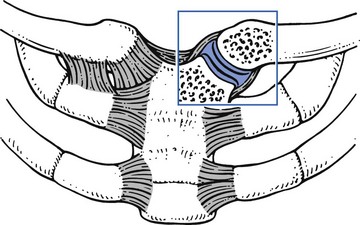
Sternoclavicular joint
The only osseous connection between the skeleton of the trunk and the upper limb is formed by the clavicle. Its medial end lies in contact with the superolateral angle of the sternal manubrium and with the medial part of the cartilage of the first rib to form the sternoclavicular joint (Fig. 9, see Putz, Fig. 285). In both the vertical and anteroposterior dimensions, the clavicular portion is larger than the opposing manubrium and extends superiorly and posteriorly relative to the sternum. The prominence of the clavicle enables its palpation. The sternoclavicular joint is mobile along all axes and almost every movement of the scapula and the arm is associated with some movement at this joint.
The capsule of the joint is thin at its inferior aspect but is reinforced anteriorly by the anterior sternoclavicular ligament, posteriorly by the posterior sternoclavicular ligament and cranially by the interclavicular ligament. The latter courses further above the sternum, to which it is firmly attached. Just lateral to the inferior part of the capsule is the costoclavicular ligament. This ligament connects the medial end of the clavicle to the cartilage of the first rib.
An intra-articular meniscus, firmly attached at its circumference to the joint capsule, to the clavicle and to the cartilage of the first rib, divides the joint into two separate cavities.
Behind the left joint is the common carotid artery, behind the right joint the innominate (brachiocephalic) vein. Both structures must be kept in mind when infiltrating on either side.
Scapulothoracic gliding mechanism
The serratus anterior muscle and the subscapularis are interposed between the scapula and the posterior thorax. The scapula is normally able to rotate, glide and tilt on the thorax. This mobility is an absolute necessity for normal function of the shoulder joint. Disorders of one of those structures, as in irregularity of the posterior thoracic wall, can result in pain on movements of the arm or scapula.
Extracapsular ligaments (Fig. 10, see Putz, Fig. 285)
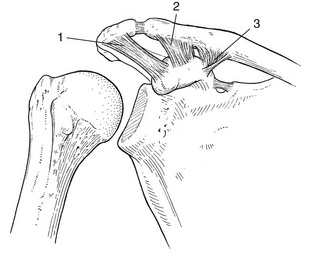
Fig 10 The extracapsular ligaments: 1, coracoacromial ligament; 2, trapezoid ligament; 3, conoid ligament.
Coracoacromial ligament
The coracoacromial ligament originates from the lateral aspect of the coracoid process and runs laterally and upwards to the tip of the acromion. It forms, together with the acromion and outer end of the clavicle, the coracoacromial roof.
The coracoacromial arch provides a strong ceiling for the shoulder joint, along which the cuff tendons must glide during all shoulder movements. Passage of the proximal humerus and its cuff tendons under this roof is facilitated by the gliding surfaces of the subacromial bursa. Because there is normally no gap between the cuff and the roof, the slightest amount of superior translation may compress the cuff tendons and/or the bursa between the humeral head and the arch (Fig. 10, see Putz, Fig. 295). Changes in the coracoacromial arch have been described in association with cuff disorders along with variations of acromial shape. Classically three types of acromion morphology are described: flat, curved and hooked. There seems to be a relationship between the presence of a hooked acromion and the prevalence of cuff lesions, although a hooked acromion and a cuff defect can both be merely the consequences of age.
Coracoclavicular ligaments
The trapezoid ligament originates superiorly on the coracoid process and inserts at the inferior–lateral aspect of the clavicle.
The triangular conoid ligament lies medial to the trapezoid ligament. Its origin is at the medial aspect of the superior surface of the coracoid process and it inserts at the conoid tubercle at the inferior clavicular aspect.
Both ligaments join together and form a half of a cone. They attach the scapula to the inferior outer side of the clavicle. Their structure enables the clavicle to rotate around its long axis on elevation of the arm. In this position the clavicular insertion of both ligaments points more or less anteriorly.
Costocoracoid fascia
Deep to the pectoralis major muscle lies a group of associated muscles and fascia: the clavipectoral fascia, the subclavius and pectoralis minor muscles (Fig. 11).
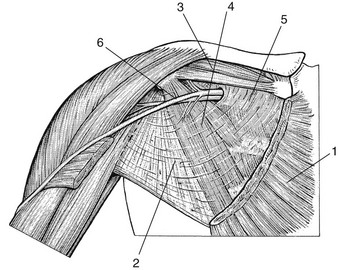
Fig 11 The costocoracoid fascia: 1, pectoralis major muscle; 2, clavipectoral fascia; 3, subclavius muscle; 4, pectoralis minor muscle; 5, costocoracoid fascia; 6, cephalic vein.
The costocoracoid fascia is that part of the clavipectoral fascia which is situated superomedial to the pectoralis minor muscle. A spontaneous loss of its normal elasticity may end in a contracture of this structure, causing limitation of elevation of the arm.
Bursae
The bursae are shown in Figures 12–13, see Putz, Fig. 295.
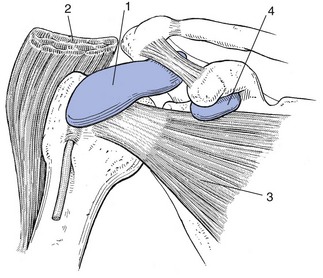
Fig 12 Anterior view of the bursae of the shoulder: 1, subdeltoid bursa; 2, deltoid muscle; 3, subscapularis muscle; 4, subcoracoid bursa.
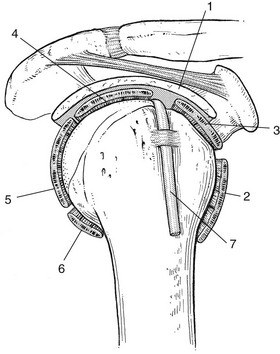
Fig 13 Lateral view of the subdeltoid bursa of the shoulder: 1, subdeltoid bursa; 2, teres major muscle; 3, subscapularis muscle; 4, supraspinatus muscle; 5, infraspinatus muscle; 6, teres minor muscle; 7, long head of biceps.
Subacromial–subdeltoid bursa
It is important to realize that there is only one bursa here. However, for clinical reasons two portions may be distinguished: a deep, subacromial part and a more superficial one. The former cannot be palpated, the latter is within a finger’s reach.
A good idea of the anatomical localization of this bursa is obtained if the palm of the contralateral hand is put on top of the shoulder. The metacarpophalangeal joints must lie contiguous with the lateral acromial rim. The area covered by the palm overlies the deep subacromial portion of the bursa, the area covered by the fingers, and delineates the superficial (subdeltoid) part of it.
The subacromial–subdeltoid bursa is normally only a potential ‘space’: two serosal surfaces in contact with each other, one on the surface of the cuff, the other on the undersurface of the coracoacromial arch (subacromial part) and the undersurface of the deltoid muscle (subdeltoid part). It normally produces a small amount of fluid which acts as a lubricant.
The bursa permits the two layers to glide in relation to each other and so can, to a certain extent, be considered as the synovial portion of the ‘subacromial joint’, an extension of the glenohumeral joint. Inflamed, the bursa becomes compromised by oedema and adhesions and may cause considerable pain and functional disturbance.
Subcoracoid bursa
Another clinically important bursa is the subscapularis bursa, which develops between the upper portion of the subscapularis tendon, the neck of the scapula and the base of the coracoid process (see Standring, Fig. 46.14A). The bursa is covered by the pectoralis major muscle. Bursitis here can give rise to an isolated limitation of passive lateral rotation. Since this movement stretches the muscle, it will painfully pinch the inflamed subcoracoid bursa, provoking a spasm of the pectoralis major.
Shoulder movements
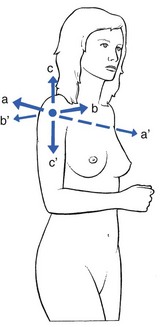
The glenohumeral joint is the most mobile joint of the human body. It can move around three different axes, all transversing the head of the humerus (Fig. 14):
• a–a′ – Transverse axis: this is a horizontal axis coursing from the left to the right shoulder. Anterior and posterior directed movements around it are flexion and extension.
• b–b′ – Sagittal axis: this horizontal axis lies in antero-posterior sense through the head of the humerus. Movement of the arm around this axis is named adduction (the arm moves towards the body) and abduction (away from the body).
• c–c′ – Vertical axis: with the right arm hanging in neutral position (radial side pointing anteriorly and elbow bent to 90°), outward movement of the arm around a vertical axis, bringing the palm of the hand anteriorly, is lateral rotation. The movement in the opposite direction is medial rotation. If the arm is first abducted to 90°, movement around the vertical axis, which brings the arm anteriorly and posteriorly, is named horizontal adduction and horizontal extension.
When the patient actively elevates the arm, the initial movement takes place at the glenohumeral joint. Later the scapula rotates synchronously. Clinically this is easily checked by palpating the inferior scapular angle during elevation. Wallace2 states that both movements take place in a ratio of about 2 : 1; that means for every 2° of movement at the glenohumeral joint there exists 1° of scapular rotation. These simultaneous movements are known as the scapulothoracic or scapulohumeral rhythm.
Mobility of the glenohumeral joint is usually tested in three directions: abduction, medial rotation and lateral rotation.
Abduction is movement in a frontal plane between a mobile humerus and a stabilized scapula. Medial and lateral rotation is assessed with the arm hanging in the neutral position. The term elevation indicates the movement of the shoulder complex (glenohumeral joints and shoulder girdle) in a frontal plane. Normally the arm can move through an angle of approximately 0° to 180° in elevation; the normal range for the glenohumeral joint is about 90° of abduction and the same for medial and lateral rotation.
The most important function of the shoulder – arm elevation – has been extensively studied, in particular the relationship and contribution of the glenohumeral and scapulothoracic joints and the ‘scapulothoracic’ rhythm has been determined. During full elevation of 180° only 90° takes place at the glenohumeral joint. The remaining half is the consequence of scapular rotation, clavicular movement and, finally, adduction of the humerus which is only possible when the scapula has been fully rotated.
Muscles and tendons
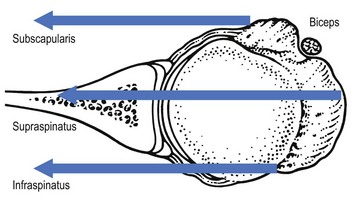
The clinically important contractile structures of the shoulder joint are those whose tendons form the rotator cuff: the supraspinatus, infraspinatus, subscapularis and, of less importance, the teres minor.
The adductors are those muscles which act below the sagittal axis, and the abductors are those acting above (Fig. 15). Medial rotators act in front of the vertical axis, lateral ones behind it.
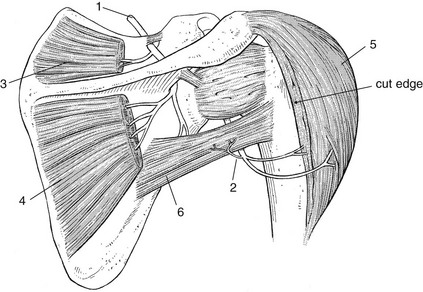
The origins and insertions of the muscles are shown in Figure 16.
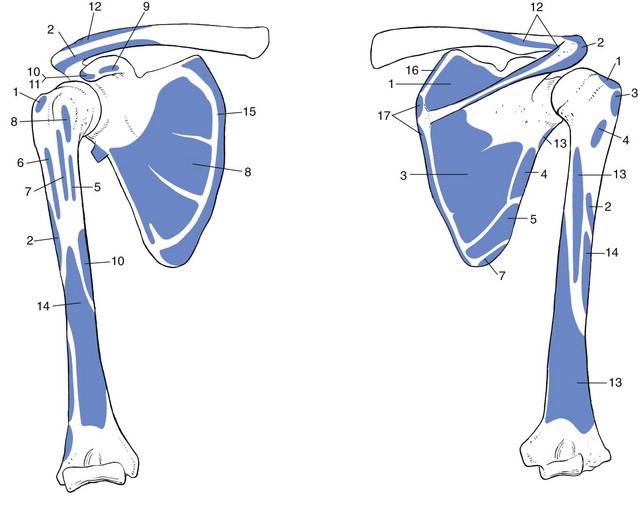
Fig 16 Muscle origins and insertions: 1, supraspinatus; 2, deltoid; 3, infraspinatus; 4, teres minor; 5, teres major; 6, pectoralis major; 7, latissimus dorsi; 8, subscapularis; 9, pectoralis minor; 10, coracobrachialis; 11, short head of biceps; 12, trapezius; 13, triceps brachii; 14, brachialis; 15, serratus anterior; 16, levator scapulae; 17, rhomboid.
Adduction
Adduction of the arm is performed by four different muscles: teres minor and major, the pectoralis major and latissimus dorsi (see Fig. 18). The first is also a lateral rotator, while the latter three are medial rotators.
The teres minor arises at the lower outer rim of the scapula, just above the origin of the teres major muscles and inserts on the major tubercle, just distal to the insertion of the infraspinatus muscle.
The teres major runs from the lower scapular angle towards the anterior aspect of the humerus, where it inserts on the minor tubercular crest, together with the latissimus dorsi muscle.
The triangular space at the posterior aspect of the shoulder between both teres muscles is divided by the long head of the triceps muscle into a quadrilateral space laterally and a triangular space medially (see Putz, Fig. 338).
The latissimus dorsi muscle originates partly from the spinous processes of the lower dorsal vertebrae, partly from the lumbar vertebrae, partly from the iliac crest and sometimes from the lower ribs. It runs outwards and upwards in the direction of the lesser tubercular crest, where it inserts just lateral to the insertion of the teres major muscle.
The pectoralis major muscle originates from the medial end of the clavicle, the sternum, the cartilage of the second to the sixth rib and the uppermost part of the rectus abdominis muscle. The upper fibres have a slightly downward course; the lower fibres run in a craniolateral direction. It inserts on the crest of the greater tuberosity.
Table 1 summarizes the adductors.
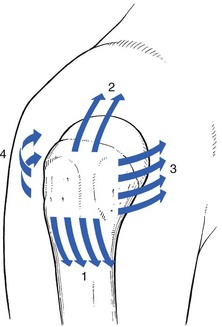
Abduction
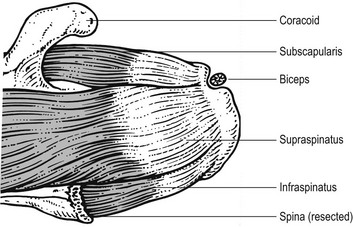
The supraspinatus muscle together with the deltoid is mainly responsible for this movement. Clinical differentiation of the two structures is made by testing resisted movement of horizontal adduction and horizontal extension, which are secondary functions of the deltoid muscle.
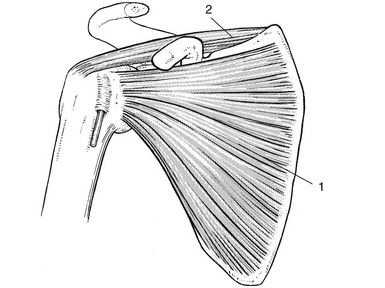
The supraspinatus, which originates in the supraspinal fossa, passes laterally, underneath the coracoacromial roof and inserts at the greater tubercle of the humerus (Fig. 17). The tendon and the tenoperiosteal junction are about 1 cm in width. On palpation it feels like a rather flat cord with a typical tendinous consistency. The muscle plays a particularly important role in the initiation of abduction. When this tendon is completely ruptured the patient can no longer lift the arm actively and must make a swinging movement of the whole body in order to start the movement. Once the arm has moved through 30° the deltoid muscle takes over and carries out further abduction.
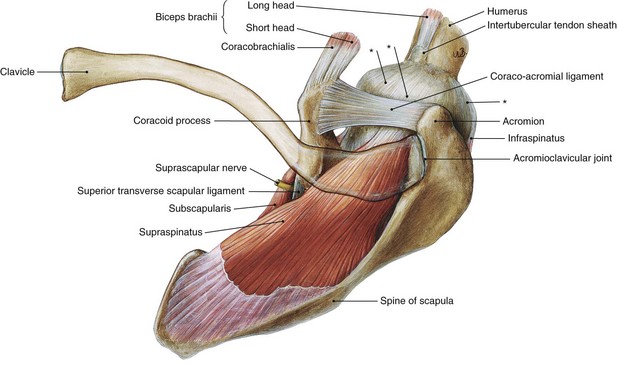
Fig 17 Supraspinatus muscle from above and anterior. *Capsule of the joint. From Putz, Sobotta – Atlas of Human Anatomy, 14th edn. Urban & Fischer/Elsevier, Munich, 2008 with permission.
The deltoid has three different parts: the clavicular, the acromial and the scapular spinal. In addition to the muscle’s overall effect in abduction, its different parts each have other functions of their own (see Putz, Fig. 345). The clavicular component helps horizontal adduction of the arm and the scapular spinal component assists horizontal extension movement. With the arm in neutral position, the former helps flexion, the latter extension.
Table 2 summarizes the abductors.
Medial rotation
Three medial rotators have been discussed already: teres major, latissimus dorsi and pectoralis major (Fig. 18, see Putz, Fig. 337). All of these are also adductors. The fourth medial rotator is the subscapularis (Figs 18, 19). Its origin lies in the subscapular fossa, and the insertion in the minor tuberosity and towards the proximal extent of the minor tubercular crest. The tenoperiosteal insertion has a width of about 3 cm, is very thin and cannot be distinguished on palpation. Location of the insertion depends entirely on bony landmarks, i.e. the minor humeral tubercle.
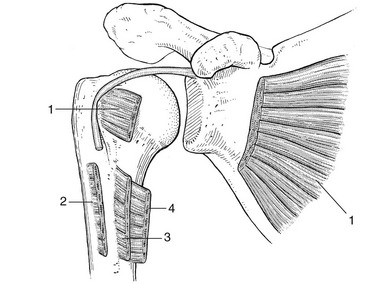
Fig 18 Muscles used in medial rotation: 1, subscapularis; 2, pectoralis major; 3, latissimus dorsi; 4, teres major.
On abduction of the arm, the upper fibres pass underneath the acromial roof. Therefore, a momentary impingement of a lesion in this location can happen and produce a painful arc.
Horizontal adduction brings the lower half of the subscapularis insertion in contact with the coracoid process, and a lesion in this portion provokes pain on this movement.
Table 3 summarizes the medial rotators.
Lateral rotation
This movement is performed mainly by the infraspinatus, teres minor being only a weak lateral rotator. The infraspinatus originates in the infraspinal fossa and passes laterally underneath the acromion. It inserts on the greater tuberosity over about 2 cm. The upper fibres are in very close relationship with the insertion of the supraspinatus (Fig. 20, see Gosling, Fig. 3.64). On palpation the insertion is flatter and has a harder consistency than the insertion of the supraspinatus tendon.
The lateral rotators are summarized in Table 4.
Flexion of the elbow
Although this movement is performed by other structures as well, it is the tendon of the long head of the biceps that is the most important here (Table 5, see Putz, Fig. 346). Arriving from the supraglenoid tubercle it is directed downward towards the bicipital groove, where it lies underneath a transverse ligament. Part of it is intra-articular, where it is surrounded by a synovial membrane. On contraction of the biceps the tendon itself does not move. It plays an important role in the stabilization of the humeral head in the glenoid fossa during powerful flexion of the elbow and supination of the forearm.
Table 5
| Muscle | Nerve | Spinal nerve root |
| Biceps brachii | Musculocutaneous | C5, C6 |
The tendon of the short head of the biceps, originating from the coracoid process, seldom causes any problem.
The other flexor muscles are described in the online chapter Applied anatomy of the elbow.
Extension of the elbow
Extension of the elbow is performed by the triceps brachii (Table 6, see Putz, Fig. 298). The long head originates from the lower margin of the glenoid. Triceps lesions at the shoulder are extremely rare. Because the humeral head is pulled up towards the coracoacromial roof on resisted extension of the elbow, it can provoke an impingement of a lesion sited between the head of the humerus and the coraco-acromial arc. Therefore, if resisted extension of the elbow provokes pain at the shoulder, it is usually considered as analogous to a painful arc.
Flexion
The pectoralis major, biceps brachii, subscapularis and deltoid muscles, which are flexors, have already been discussed. The only other structure that can provoke pain on resisted flexion of the arm is the coracobrachialis. Its origin is at the coracoid process, together with the short head of the biceps, and it inserts at the medial aspect of the midportion of the upper arm, below the minor tubercular crest.
The flexors are summarized in Table 7.
Table 7
| Muscle | Nerve | Spinal nerve root |
| Coracobrachialis | Musculocutaneous | C5, C6 |
| Pectoralis major | Pectoral | C5–C8 |
| Deltoid (anterior portion) | Axillary | C5 (C6) |
| Subscapularis | Subscapular | C5–C8 |
| Biceps brachii | Musculocutaneous | C5, C6 |
The anatomy of other muscles which are mainly associated with movements of the scapula – such as the subclavius, levator scapulae and others – are discussed in the online chapter Applied anatomy of the thorax and abdomen.
Rotator cuff
Although the rotator cuff muscles have been discussed individually, some remarks about the cuff as a whole are in order.
The rotator cuff is a complex of four muscles that arise from the scapula and attach to the tuberosities of the humerus. Although the muscles are separate superficially, in their deeper region they merge with each other, with the capsule underneath and with the tendon of the long head of the biceps.
Their intimate relationship with each other and with the capsule, together with their unique localization, provides the rotator muscles with some particular functions:
• First: the rotator cuff muscles ‘rotate’ the humerus with respect to the scapula – a function that has been discussed earlier. However, the insertion of these tendons as a continuous cuff around the humeral head permits the cuff muscles to provide an infinite variety of movements to rotate the humerus.
• Second: by contracting together, the rotator cuff muscles and the biceps compress the humeral head into the glenoid fossa, locking it into position and providing a secure scapulohumeral link for upper extremity function – known as ‘concavity compression’ (Fig. 21).
• Third: they provide muscle balance. In the shoulder, no fixed axis exists and, in a specified position, activation of one muscle will create a set of different rotational movements. In order to produce movement in one direction, the other movements initiated by the contracting muscle must be neutralized by other muscles. The rotator cuff muscles are critical elements of this shoulder muscle balance equation: by contracting selectively, they resist displacing forces resulting from contraction of the principal shoulder movers (deltoid, pectoralis major, latissimus dorsi).
• Fourth: they have an important role in capsular stability of the joint. By virtue of the blending of their tendons with the glenohumeral capsule and ligaments, selective contraction of the cuff muscles can adjust the tension in these structures, so producing ‘dynamic’ ligaments (see Fig. 22).
Nerves and blood vessels
Suprascapular nerve
This nerve is derived from the brachial plexus. It contains motor fibres of the C5 (C6) root and passes in the scapular incisura, under the transverse scapular ligament (Fig. 23), whereas the suprascapular artery lies above the transverse ligament. It innervates the supraspinatus and infraspinatus muscles.
Axillary nerve
The axillary nerve (Figs 23, 24) contains both motor and sensory fibres from C5 (C6). Originating on the brachial plexus anteriorly, it passes dorsally via the lateral axillary foramen. Its close contact with the humeral neck often results in injury in the event of a dislocation.
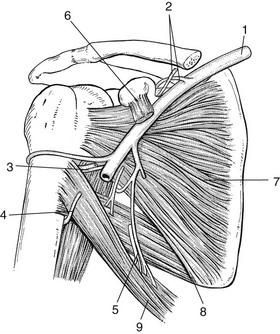
Fig 24 The anterior scapulohumeral region; 1, subclavian artery; 2, suprascapular artery and nerve; 3, axillary nerve; 4, radial nerve; 5, subscapularis nerve; 6, pectoralis minor muscle; 7, subscapularis muscle; 8, teres major muscle; 9, latissimus dorsi muscle.
It gives a branch to the teres minor muscle and ends in the deltoid muscle. The terminal branch is the lateral superior brachial cutaneous nerve, which innervates the upper and outer aspect of the skin over the deltoid.
Subclavian artery and vein
The subclavian blood vessels are of particular importance since their compression can give rise to the subclavian steal syndrome or may play a role in the thoracic outlet syndrome. The vessels lie between the first rib and the clavicle, medially to the brachial plexus, and are separated by the scalenus anterior muscle.
O’Brien, M. Aids to the Examination of the Peripheral Nervous System. London: Baillière Tindall; 1986.
Burns, W, Whipple, T. Anatomic relationships in the shoulder impingement syndrome. Clin Orthop Rel Res. 1933; 294:96–102.
Claessens, H. De pijnlijke Schoulder. Leiden: Stafleu’s Scientific Editing Company; 1967.
Clarys, J, Cabri, J, Vanderstappen, D. Functionele Anatomie. VUB-uitgaven; 1989.
Codman, E. Normal motions of the shoulder joint. In: The Shoulder. Boston: Thomas Todd; 1934:52.
Cooper, D, Arnoczky, S, O’Brien, S, Warren, R, CiCarlo, E, Allen, A. Anatomy, histology, and vascularity of the glenoid labrum. J Bone Joint Surg. 1992; 74A(1):46–52.
Cooper, D, O’Brien, S, Warren, R. Supporting layers of the glenohumeral joint. Clin Orthop Rel Res. 289, 1993. [144–144].
Fautrez J. Leidraad bij de studie van de stelselmatige ontleedkunde van de mens, vols I and II. In: Desoer L, editor. 1967.
Guyot, J. Atlas of Human Limb Joints, 2nd ed. Berlin: Springer; 1990.
Hoppenfeld, S. Physical Examination of the Spine and Extremities. Norwalk, Connecticut: Appleton-Century-Crofts; 1976.
Kaltsas, D. Comparative study of the properties of the shoulder joint capsule with those of other joint capsules. Clin Orthop Rel Res. 1983; 173:20–26.
Keating, J, Waterworth, P, Shaw-Dunn, J, Crossan, J. The relative strengths of the rotator cuff muscles. J Bone Joint Surg. 1993; 75B(1):137–140.
Kingma, M. Schouderpijn. Ned Tijdschr Geneeskd. 1986; 120(8):325–337.
Kumar, V, Satku, K, Balasubramanium, P. The role of the long head of biceps brachii in the stabilization of the head of the humerus. Clin Orthop Rel Res. 1989; 244:172–175.
Lipmann, K. Clinical Disorders of the Shoulder, 2nd ed. London: Churchill Livingstone; 1986.
Matsen F, Fu F, Hawkins R, eds. The Shoulder: A Balance of Mobility and Stability. Colorado: Vail, 1992.
McMinn, R, Hutchings, R. Atlas of Human Anatomy. London: Mosby; 1993.
Mink, A, Ter Veer, H, Vorselars, H. Extremiteiten: Functieonderzoek en Manuele Therapie. Bohn, Schelteme Holkema Utrecht/ Antwerpen; 1990.
Netter, F. The Ciba Collection of Medical Illustrations, vol 8, Musculoskeletal System. Summit, New Jersey: Ciba–Geigy Corporation; 1987.
Nobuhara, K. Contracture of the shoulder. Clin Orthop Rel Res. 1990; 254:105–110.
Reilly, J, Nicholas, J. The chronically inflamed bursa. Clin Sports Med. 1987; 6(2):345–370.
Saha, A. The classic mechanism of shoulder movements and a plea for the recognition of ‘zero position’ of the glenohumeral joint. Clin Orthop Rel Res. 1983; 173:3–10.
Sarrafian, S. Gross and functional anatomy of the shoulder. Clin Orthop Rel Res. 1983; 173:11–19.
Sobotta, J, Becher, H. Atlas der Anatomie des Menschen. Munich: Urban & Schwarzenberg; 1967.
Vleeming, A, Stoeckart, R, Klein, H, Volkers, A. Misunderstandings concerning bursae of the shoulder. Ned Tijdschr Geneeskd. 1987; 131(41):1807–1809.